Table of Contents
ToggleOPPORTUNISTIC INFECTIONS IN HIV/AIDS
Opportunistic infections (OIs) are infections affecting HIV patients with weakened immunity, indicated by a white blood cell count below 200 cells/cm³ (14%).
- Advanced HIV infection makes individuals vulnerable to opportunistic infections or malignancies. These infections exploit the weakened immune system.
- Childhood acquisition of OIs and HIV often occurs from infected mothers.
- Women living with HIV are more prone to co-infections with opportunistic pathogens, increasing the risk of transmission to their infants.
- Adolescents with HIV, including long-time survivors of perinatal infection, are increasingly common. Treatment guidelines also apply to youth living with HIV who have not yet completed pubertal development.
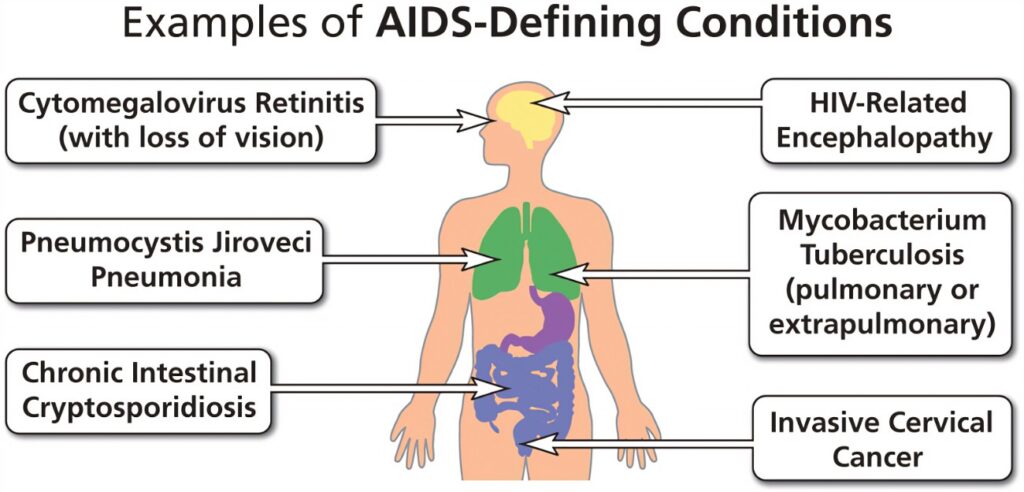
Examples of Opportunistic Infections
Category | Infection | Explanation |
Bacterial OIs | Pneumococcal pneumonia | A bacterial infection causing severe respiratory illness, commonly affecting HIV patients due to weakened immunity. |
Pulmonary tuberculosis | A serious infectious disease that primarily affects the lungs, prevalent in HIV patients due to compromised immune defenses. | |
Salmonellosis | An infection caused by Salmonella bacteria, leading to severe gastrointestinal symptoms, more common in immunocompromised individuals. | |
Extra-pulmonary tuberculosis | Tuberculosis infection occurring outside the lungs, such as in the lymph nodes or bones, often seen in advanced HIV cases. | |
Viral OIs | Herpes zoster | Also known as shingles, caused by the reactivation of the chickenpox virus, leading to painful skin rashes in HIV patients. |
Recurrent/disseminated viral herpes simplex | Chronic or widespread herpes simplex virus infections, more severe and frequent in individuals with HIV. | |
Parasitic OIs | Pneumocystis carinii pneumonia | A fungal infection (previously classified as parasitic) causing severe lung disease, a common and life-threatening infection in HIV patients. |
Toxoplasmosis | An infection caused by the Toxoplasma gondii parasite, leading to severe neurological issues in immunocompromised individuals like those with HIV. | |
Fungal OIs | Cryptosporidium | A parasitic infection causing severe diarrhea, often found in HIV patients due to their weakened immune systems. |
Oro-pharyngeal candida | A fungal infection in the mouth and throat, also known as thrush, common in HIV patients. | |
Candida Esophagitis | A severe fungal infection of the esophagus, causing difficulty in swallowing and chest pain, prevalent in advanced HIV cases. | |
Histoplasmosis | A fungal infection caused by inhaling Histoplasma spores, leading to lung disease, more severe in immunocompromised patients. | |
Coccidioidomycosis | A fungal disease also known as Valley fever, causing respiratory issues, especially severe in those with weakened immune systems. | |
Cryptococcal meningitis | A life-threatening fungal infection of the brain and spinal cord, common in advanced HIV/AIDS patients. | |
Opportunistic Cancers | Invasive cervical cancer | Cancer caused by the human papillomavirus (HPV), more prevalent and aggressive in women with HIV. |
Kaposi sarcoma | A cancer caused by human herpesvirus 8 (HHV-8), leading to lesions on the skin and other organs, commonly seen in HIV patients. | |
Non-Hodgkin lymphoma | A type of cancer affecting the lymphatic system, more common and aggressive in individuals with HIV. | |
Other OIs | Oral hairy leukoplakia | A condition characterized by white patches on the tongue, caused by Epstein-Barr virus, indicating immunosuppression in HIV patients. |
Leukoencephalopathy | A rare, progressive viral disease affecting the white matter of the brain, often seen in severe immunocompromised states like advanced HIV. | |
Progressive multifocal leukoencephalopathy | A demyelinating disease of the central nervous system caused by the JC virus, highly fatal in HIV patients. |
Causes of Opportunistic Infections:
- Poor adherence to treatment
- Presence of other diseases (e.g., juvenile diabetes mellitus)
- Delay in identification of the infection
- High viral load
- Poor nutrition
- Exposure to opportunistic infectious agents
- Ingestion of substances contaminated with opportunistic infectious agents
- Missing out on immunization programs
- Poor hygiene
- Poor sanitation
- Poor ventilation
Prevention of Opportunistic Infections:
- Avoidance of contact with the disease agents
- Proper treatment of other underlying diseases
- Adherence to HIV drug treatment
- Immunization of children against killer diseases
- Ensuring that children consume well-cooked food and boiled water
- Early identification and treatment of opportunistic diseases
- Health education of the family and infected child about opportunistic infections
HEPATITIS B
Hepatitis B is a chronic liver infection characterized by inflammation of hepatocytes caused by the hepatitis B virus.
Transmission:
- High: Blood
- Moderate: Semen, Urine, Serum, Wound exudate, Vaginal fluid
- Low/Not Detectable: Saliva, Feces, Sweat, Tears, Breast milk
Stages of Hepatitis B:
- Immune Tolerance: Represents the incubation period, lasting approximately 2-4 weeks in healthy adults, and often decades in newborns.
- Immune Active/Immune Clearance: Inflammatory reaction occurs with active viral replication. Duration varies; for acute infection, approximately 3-4 weeks; for chronic infection, up to 10 years.
- Inactive Chronic Infection: Host targets infected hepatocytes and HBV, with low or no measurable viral replication in serum. Anti-HBe can be detected.
- Chronic Disease: Chronic HBeAg-negative disease may emerge.
- Recovery: Virus undetectable in blood, antibodies to viral antigens produced.
Clinical Features:
Symptoms can be symptomatic or asymptomatic:
- Weakness, malaise, low-grade fever
- Nausea, loss of appetite, vomiting
- Pain or tenderness over right upper abdomen
- Jaundice, dark urine, severe pruritus
- Enlarged liver
- Complications: liver cirrhosis, hepatocarcinoma
Investigations:
- Hepatitis B surface antigen positive for >6 months
- Hepatitis B core antibody: Negative IgM and Positive IgG to exclude acute hepatitis B infection
- Liver tests, repeated at 6 months
- HBeAg (can be positive or negative)
- HBV DNA if available
- HIV serology
- APRI (AST to Platelets Ratio Index): a marker for fibrosis
- Alpha fetoprotein at 6 months
- Abdominal ultrasound at 4-6 months
Management:
General Principles:
- Screen for HIV and refer if positive.
- Refer to a regional hospital for specialist management if HIV is negative.
- Antiviral treatment is given to prevent complications and usually for life.
- Patients with chronic hepatitis B need periodic monitoring and follow-up for life.
- Periodic screening for hepatocarcinoma with alfa fetoprotein and abdominal ultrasound once a year.
Treatment with Antivirals:
- Treat with antivirals based on specific criteria.
First-line antivirals:
- Adults and children >12 years or >35 kg: tenofovir 300 mg once a day
- Child 2-11 years (>10 kg): Entecavir 0.02 mg/kg
Health Education:
- Management is lifelong.
- Bed rest is recommended.
- Avoid alcohol as it worsens the disease.
- Immunization of household contacts.
- Do not share items that the patient puts in the mouth (e.g. toothbrushes, cutlery, razor blades).