Table of Contents
ToggleOrganophosphates Poisoning
Organophosphates Poisoning is when a person develops an illness as a result of organophosphate exposure.
Organophosphates are chemicals in insecticide used extensively in agriculture. When people, such as agricultural workers, are exposed to large quantities of organophosphates, these chemicals can be harmful.
Organophosphates include: parathion, fenthion, malathion, diazinon, dursban, quinalphos and prothoate.
Fast facts on organophosphate poisoning
- Nearly 25 million cases of unintentional pesticide poisoning occur in the agricultural industry across the world each year.
- Globally, it is reported that 3 million or more people are exposed to OPs every year, accounting for 300,000 mortalities.
- In the United States, there are around 8000 exposures per year, with fewer deaths. Poisoning leads to significant morbidity and mortality each year in India. According to the National Crime Records Bureau of India, there were 27,657 deaths and suicides by poisoning in 2015.
- Cases are most common in regions where workers do not use or do not have access to protective gear, such as suits or masks.
- Symptoms and complications vary but can include death.
Definitions
- Poison: A foreign chemical that is capable of producing a harmful effect on a biologic system (xenobiotic)
- Poisoning: The development of harmful effects on normal body functions following exposure to chemicals after it is swallowed, inhaled, injected or absorbed.
Pathophysiology of Organophosphates Poisoning.
Organophosphates exert their acute effects by causing overstimulation at cholinergic nerve terminals. Acetylcholine (Ach) is found in the central and peripheral nervous systems, neuromuscular junctions and red blood cells (RBCs). Normally, acetylcholinesterase (AChE) catalyzes the degradation of the neurotransmitter Ach into choline and acetic acid in the synapse. OP pesticides act by binding irreversibly to the AChE, thereby reducing the ability of the enzyme to break down the neurotransmitter. This produces an accumulation of Ach in the central and peripheral nervous systems, resulting in an acute cholinergic syndrome via continuous neurotransmission. The clinical onset of cholinergic overstimulation can vary from almost instantaneous to several hours after exposure. Although most patients rapidly become symptomatic, the onset and severity of symptoms depend on the specific compound, amount, route of exposure and rate of metabolic degradation.
Routes of absorption during organophosphate poisoning
- Ingestion – Gastrointestinal (GI) tract (accidental, deliberate)
- Cutaneous – Skin
- Inhalation – Lungs.

Signs and symptoms of organophosphates poisoning
Organophosphate poisoning symptoms can range from mild to severe. In more severe cases, a person may die from the toxicity.
The length and strength of the exposure will determine the nature of someone’s symptoms. Symptoms may start in as little as a few minutes or after several hours.
Symptoms of mild exposure to organophosphates include:
- Blurry or impaired vision
- Watery eyes
- Narrowed pupils
- Stinging eyes
- Nausea
- Runny nose
- Muscle twitching
- Glassy eyes
- Extra saliva
- Headache
- Muscle fatigue or weakness
- Agitation
Symptoms of moderate exposure to organophosphate include:
- Dizziness
- Very narrow pupils
- Fatigue
- Muscle tremors
- Muscle twitching
- Drooling
- Disorientation
- Wheezing or coughing
- Severe diarrhea
- Difficulty breathing
- Sneezing
- Uncontrolled urination or bowel movements
- Excessive phlegm
- Muscle weakness
- Severe vomiting
Symptoms of emergency-level exposure to organophosphate include:
- Confusion
- Narrow pupils
- Convulsions
- Coma
- Agitation
- Excessive secretions, such as saliva, sweat, tears, and mucus
- Irregular or slow heartbeat
- Collapsing
- Breathing that is ineffective stops
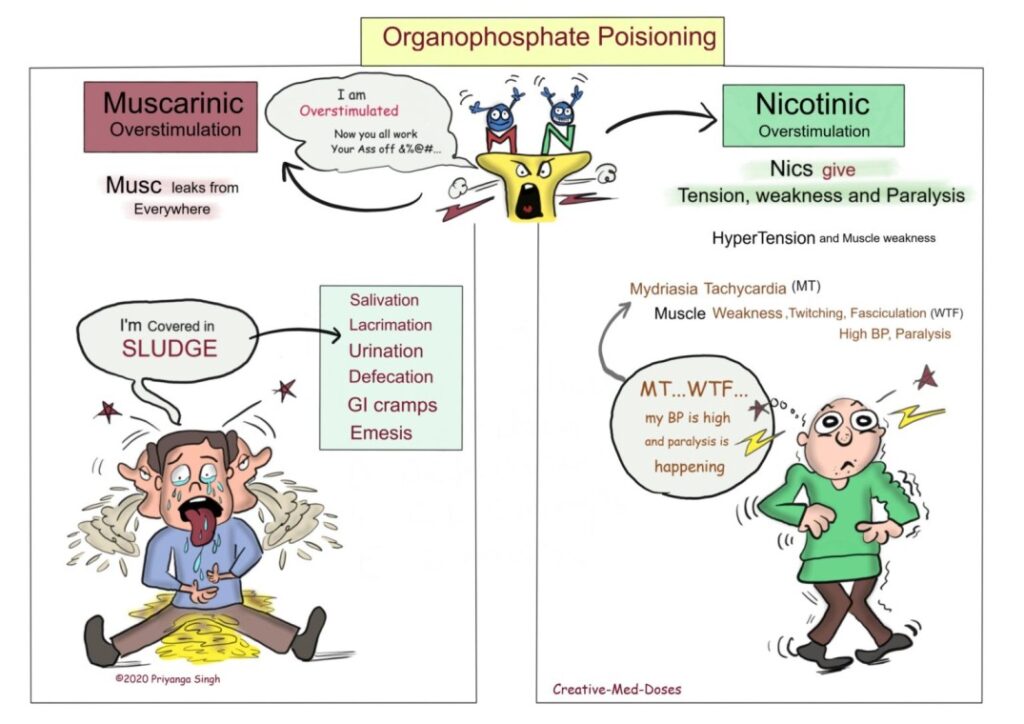
Signs and Symptoms according to stimulation
Muscarinic signs and symptoms
“Musc leaks from everywhere”
Remember this mnemonic SLUDGE, there is excessive secretions from everywhere in muscarinic overstimulation.
- S – salivation
- L- lacrimation
- U- urination
- D- defecation
- G- GI cramps
- E- emesis
Nicotinic signs and symptoms
“Nics give tension (hypertension), weakness and paralysis”
Remember this mnemonic MT WTF my BP is high, and Paralysis is happening.
- M-Mydriasis
- T-Tachycardia
- W-muscle weakness
- T-muscle twitching
- F-muscle fasciculation
- BP is high- hypertension
- Paralysis is happening – muscle paralysis
Complications
In addition to immediate signs and symptoms, organophosphate exposure can cause a number of long- term complications. Again, the severity of the complications depends on the extent and length of exposure.
- Paralysis
- Fertility issues
- Cancer
- Metabolic disorders, such as high blood sugar levels
- Inflammation of the pancreas
- Excess acid in the blood
- Brain and nerve problems
Diagnosis of Organophosphate Poisoning
1. History
2. Physical examination
3. Vital signs
- Depressed respirations, bradycardia and hypotension are possible findings.
4. Laboratory investigations:
- Plasma pseudocholinesterase levels: Normal 3000–8000 U/L. Serum levels may be < 1000 U/L
- RBC AChE level:
- White blood cells (WBC) – Leucocytosis is seen
- ABG values to rule out acidosis – Metabolic and/or respiratory acidosis
- Potassium and magnesium levels are decreased.
5. Imaging studies
- Chest X-ray for
- Electrocardiogram for ventricular
Medical management
Step 1: Identify the nature of poison i.e. OP, carbamate, chloride, pyrethroid.
Step II: Decontamination
- Staff must have on protective equipment before commencing treatment including mask, gloves, gowns and eye protection. Staff involved in direct contact with patient’s bodily secretions should immediately and thoroughly wash the affected area with soap and water.
- Gastric lavage should be done only after stabilizing the forced emesis if patient is awake. Gastric lavage is given within 1 hour of ingestion of Organophosphates. Activated charcoal 0.5–1 g/kg can be given within 1 hour of ingestion, but studies have shown no benefit.
Step III: Maintaining airway, breathing and circulation
- Airway: Maintain clear airway and ensure adequate oxygenation. Check gag reflex. If absent, intubate before stomach wash.
- Breathing: Administer oxygen 6 L/min by Intubation if breathing is inadequate, oximetry is <90%, or Glasgow coma scale (GCS) <8. Administer injection atropine 0.05 mg/kg (2 mg in adults) every 5 min to reduce bronchial and oral secretions until adequately atropinised.
- Circulation: Administer adequate intravenous (IV) fluids through a wide bore cannula to replace volume loss.
Step IV: Cardiac monitoring
- Monitor for arrythmias.
Step V: Specific therapy Antidotes
- Atropine is given in intermittent boluses 2 mg every 5 min or as an infusion. The aim is to keep patient airway dry.
- Atropinisation is to be initiated as soon as diagnosis is suspected.
- Signs of atropinisation: Heart rate about 100/min, pupils mid position, bowel sounds just heard, clear lung sounds, dry skin
- Protocol for atropinisation: Injection atropine 2 mg IV bolus is administered, and then the dose is doubled every 5 min till atropinisation is achieved.
- Signs of atropine toxicity (anticholinergic toxidrome): Dry mucus membranes (dry as a bone), mental status changes (mad as a hatter), flushed skin (red as a beet), mydriasis (blind as a bat), fever (hot as hell), tachycardia, hypertension, decreased bowel sounds/GI motility and urinary retention.
- Atropine toxicity is treated with injection haloperidol 5 mg intramuscular or IV and by reducing the dose of atropine.
Antibiotics
- Antibiotics are not usually indicated for OP.
- Gastric lavage with an unprotected airway and/or a low GCS in the setting of poisoning are the risk factors for aspiration.
- If aspiration pneumonia is suspected (fever, leucocytosis, pulmonary infiltrates with worsening oxygenation), antibiotics such as penicillin (ceftriaxone, amoxycillin or clauvulenic acid, piperacillin tazobacterium [Piptaz]) may be considered.
Sedation
- Agitation in the setting of OP poisoning may indicate over atropinisation, hypoxaemia, or distress due to pain/discomfort. Intubated patients need a combination of an analgesic and a sedative such as morphine + lorazepam as an infusion. Haloperidol may increase seizure threshold and is not recommended unless patients are unresponsive to other drugs.
- Lasix is the drug of choice if pulmonary oedema persists even after full atropinisation
Nurses roles during management of organophosphate poisoning
- Assessing the airway for bilateral equal air entry, respiratory rate and breath sounds
- Assessing for cough and gag reflex and for bronchospasms.
- Changed position every 2 hourly to mobilize secretions.
- Positioning him in semi-fowlers at 45° to promote lung expansion and to prevent aspiration.
- Maintaining adequate hydration by administering IV fluids.
- Providing humidification to airways to thin secretions.
- Checking for neck muscle weakness, use of accessory muscles for breathing.
- Assessing single breath count.
- Assisting for intubation.
- Checking the ventilator settings of the patient.
- Positioning patient in semi-fowler’s position to promote diaphragmatic descent and maximal inhalation.
- Performing suctioning whenever necessary.
- Assessing heart rate, rhythm for arrhythmias, BP, capillary refill time, skin turgor, vital signs every hour.
- Assessing peripheral sites for perfusion.
- Monitoring urine output every hour.
- Administered atropine infusion to maintain the heart rate above 90/min.
- Monitoring vital signs.
- Following strict aseptic technique while handling invasive lines and while performing suctioning.
- Providing oral care with chlorhexidine solution.
- Checking for the colour, consistency and volume of secretions.
- Monitored ABG values, WBC counts, culture and sensitivity results, chest X-ray.
- Administering injection Piptaz 4.5 g IV q 8 hourly as per the order.
- Evaluating his feelings and perception of the reasons for lack of power and sense of helplessness.
- Involving him in care.
- Identifying his usual belief/locus of control that influences his life.
Opium/Opioid poisoning
Voluntary or accidental overdose of opioid drugs
Clinical features
- Respiratory depression
- Hypotension
- Hypothermia
- Pinpoint pupils
- Decreased mental status or coma
Management
- Aim at restoring respiration not consciousness
- Give antidote; naloxone 4-2mg IV or IM repeat dose every 2-3minutes if not improving up to max of 10mg
- For children give 0.1mg/kg
NB
- Naloxone is contraindicated opioid-induced respiratory depression in chronic opioid use like in palliative care of cancer patients
TOXICOLOGY/POISONING:
Toxicology is a scientific study of adverse effects of chemicals/poisons and their effect on living system
Poisoning refers to bodily entry of toxic substance in amounts that cause dysfunction of body system
Antidote is a chemical substance that stops or counteracts effects of a poison
It is caused by;
- Micro organism e.g. in food poisoning
- Inorganic sources e.g. lead, mercury, copper metal poisoning
- Organic sources e.g. agriculture chemical, paraffin, petrol
- Drug abuse e.g. alcohol or medicines in excess amounts
GENERAL MANAGEMENT OF POISONING
- Refer patients to the admission
- In hospital, admit all patients with history or signs of poisoning even if they are well.
- Optimal management depends on the specific poison taken, presenting and suspected illness and time has elapsed between exposure and presentation.
Management includes;
- Supportive care
- Decontamination and enhanced elimination techniques
- Antidote therapy
Supportive therapy
- Airway and breathing support
- Position in semi prone to minimize risk of aspiration of vomitus
- Maintain airway patent and if necessary assist in ventilation
- Administer oxygen
- Blood pressure
- If hypotensive, raise foot of bed and start IV N/S
- If hypertensive manage appropriately
6. Temperature
- If hypothermic, cover with heavy blanket
- If hyperthermic, tepid sponging and give antipyretics
7 .Convulsion
- Give diazepam 10mg rectally of 5-10mg as slow IV in adults. Max dose is 30mg
- In children 0.5mg/kg rectally or 0.2mg/kg as IV
8. Counsel patient and families on poisoning
Decontamination
It refers to removal and elimination of poison.
It has to be implemented after stabilization of vitals.
It involves;
- Removal of the stomach, Do not induce vomiting
- Balance dangers of gastric emptying against the likely toxicity of swallowed medicine
- Insert NG tube perform gastric lavage. It is useful if done within 2 hours of ingestion of poison and is contraindicated in comatose patients, and in corrosive or petroleum products
- Prevention of absorption and enhance active elimination
- Administer activated charcoal to bind the poison in the stomach and reduce absorption. Give 50g (250mg) repeated every 4 hours if necessary. Grind the tablet into fine powered then mix with 100mls of water. In children give 0.5-1g/kg.
- This is effective within 2 hours of ingestion of poison and is contraindicated in intestinal obstruction, corrosive or petroleum products, toxins that are poorly absorbed by charcoal, depressed mental status in late presentation
Benzodiazepine toxicity
- Benzodiazepines are used in anxiety and as a sedative drug its overdose can be international or accidental
Clinical presentations
- Confusion or drowsiness
- Hypotension
- Unresponsiveness or coma
- Respiratory depression
- Nystagmus
- Hallucinations
- Slurred speech
- Body weakness/ hypotonia
Management
- Obtain a baseline prothrombin time and international normalized ratio (PT/INR) and make arrangements for a repeat measurement in 24-48 hours
- Administer activated charcoal for recent (within the last 1-2 hours)
- Gastric lavage is unnecessary if rapid administration of activated charcoal is feasible/ carried out
- If the patient is elevated, the effects of wafarin can be reversed with vitamin K1 is appropriate; 10mg orally or by slow IV infusion or flesh frozen plasma (FFP)
- For urgent reversal of the effects, prothrombin complex concentrate (PCC) also known as factor IX complex, has been approved in urgent reversal of acquired coagulation factor deficiency induced by wafarin
Paracetamol toxicity
- Accidental or international consumption of paracetamol
- Toxic dose>150mg/kg or 7.5g
Clinical features
- First 24 hours, the individual may be asymptomatic or may present with nausea, vomiting, malaise and abdominal pain
- In 24-72 hours, progressive signs of hepatoxicity appear such as right upper quadrant pain, enlarged tender liver and raised LFT
- After 72 hours, its followed by either recovery after 5-7 days or progression to hepatic failure
Management
- If ingestion occurred less than two hours, perform gastric lavage to empty the stomach and remove any remaining medicine
- Give repeated doses of activated charcoal like 25-50g every 4 hours
- Give acetylcysteine IV preferably within 8 hours from ingestion. It work to reduce paracetamol toxicity by providing cysteine for glutat5haione synthesis which is an antioxidant. Glutathione reacts with the toxic metabolite so that it does not damage cells and can be safely excreted.
It can be given as follows;
- 150mg/kg (max 15g) in 200mls D5 in 60 minutes followed by
- 50mg/kg (max5g) in 500ml D5 in 4 hours followed by
- 100mg/kg (max 10g) in 100ml D5 in 16 hours
Aspirin/acetylsalicylic poisoning
- Overdose of ASA occurs when there is consumption of > 10g in adults and 3g in children
Clinical features
- Mild to moderate toxicity; hyperventilation, nausea, vomiting, vasodilation and tinnitus
- Severe toxicity; hyperpyrexia, convulsions, altered mental status,
- Acidosis
Food poisoning
This is illness caused by consumption of food or water caused by pathogenic micro-organism.
It caused by infections with mainly salmonella typhi or toxins released by micro-organisms
Clinical features
- Nausea and vomiting
- Intermittent abdominal pain
- Diarrhoea
- Fever
Management
- Give ORS or IV fluids normal saline to rehydrate the patient
- Give paracetamol 1g 6 hourly incase of abdominal pain
- Establish the cause and treat accordingly
- In severe cases, give antibiotics like ciprofloxacin 500mg 12 hourly or metronidazole 400mg tds
Prevention
- Heat cooked food thoroughly before eating and avoid leftovers
- Ensure food and utensil hygiene
- Ensure personal hygiene
Carbon monoxide poisoning
- Carbon monoxide is a colourless, odourless and non-irritating gas. The poisoning can result from inhalation of smoke, car exhaust or fumes or use charcoal stoves in unventilated rooms
Clinical features
- Headache, dizziness and confusion
- Nausea and vomiting
- Seizures, collapse and coma
Management
- Move person to fresh air
- Clear airway
- Give 100% oxygen via non-rebreather mask
- Re-assess the ABGS
- IV fluids incase of hypotension
- Diazepam for seizures
Methanol toxicity
Methanol is used as an industrial solvent and is an ingredient of methylated spirits
Methanol is a product of incomplete conversion of alcohol to ethanol especially in home- distilled crude alcohol. When taken, it’s transformed into toxic products in the body that cause acidosis
Ingestion of a dose >1g/kg is lethal
Clinical features
- Initially presents with; headache, dizziness, nausea, vomiting and visual disturbances
- Later CNS depression, respiratory failure and coma
- Toxic metabolites may cause severe acidosis and retinal optical nerve damage
Management
- Gastric lavage if ingestion occurred within 1 hour to arrival
- Charcoal is not effective
- Give IV fluids to manage shock and hypovolemia
- Administer deferoxamine as an antidote for iron toxicity. Give a continuous infusion of 5mg/kg/hr in N/S or D5. Continue until metabolic acidosis clears or symptoms improve. Do not use for more than 2 hours
- Avoid the drug in cases of renal failure
Paraffin and other petroleum products
- Petroleum products include; paraffin, petrol, paint thinners and organic solvents
Clinical features
- Patient may smell paraffin or other petroleum products
- Burning sensation in the mouth and throat
- Patient looks pale, dyspnea and tachypnea
- Vomiting, diarrhoea and bloody stool
- Cough
- Lethargy
Management
- Remove clothes and wash skin with soap and water if contaminated
- Avoid gastric lavage or use of enemas.
- Do not give charcoal
- Treatment is supportive or symptomatic
- Administer oxygen if hypoxic