Table of Contents
ToggleOphthalmology
Ophthalmology is a branch of medicine that deals with the diagnosis and treatment of diseases and disorders related to the eyes.
Definition of Terms
- Ophthalmologist: A medical or osteopathic doctor specializing in eye and vision care. Ophthalmologists diagnose and treat all eye diseases, perform eye surgery, and prescribe and fit eyeglasses and contact lenses to correct vision problems. Many ophthalmologists are also involved in scientific research on the causes and cures for eye diseases and vision disorders.
- Optometrist: A healthcare professional providing primary vision care ranging from sight testing and correction to the diagnosis, treatment, and management of vision changes. An optometrist is not a medical doctor.
- Optician: A technician trained to design, verify, and fit eyeglass lenses and frames, contact lenses, and other devices to correct eyesight.
- Ophthalmic Nurse: A nursing professional focused on assessing and treating patients with various eye diseases and injuries.
Role of Ophthalmic Nurses
- Provide first aid treatment in cases of eye injuries and emergencies.
- Perform preliminary physical examinations, such as blood tests, to detect possible underlying illnesses that could contribute to eye problems (e.g., hypertension).
- Conduct initial screenings on patients.
- Collect medical histories.
- Assist in eye examinations.
- Offer tips and advice to help patients manage eye pain and other symptoms.
- Demonstrate how to administer medication.
- Educate patients on the treatment of ocular conditions.
- Prepare patients for surgery and assist during operations.
- Provide after-surgery care for patients.
- Conduct various eye tests and procedures.

Ophthalmic Emergencies and Urgent Cases
Emergencies requiring immediate medical attention include:
Sudden vision loss:
- Central retinal artery occlusion: Blockage of the artery supplying the central retina.
- Central retinal vein occlusion: Blockage of the vein draining blood from the retina.
- Giant cell arteritis: Inflammation of the arteries in the head, including those supplying the eye.
- Retinal detachment: Separation of the retina from the back of the eye, especially if the macula (central part of the retina) is still attached.
Primary acute glaucoma: Rapid increase in pressure within the eye, causing pain, blurred vision, and halos around lights.
Trauma:
- Penetrating or perforating injuries: Objects entering the eye.
- Chemical burns: Exposure of the eye to chemicals.
Orbital cellulitis: Infection of the tissues surrounding the eye.
Urgent cases requiring prompt medical attention, but not considered true emergencies:
- Corneal ulcer: Open sore on the cornea, causing pain, redness, and blurred vision.
- Vitreous hemorrhage: Bleeding into the vitreous humor (jelly-like substance filling the back of the eye), causing blurred vision or floaters.
- Acute dacryocystitis: Inflammation of the lacrimal sac (tear sac), causing pain, swelling, and redness.
- Optic nerve disorders: Conditions affecting the optic nerve, causing vision loss or other visual disturbances.
- Ocular tumors: Growths within the eye, which may affect vision or require treatment.
- Acute uveitis: Inflammation of the middle layer of the eye, causing pain, redness, and blurred vision.

EYE CARE
Eye care is characterized as the special attention given to the eyes to prevent complications.
Natural Cleansing: The production of tears and the blinking mechanism provide a natural cleansing process for the eyes (Harrison, 2006). When this process is interrupted, the eyes may need to be artificially cleansed to remove debris, prevent dryness, and ensure eyelid closure (Dawson, 2005).
Eye Cleansing: Eye cleansing can be performed alone or with eye swabbing, instilling eye medication, and applying eye padding/dressing/shield.
Indications for Eye Care:
- Children Undergoing Eye Surgery: Pre-operative and post-operative eye care is important to ensure the eye is clean, free from infection, and well-prepared for surgery. This care includes instilling prescribed eye drops, maintaining proper hygiene, and following specific instructions from the ophthalmologist.
- Children Whose Eyes Cannot Close Properly: Hydrocephalus, cerebral palsy, facial nerve palsy, and other conditions affecting eyelid closure,, where eyelid function may be compromised, maintaining eye moisture and cleanliness is essential to prevent corneal damage and infection.
- Unconscious, Sedated, or Muscle-Relaxed Children: These children cannot blink or close their eyes effectively, making them prone to dryness and exposure to keratitis. Regular eye care, including lubrication and protective measures, is necessary to prevent complications.
- Presence of Infection (e.g., Conjunctivitis/Neonatal Conjunctivitis): Eye infections require careful cleansing and medication administration to control and eradicate the infection. This prevents the spread of infection and promotes faster healing.
- Infants with Non-Infected Sticky Eye Due to Underlying Causes (e.g., Blocked Tear Ducts): Conditions like blocked tear ducts can cause sticky discharge. Regular eye cleaning helps keep the eye clear and reduces the risk of secondary infections.
- Immunosuppressed Children: These children are more susceptible to infections due to their weakened immune systems. Regular and prompt eye care helps prevent opportunistic infections and maintain eye health.
- Trauma: Eye injuries require prompt and careful cleaning to remove debris, prevent infection, and manage pain. Eye care post-trauma is crucial for recovery and to avoid further damage.
- Chronic Eye Conditions (e.g.,Dry Eye Syndrome): Conditions causing chronic dryness need regular lubrication to maintain comfort and prevent damage to the cornea and conjunctiva.
- Post-Chemotherapy/Radiation Therapy: Children undergoing cancer treatments may experience eye issues due to the side effects of therapy. Regular eye care can mitigate symptoms like dryness and irritation.
- Congenital Eye Disorders (e.g., Ptosis, Congenital Glaucoma): Children with congenital eye disorders may need regular eye care to manage symptoms, prevent complications, and support overall eye health.
- Post-Cataract Surgery: After cataract surgery, careful eye care is necessary to ensure proper healing, prevent infection, and manage any postoperative complications.
- Severe Allergies: Children with severe allergies may experience frequent eye irritation and discharge, necessitating regular cleaning and medication application.
- Exposure to Environmental Irritants: Children exposed to smoke, dust, or chemicals need regular eye cleaning to remove irritants and prevent damage.
Purpose of Performing Eye Care:
- Maintain Eye Cleanliness: Regular eye care helps keep the eyes clean, promoting comfort for the patient and reducing the risk of cross-infection, particularly in clinical settings.
- Prevent Eye Dryness: Various methods are employed to keep the eyes moist and comfortable. These include:
Methylcellulose Drops: Used for general lubrication.
Ointments: Provide longer-lasting moisture.
General Lubricants: Help maintain moisture balance.
Polyacrylamide Hydrogel Dressings: Effective for unconscious, sedated, or paralyzed children as they moisten and lubricate the eye area while maintaining eyelid closure.
Hypromellose Drops (Artificial Tears): Used to supplement natural tears and prevent dryness.
- Ensure Eyelid Closure: Using polyacrylamide hydrogel dressings like Geliperm® helps keep the eyelids closed, which is crucial for preventing exposure to keratitis in patients who cannot close their eyes naturally.
- Treat Existing Eye Infections: Proper eye care is essential for treating infections, involving cleaning the eye and administering appropriate medications to eradicate the infection and prevent its spread.
- Prepare for Medication Administration: Ensuring the eye is clean and free from debris before administering medications enhances the effectiveness of the treatment and reduces the risk of complications.
- Protect the Eye During Phototherapy: When using phototherapy light lamps, especially in newborns with jaundice, eye care measures are taken to protect the retina from potential damage caused by the light exposure.
- Support Healing Post-Surgery: After eye surgeries such as cataract removal, meticulous eye care supports the healing process, reduces the risk of infection, and helps manage post-operative discomfort.
- Manage Allergic Reactions: In cases of severe allergies, eye care involves cleaning and administering anti-allergy medications to reduce irritation and prevent secondary infections.
- Facilitate Proper Drainage: For conditions like blocked tear ducts, regular eye care helps in facilitating drainage and reducing discomfort and infection risk.
- Prevent Damage in Systemic Conditions: In children with systemic conditions like diabetes, regular eye care is vital to monitor and manage potential complications, thus preserving eye health.
- Educate Caregivers: Eye care is a tool for educating caregivers on proper eye care techniques, signs of complications, and the importance of maintaining eye hygiene ensures consistent and effective care for the child.
Purpose of Eye Medications:
Topical medication is the preferred route for treating eye diseases. Eye medications are delivered to:
- Treat infections.
- Provide intraocular treatment for diseases such as glaucoma.
- Prepare for and recover from surgical procedures.
- Dilate pupils for eye examinations and/or refraction.
- Provide lubrication.

Care of the Child Undergoing Eye Surgery:
The care involves pre-operative, intra-operative, and post-operative care.
Pre-operative Care:
Common conditions requiring surgical intervention include trauma, Cataracts, Foreign body eye, Congenital malformations, Glaucoma, Eye injuries, Astigmatism or strabismus, Sagging of the upper eyelid (ptosis) and detached retina. The ophthalmologist will determine the treatment and procedure, ranging from a simple incision to total removal of the eyeball (enucleation).
- Admission: The child will be admitted to a warm and clean bed in the pediatric surgical ward. The bed will have enough light to ensure a comfortable environment for the child and will be free from environmental dust to minimize the risk of infection.
- History taking: Take a detailed history of the child’s medical background, including any previous surgeries, allergies, or medical conditions, also inquire about any medications the child is currently taking.
- Physical examination. A thorough physical examination will be conducted and will assess the child’s overall health and identify any potential risks or concerns. The physical examination will include checking vital signs such as heart rate, blood pressure, and temperature and the child’s eyes will be examined to evaluate the specific condition requiring surgery and to ensure there are no additional eye health issues.
- Observation: Vital signs (temperature, respiration, pulse, blood pressure). Observation of the affected eye.
- Investigations: History taking from the child and parent, Physical examination of the eye, tests like Visual acuity test, Visual field test and Tonometry test for fluid pressure inside the eye (evaluates for glaucoma) are ordered and done.
- Physical Orientation: Thorough orientation to the hospital environment to help the patient post-operatively, especially if vision is impaired. Assist older children to learn details of their room (location of furniture, doors, windows, etc.). Familiarize the patient with voices and daily sounds.
- Education: Thorough education about post-operative care and restrictions. Keep the head still, avoid reading, showers, shampooing, tub baths, bending over, lifting heavy objects, and sleeping on the operative side.
- Explaining the Diagnosis and the Need for Surgery: Communicate with the patient, explaining the diagnosis and the reasons for the recommended surgery. This helps the patient understand the importance of the procedure and alleviates any concerns or fears they may have.
- Reassurance and Counseling: It is important to provide emotional support and reassurance to the patient, addressing any anxieties or fears they may have about the upcoming surgery. Counseling may also be provided to help the patient cope with the stress associated with the procedure.
- Booking and Scheduling the Operation: The date and time for the surgery are scheduled, taking into account the patient’s availability and the surgical team’s availability. In some cases, surgeries may be booked several months in advance, and the patient should be informed about what to do in case of any problems or changes before the scheduled date.
- One Week Before Surgery: Preoperative tests and assessments may be conducted, such as blood tests, imaging studies, and specific examinations related to the surgical procedure. The patient may also be instructed to take certain medications or eye drops as prescribed.
- A Day Before Surgery: In some cases, the patient may be required to be temporarily admitted to the hospital the day before the surgery. During this time, the patient’s feeding and hygiene needs are addressed, and a detailed history and physical examination, including ophthalmological tests, are performed. The patient is also informed about the personal requirements and procedure-related instructions.
- Day of Operation: The patient is required to sign a consent form, indicating their agreement for the operation. Depending on the anesthesiologist’s instructions, the patient may need to be nil per os (NPO), refraining from eating or drinking for at least 8 hours prior to surgery. Reassurance, hygiene measures, removal of jewelry, and administration of pre-medication, if necessary, are also carried out. Hydration may be provided as instructed.
- Rest and Sleep: Ensure rest and minimize noise and bright light.
- Physical Preparation:
Bowel Prep: Bowel preparation is sometimes required before surgery to empty the bowels and prevent straining post-operation. This may involve taking a laxative or using an enema the evening before surgery.
Hair Removal: Hair removal, such as shaving of eyebrows, cutting of eyelashes, and shaving of the face, should only be done on the surgeon’s order. In some cases, hair removal may be necessary to ensure a sterile surgical field.
Postoperative Bed Preparation: Depending on the type of surgery, it may be necessary to prepare a postoperative bed with side rails and sandbags for head immobilization. This is done to ensure the patient’s safety and prevent any accidental movement or injury during the recovery period.
- Transportation to the Operating Room: When it is time for the patient to be taken to the operating room, two nurses accompany the patient. This is done to ensure the patient’s safety and provide any necessary support during the transportation process.

Post-operative Care:
- When the nurses arrive at the theater to pick up the child after surgery, the first step is to check the child’s vital signs and obtain a detailed report from the theater staff who performed the surgery. This ensures continuity of care and that all necessary information is communicated effectively.
- The patient is taken to the pediatric surgical ward in a post-operative bed, positioning the child face down as ordered by the surgeon. This specific positioning is important for optimal recovery and to prevent complications.
Upon arrival at the pediatric surgical ward, the following post-operative care procedures are implemented:
Initial Care and Positioning.
- Vital Observations: Regular monitoring of vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation.
- Positioning: The child is positioned in bed as prescribed, usually face down to ensure recovery and prevent complications.
- Immobilization: If ordered, sandbags may be used to immobilize the head to prevent any unnecessary movement that could affect healing.
- Safety Measures: If both eyes are bandaged, the side rails of the bed are kept raised to prevent falls. The call bell is placed within easy reach of the patient’s head for safety and communication.
- Rest and sleep: The child is allowed to rest in the ward temporarily to recover from the effects of anesthesia. The bed positioning continues to be monitored to ensure it aligns with the surgeon’s instructions.
Ongoing Observations:
- Bleeding: Continuous monitoring for any signs of bleeding from the surgical site.
- Dressings: Regular checks to ensure dressings are secure and dry. Any signs of infection or complications are promptly addressed.
Welcoming the Child:
- The child is gently welcomed back to the ward and from the effects of anesthesia. Comforting words and reassurance are provided to help ease any anxiety or discomfort they may feel upon waking.
- Apply non-sterile gloves (to remove old eye dressing or patches/shields and discard them appropriately. If eye dressings are difficult to remove from the eyelid / lashes, apply gauze moistened with 0.9%w/v NaCl solution to the eye dressing.
- Assess the general condition of each eye and surrounding tissue before proceeding for:-
- Redness
- Swelling
- Abrasions
- Irritation (itching, stinging, burning)
- Discharge (colour, odour, volume)
- Eyelid position (partial/full closure, blink)
- If cooperative, ask the child to look upwards, or if uncooperative gently hold the child with parental assistance and then gently pull the lower lid downwards to part the eyelid.
- If there is evidence of any encrustation on the eyelids and lashes, dampen sterile gauze with 0.9%w/v NaCl solution and apply to the eye.
- If there is any discharge, perform an eye swab before proceeding with eye cleansing
Performing Eye Swabbing:
- Use a sterile cotton wool swab to roll over the conjunctival sac inside the lower eyelid.
- Place the swab in the transport medium and transport immediately to the laboratory.
- For suspected Chlamydia Infection, perform the eye swab after eye cleansing.
Performing Eye Cleansing:
- Use 0.9% NaCl or sterile water in a sterile gallipot.
- Moisten sterile gauze with the solution.
- Wipe the eye from the inside aspect to the outside aspect, using a new gauze square for each stroke.
- Clean the non-infected eye first.
- Decontaminate hands again.
Instilling Eye Medication:
- Cleanse the eye(s) before instilling medication.
- Check the child’s identification band against the medication prescription chart.
- Adolescents over 16 may consent to the procedure, but supervision is required if the medication affects vision.
- Use new medication containers post-surgery.
- Position a hand gently on the forehead while holding the medication container.
- Place a tissue/non-sterile gauze swab under the lower eyelid and gently pull down the lower eyelid.
Applying Eye Padding/Dressing(s)/Shields:
- Eye Padding: Apply gauze over the closed eyelid and secure it with tape.
- Eye Dressings: Use polyacrylamide hydrogel dressings (Geliperm®) to cover the closed eyelid.
- Eye Shield: Apply a clear shield over the affected eye and secure it with clear tape.
Precautions:
- Secure eye dressings with an eye shield or reinforce loose tape.
- Restrain the arms of children and disoriented patients as appropriate.
- Constantly watch sleeping patients to maintain proper positioning.
- Avoid jarring the bed to prevent startling the patient.
- Monitor for depression or suicidal tendencies in newly blinded patients.
- Check the physician’s orders before giving anything by mouth to avoid nausea and vomiting.
Approaching the Patient:
- Always speak to the patient upon entering their area and before touching them.
- Explain each procedure or activity fully.
- Reinforce orientation to surroundings.
- Inform the patient when leaving their area.
Diversional Activity:
- Provide non-fatiguing activities if eyes are not bandaged.
- Encourage visitors to chat or read to the patient.
- Use a radio for entertainment and to keep the patient informed.
Nursing Care of the Patient with Vision Loss:
- Physical Orientation: Describe the room and its contents in detail and lead the patient around the room.
- Precautions: Inform the patient about any changes in the room, keep doors fully open or closed, maintain the placement of toilet articles, and remove hazardous items.
- Assisting the Patient: Address the patient by name, inform them when leaving, and allow them to place their hand on your arm or shoulder when walking.
- Encourage Independence: Encourage the patient to be self-sufficient.
Complications of eye surgery;
- Infections such as Endophthalmitis: A serious infection inside the eye. This can lead to vision loss if not treated promptly.
- Fluid and Swelling like Cystoid Macular Edema: Swelling and fluid build-up in the macula, the central part of the retina responsible for sharp, central vision. This can cause blurred vision.
- Corneal Edema: Swelling of the cornea, the clear outer layer of the eye. This can cause blurry vision and discomfort.
- Bleeding (Hyphema): Bleeding in the front chamber of the eye, the space between the cornea and the iris. This can cause pain, redness, and blurry vision.
- Tissue Damage such as Capsule Rupture: The capsule surrounding the lens may rupture during surgery, leading to loss of vitreous gel, the clear jelly-like substance that fills the eye. This can cause blurry vision and other complications.
- Retinal Detachment: The retina, the light-sensitive tissue at the back of the eye, can become detached from the underlying choroid. This can lead to permanent vision loss.
- Cataract Formation: While rare, eye surgery can sometimes trigger the development of a new cataract.
- Glaucoma: Eye surgery can, in some cases, increase the pressure inside the eye, potentially leading to glaucoma.
- Dry Eye Disease: Dry eye can become worse or develop after eye surgery due to changes in the eye’s surface.
Care at Home After Eye Surgery
Bathing
- Clean your eyelid edges: At least twice a day with a moist, clean face cloth, avoiding pressure on the upper eyelid.
- Showering/Bathing: You may shower or take a tub bath and wash your hair the day after surgery.
- Avoiding Soap/Water in Eye: Ensure no soap or water enters the eye for at least one week.
- Eye Make-up: Do not wear eye make-up for at least one week.
- Avoid Fibrous Materials: Do not use cotton balls or make-up remover pads near your eye or under the eye shield.
Care of Your Eye
- Protective Eye Shield: Wear your protective eye shield when sleeping or lying down for at least one week to protect from accidental bumps or scratches.
- Cleaning the Eye Shield: Clean it once a day with 70% isopropyl alcohol and allow it to air dry before reusing.
- Glasses: You may wear your old glasses if needed. Vision may be better without them in the operated eye.
- Attaching the Shield: Attach the tape to your forehead over the shield and tape it to your cheek.
Activity
- Permissible Activities: You may watch TV, read, or go for walks if you feel up to it.
- Saunas and Hot Tubs: Avoid these for at least one week.
- Sleeping Position: Avoid sleeping on the operated side for at least two weeks.
- Straining and Lifting: Avoid straining or lifting anything over 10 lbs. (4.5 kg) for at least two weeks or until your surgeon advises otherwise.
- Swimming/Submersion: Avoid swimming or submerging your head in water for at least three weeks.
- Strenuous Activities: Do not engage in very strenuous activities or rough contact sports for at least four weeks or until cleared by your surgeon.
- Eye Protection: Avoid rubbing or bumping your eye for at least six weeks.
- Sexual Activity: Resume when you feel comfortable.
- Driving: Do not drive until your surgeon gives you the okay.
Healthy Eating
- Diet: Resume your regular diet after surgery.
- Avoid Constipation: Prevent constipation and forceful straining during bowel movements by increasing fluids, activity, and fiber in your diet.
Medications
- Regular Medications: Restart all regular medications you took before surgery unless instructed otherwise by your doctor.
- Postoperative Eye Drops: Obtain all prescriptions for postoperative eye drops and take them as directed by your surgeon.
- Artificial Tears: You may use artificial tears like Refresh™ or Genteal™ to reduce scratchiness. Wait 30 minutes after using prescription eye drops before using artificial tears.
When to Seek Help
- Worsening Eyesight: If your eyesight worsens.
- Increasing Pain: If you experience increasing pain or ache in the eye.
- Redness: If there is increasing redness.
- Swelling: If there is swelling around the eye.
- Discharge: If there is any discharge from the eye.
- New Symptoms: If you notice new floaters, flashes of light, or changes in your field of vision.
How to Instill Eye Drops
- Wash Your Hands: Ensure your hands are clean before touching your eye drops.
- Tilt Your Head: Look at the ceiling from a sitting or lying position.
- Form a Pocket: Use one or two fingers to gently pull down your lower eyelid to form a pocket.
- Instill the Drop: Keeping both eyes open, gently squeeze one drop into the eye pocket. Avoid letting the bottle top touch your eye, eyelashes, fingers, or any surface.
- Close the Eye: Close the eye for 30 to 60 seconds to let the drops absorb.
- Avoid Rubbing: Do not rub your eyes after applying the drops. Gently blot the eye area with a tissue if needed.
- Multiple Drops: When using multiple eye drops, wait about three minutes after instilling the first medication before applying the next.

Responsibility of nurse during ophthalmology
The Nurse’s Role in Ophthalmic Visual Acuity Testing
Visual acuity, the measurement of central vision sharpness, is a cornerstone of any ophthalmic examination. An accurate assessment is important for diagnosis and treatment planning. It tests the entire visual system, from the occipital cortex (brain) to the cornea (front of the eye).
Nurses responsibilities include;
1. Preparing the Patient:
- Explaining the Test: Clearly explain the purpose of the test and how it’s conducted, ensuring the patient understands the process.
- Addressing Concerns: Answer any questions the patient may have regarding the test.
- Ensuring Comfort: Make the patient feel comfortable and relaxed. Offer assistance with positioning and support.
- Assessing Language Barriers: Identify and address any language barriers to ensure comprehension.
2. Performing the Test:
- Using the Appropriate Chart: Select the appropriate visual acuity chart based on the patient’s age, literacy, and any specific needs (e.g., Snellen chart for adults, LEA chart for children).
- Maintaining Proper Distance: Ensure the patient is positioned at the correct distance from the chart (typically 20 feet or 6 meters).
- Occluding the Non-Tested Eye: Properly cover the non-tested eye to avoid cross-viewing.
- Recording Results: Accurately document the visual acuity reading for each eye, including the distance from the chart and the line identified.
3. Identifying Factors that May Affect Acuity:
- Refractive Error: Assess for signs of refractive errors (nearsightedness, farsightedness, astigmatism) that could impact visual acuity.
- Media Opacity: Observe any cloudiness in the ocular media (cornea, lens, vitreous) that may interfere with light transmission and affect acuity.
- Patient Cooperation: Recognize and document any lack of patient cooperation or comprehension that could affect the accuracy of the test.
4. Reporting Observations:
- Communicating with the Ophthalmologist: Communicate any relevant observations, including patient cooperation, suspected refractive errors, or signs of media opacity to the ophthalmologist for further assessment and diagnosis.
Factors Influencing Accurate Visual Acuity Testing:
- Patient Cooperation: The patient must understand and follow instructions, including focusing on the chart and maintaining a fixed gaze.
- Recognition of Forms: The patient needs to be able to identify the forms displayed on the chart.
- Ocular Media Clarity: The cornea, lens, and vitreous must be clear for light to pass through and reach the retina.
- Focusing Ability: The eye must be able to focus properly on the chart.
- Eye Convergence: Both eyes need to work together to converge on the target.
- Retinal Function: The retina must be able to receive and process the visual information.
- Intact Visual Pathways: The optic nerve and brain pathways must be intact for visual information to travel to the brain.
Common charts used in the measurement of distance visual acuity
The most common chart for measuring distance visual acuity in a literate adult is the Snellen chart. Distance vision is tested at 6 meters, as rays of light from this distance are nearly parallel. If the patient wears glasses constantly, vision may be recorded with and without glasses, but this must be noted on the record. Each eye is tested and recorded separately, the other being covered with a card held by the examiner.
Snellen’s Chart
Heavy block letters, numbers, or symbols printed in black on a white background are arranged on a chart in nine rows of graded size, diminishing from the top downwards. The top letter can be read by the normal eye at a distance of 60 meters, and the following rows should be read at 36, 24, 18, 12, 9, 6, 5, and 4 meters, respectively.
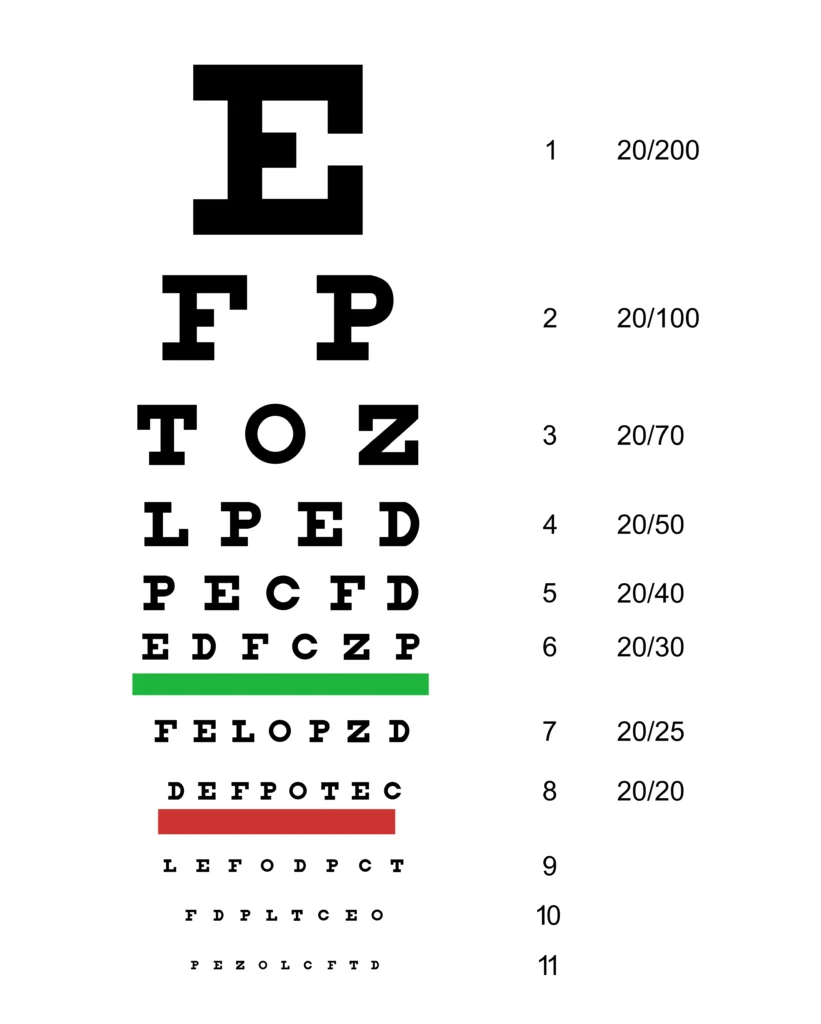
Procedure:
- One eye is tested at a time, with the other eye covered.
- The patient reads lines of letters, starting from the top and working down.
- The smallest line the patient can read correctly indicates their visual acuity.
Recording: Visual acuity is recorded as a fraction (e.g., 20/20, 6/6), where the numerator represents the distance at which the patient can read the line and the denominator represents the distance at which a person with normal vision can read that same line.
Using the pinhole in the measurement of visual acuity
Occasionally, a patient’s visual acuity may be below average, which could be a result of a refractive error not corrected by glasses, or due to the patient wearing an old pair of prescription glasses. One effective, but very simple, way to see if distance visual acuity can be improved through spectacles or a change of prescription is a pinhole. A pinhole disc only allows central rays of light to fall onto the macula and does not need to be refracted by the cornea or lens. A ‘pinhole disc’ is used if the VA is less than 6/6 or 6/9, which may improve VA. If a considerable increase in vision is obtained, it may usually be assumed that there is no gross abnormality, but rather a refractive error.

- Purpose: Used when visual acuity is below average, to determine if the problem is refractive error (uncorrected by glasses) or another condition.
- Method: A pinhole disc restricts light to pass through a small opening, improving focus and reducing blur caused by refractive errors.
- Interpretation:
- If visual acuity significantly improves with the pinhole, it suggests a refractive error.
- If visual acuity does not improve, it may indicate another underlying eye condition.
Sheridan Gardner Test Chart
The Sheridan Gardner test chart can be used for children and patients who are illiterate. This test type has a single reversible letter on each line. For example, A, V, N. The child holds the card with these letters printed on and is asked to point to the letter on his card which corresponds to the letter on the test type. This test can also be used for very young children as they do not have to name a letter.
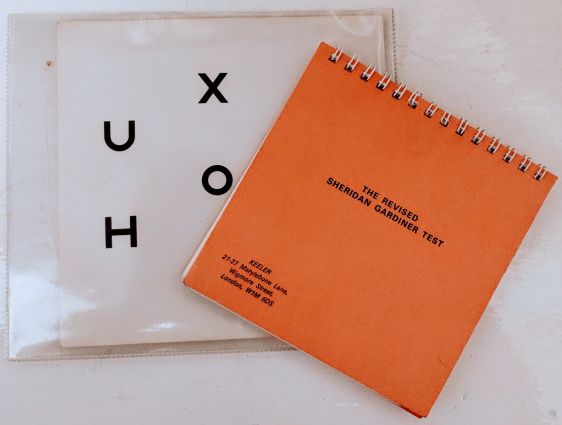
Procedure:
- The patient holds a card with the same letters printed on it.
- The examiner points to a letter on the chart.
- The patient points to the corresponding letter on their card.
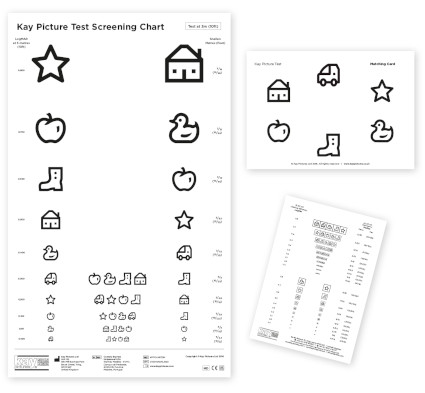
Kay Picture Chart
The Kay picture chart is again used with patients who are illiterate or with children. Instead of letters, the book contains pictures, which are also of varying sizes. The patient is asked what the picture represents. In order to avoid any misunderstanding amongst patients with language difficulties, it is good practice to ask the hospital’s official interpreter to translate for patients.
Tumbling E chart
The tumbling E chart is mainly used for patients who are illiterate. In the chart, the Es face in different directions. The patient is asked to hold a wooden E in his hand and to turn it the same way as the one the examiner is pointing to on the test chart.
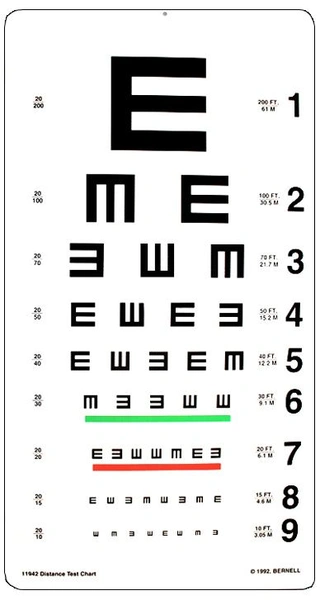
Procedure:
- The patient holds a wooden “E”.
- The examiner points to an “E” on the chart.
- The patient rotates their wooden “E” to match the orientation of the “E” on the chart.



The content adds knowledge
Appreciate your efforts
Thanks.
Well elaborated keep it up
This is a very helpful Note, thanks so much.. however, different surgeries have their different nursing care, I feel would be good if explained according to a specific surgery