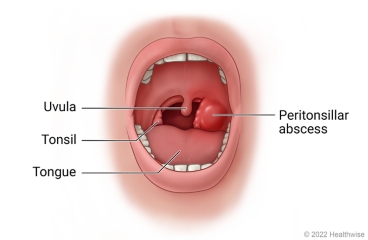
Peritonsillar abscess, often referred to as Quinsy, represents a localized collection of pus situated in the peritonsillar space. This space is found between the tonsillar capsule and the superior constrictor muscle of the pharynx.
It generally involves a pus-filled pocket that forms near one of the tonsils. It is a collection of pus around the tonsils. It usually begins as a complication of untreated streptococcal throat or tonsillitis infection
- Localized Collection of Pus: This indicates an infection that has progressed beyond simple inflammation to form a contained pocket of purulent material (pus).
- Peritonsillar Space: This anatomical region is a potential space, meaning it is not normally open, but can become filled due to infection. It is bordered by:
- Medially: The palatine tonsil and its capsule.
- Laterally: The superior constrictor muscle, which forms part of the pharyngeal wall.
- Relationship to Tonsillitis: A peritonsillar abscess is considered a complication of acute tonsillitis, meaning it often develops following a prior tonsillar infection that has either gone untreated or not responded adequately to initial therapy. While related to the tonsil, the abscess itself is outside the tonsillar tissue, in the surrounding connective tissue.
- Unilateral Presentation: Peritonsillar abscesses almost invariably affect only one side of the throat, which is a key distinguishing feature from uncomplicated tonsillitis, which is usually bilateral.
Understanding how a peritonsillar abscess (PTA) forms involves examining both the causative agents and the sequence of events within the throat that leads to this distinct pus collection.
The formation of a peritonsillar abscess is almost always linked to a bacterial infection.
- Bacterial Infection:
- Primary Culprit: The organism most frequently isolated from PTAs is Group A Streptococcus pyogenes (GAS), the same bacterium responsible for most cases of "strep throat."
- Polymicrobial Nature: While GAS is prominent, many PTAs are polymicrobial, meaning they involve a combination of bacteria. Other common pathogens include:
- Staphylococcus aureus (including Methicillin-resistant S. aureus - MRSA in some regions).
- Respiratory anaerobes (e.g., Fusobacterium, Bacteroides, Peptostreptococcus species). These anaerobic bacteria thrive in low-oxygen environments and are particularly common in abscess formation.
- Viral Precursors: Though bacteria cause the abscess, a preceding viral tonsillitis can sometimes weaken the local defenses, making the area more susceptible to subsequent bacterial invasion and abscess development.
- Origin from Tonsillitis: A peritonsillar abscess is regarded as a complication of acute tonsillitis, meaning it typically arises after a bout of tonsillar inflammation. This connection is fundamental to its etiology.
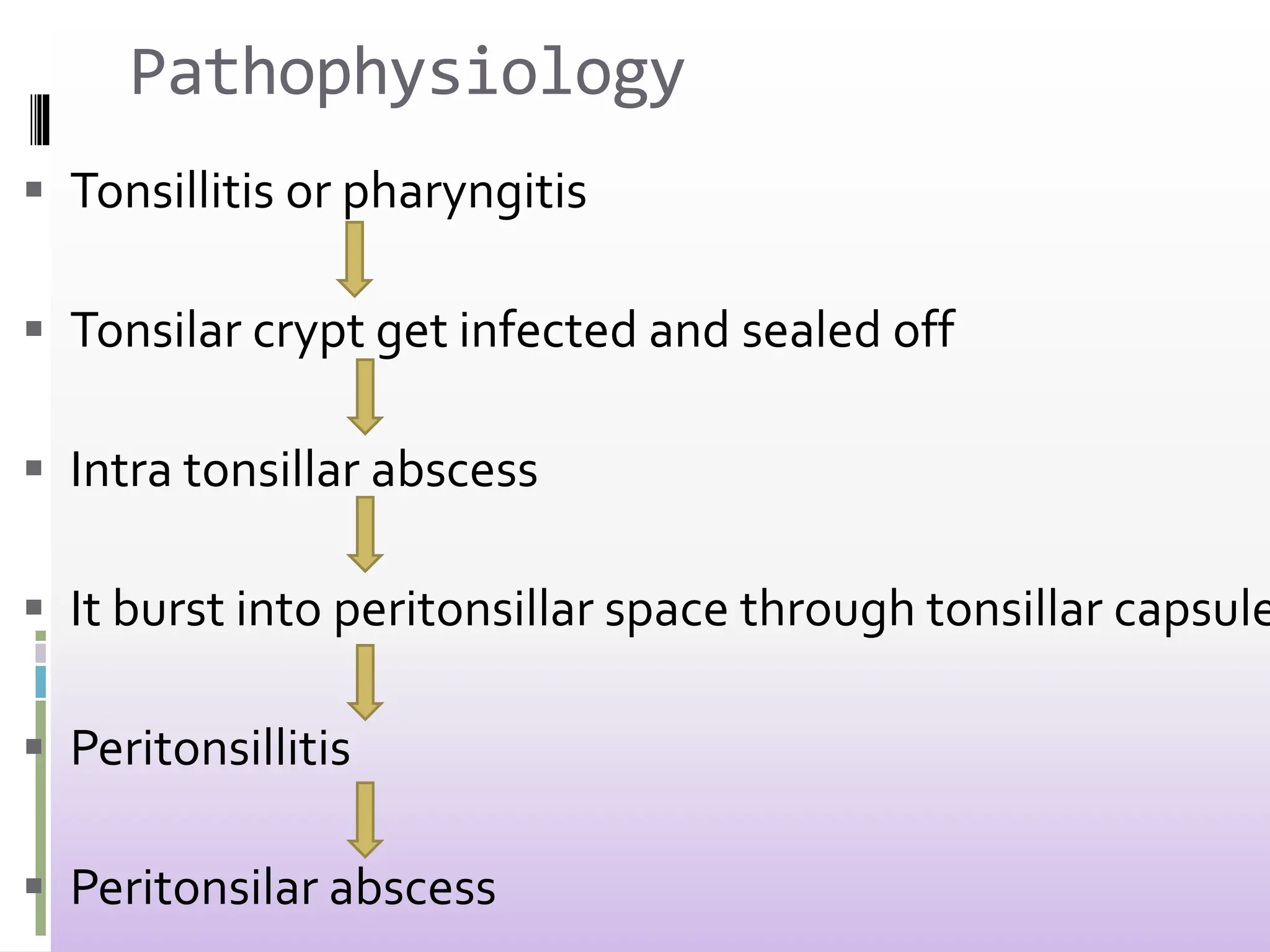
The development of a peritonsillar abscess is a sequential process that begins with infection and progresses to tissue breakdown and pus accumulation.
- Initial Infection: The process commences with an infection of the tonsils (tonsillitis), predominantly bacterial.
- Inflammation and Crypt Involvement: The infection spreads within the tonsillar tissue, leading to marked inflammation. The deep crypts within the tonsils can become obstructed and infected.
- Spread to Weber's Glands: A generally accepted theory points to the infection originating in the salivary glands of Weber. These are small mucous glands located superior to the tonsil, in the supratonsillar fossa (the small depression above the tonsil). Their ducts can become blocked by inflammation or debris.
- Abscess Formation:
- Once Weber's glands are infected and obstructed, the infection spreads from these glands into the peritonsillar space.
- This space, as defined earlier, lies between the tonsillar capsule and the pharyngeal constrictor muscle.
- The bacterial proliferation, coupled with the body's immune response, leads to tissue necrosis (death) and liquefaction, forming a collection of pus.
- The inflammation and pus collection cause the tonsil and its surrounding structures to bulge medially (towards the midline of the throat).
- Unilateral Predominance: The anatomy of the peritonsillar space and the involvement of Weber's glands (which are present in both tonsils but infection often localizes to one side) contribute to the distinctive unilateral presentation of most peritonsillar abscesses.
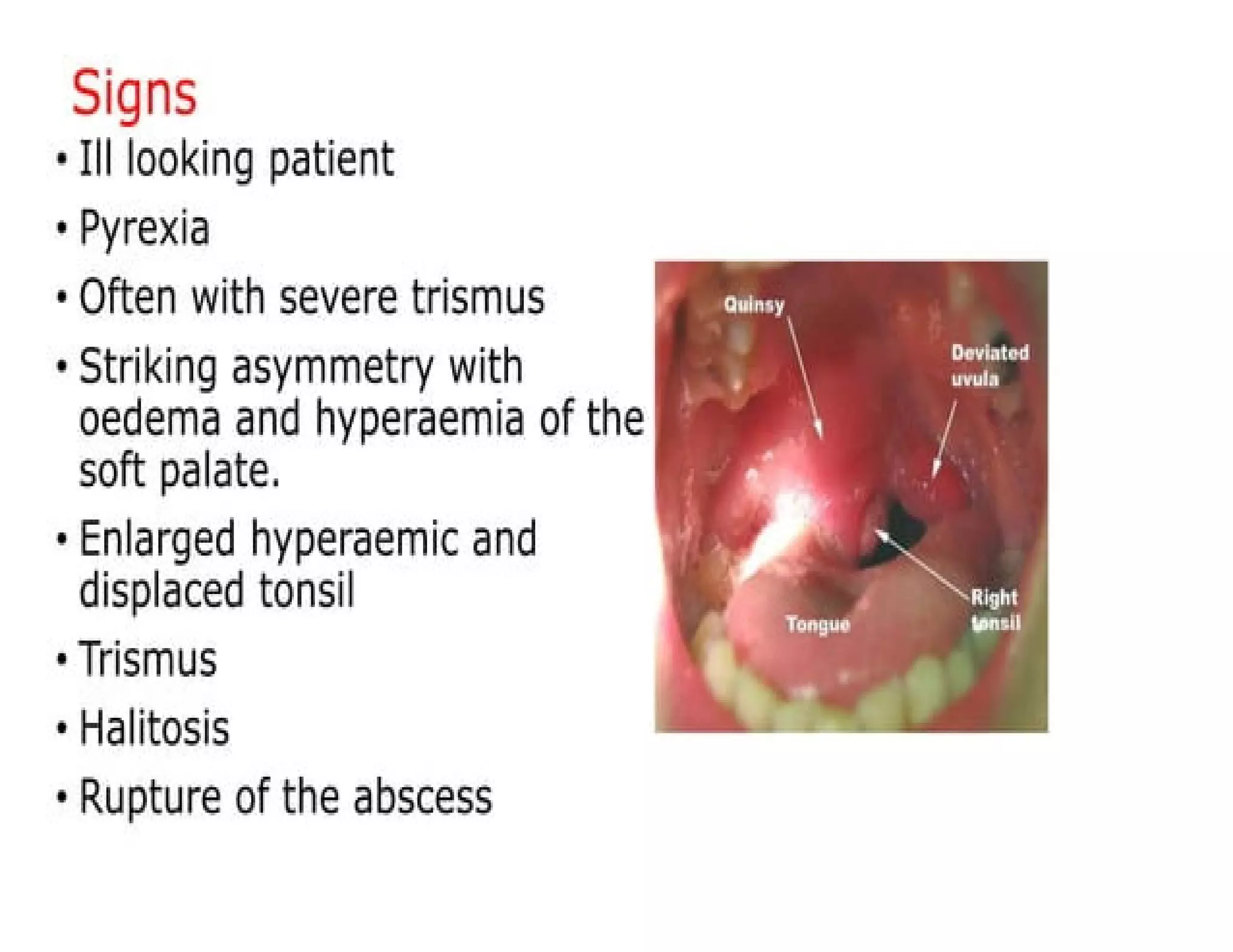
The clinical presentation of a peritonsillar abscess (PTA) is distinct and often more severe than uncomplicated tonsillitis. The signs and symptoms arise from the inflammation, pus accumulation, and muscle spasms in the peritonsillar region. Presentation is USUALLY unilateral.
- Severe Sore Throat (Unilateral): This is a predominant symptom, often described as intense and localized to one side of the throat. Unlike tonsillitis, which is frequently bilateral, the pain of a PTA is almost always felt more strongly on one side.
- Odynophagia (Painful Swallowing): Extreme pain upon swallowing, often making even sips of water unbearable. This can contribute significantly to dehydration.
- Dysphagia (Difficulty Swallowing): The swelling and pain can make the physical act of swallowing very difficult, sometimes leading to drooling.
- Trismus (Difficulty Opening the Mouth): This is a highly characteristic sign. It refers to painful spasm of the masticatory muscles, making it hard or impossible to fully open the mouth. Caused by Irritation of the pterygoid muscles due to inflammation in the adjacent peritonsillar space.
- "Hot Potato" Voice (Muffled Voice): The patient's voice sounds muffled, as if they are speaking with a hot object in their mouth. Caused by swelling and edema of the soft palate and pharyngeal structures interfere with vocal resonance.
- Drooling/Sialorrhea: Due to extreme pain and difficulty swallowing saliva, patients may drool.
- Fever and Chills: Systemic signs of infection are common, including elevated body temperature and shivering.
- Malaise and Fatigue: A general feeling of discomfort, illness, and lack of energy.
- Halitosis (Bad Breath): The presence of pus and infection can cause foul-smelling breath.
- Referred Ear Pain (Otalgia): Pain can sometimes be felt in the ear on the same side as the abscess due to shared nerve pathways (glossopharyngeal nerve).
- Unilateral Tonsillar Swelling: The affected tonsil appears significantly enlarged and displaced.
- Medial and Inferior Displacement of the Tonsil: The tonsil is often pushed towards the midline and downwards.
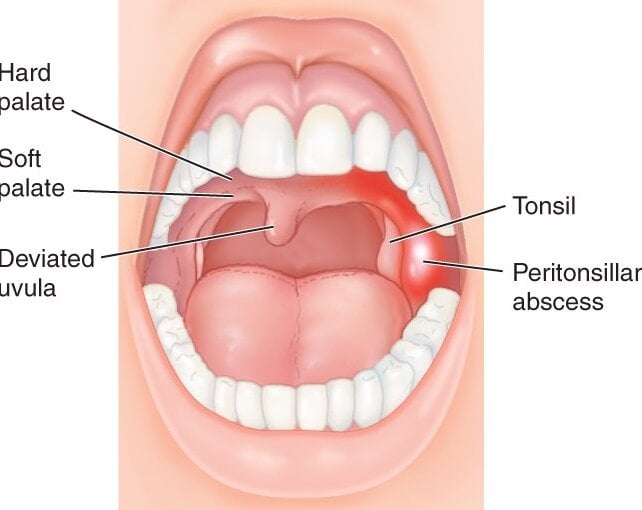
- Bulging of the Soft Palate: The area just above and lateral to the affected tonsil (soft palate) appears red, swollen, and bulging (as shown in your image "3. Peritonsillar Abscess").
- Uvular Deviation: The uvula (the fleshy extension hanging at the back of the soft palate) is typically pushed away from the affected side, towards the unaffected side of the throat. This is a very suggestive sign.
- Exudates: Pus or white patches may be visible on the tonsil, similar to tonsillitis.
- Cervical Lymphadenopathy: Swollen, tender lymph nodes in the neck, particularly on the affected side.
Diagnosing a peritonsillar abscess (PTA) relies primarily on a thorough clinical assessment.
- Inquire about the duration and severity of symptoms.
- Determine if there was a preceding sore throat or tonsillitis.
- Elicit information regarding the unilateral nature of the pain, difficulty swallowing, muffled voice, and especially trismus.
- Document fever, chills, and general malaise.
- Throat Inspection:
- Ask the patient to open their mouth as wide as possible (noting any trismus).
- Visually inspect the oropharynx, paying close attention to the soft palate, tonsils, and uvula.
- Key Findings: Observe for:
- Unilateral bulging of the soft palate adjacent to the affected tonsil.
- Medial and inferior displacement of the affected tonsil.
- Uvular deviation to the contralateral (unaffected) side.
- Erythema (redness) and edema (swelling) of the affected area.
- Exudates on the tonsil may or may not be present.
- Palpation: Gently palpating the soft palate with a gloved finger (if tolerated by the patient and if trismus allows) can sometimes confirm fluctuance (the sensation of fluid beneath the surface), which is highly indicative of an abscess. However, this can be extremely painful and may not always be necessary or feasible.
- Neck Examination: Palpate the cervical lymph nodes for tenderness and enlargement.
While not diagnostic of PTA itself, these tests provide supportive evidence of infection and assess the patient's general status.
- Complete Blood Count (CBC): Often reveals leukocytosis (elevated white blood cell count) with a left shift (increased neutrophils), indicating a bacterial infection.
- C-Reactive Protein (CRP) / Erythrocyte Sedimentation Rate (ESR): These inflammatory markers will typically be elevated, reflecting systemic inflammation.
- Rapid Strep Test / Throat Culture: To identify the presence of Streptococcus pyogenes if the patient can tolerate a swab. This confirms the bacterial etiology but does not distinguish between simple tonsillitis and an abscess.
Imaging is not always necessary if the clinical diagnosis is clear and the patient has minimal trismus. However, it is especially valuable in cases of:
- Uncertain Diagnosis: When clinical findings are ambiguous or atypical.
- Severe Trismus: When a good physical examination is hindered by the patient's inability to open their mouth.
- Concern for Deeper Space Infection: To differentiate PTA from a parapharyngeal or retropharyngeal abscess, which requires different management.
- Abscess Localization: To guide needle aspiration or incision and drainage, especially in pediatric patients or if multiple attempts at drainage have failed.
- Intraoral Ultrasound:
- Method: A small ultrasound probe is placed in the mouth.
- Advantage: Non-invasive, no radiation, can differentiate between cellulitis and an abscess (solid vs. fluid collection), and can guide needle aspiration in real-time. This is gaining favor in many emergency departments.
- Computed Tomography (CT) Scan with Contrast:
- Method: Provides cross-sectional images of the neck and pharynx.
- Advantage: Offers excellent anatomical detail, clearly delineates the extent of the abscess, identifies if the infection has spread to deeper neck spaces, and is useful for surgical planning. It can definitively confirm the presence and location of an abscess.
- Disadvantage: Involves radiation exposure.
- Method: A needle is inserted into the suspected bulging area to aspirate pus.
- Purpose: The successful aspiration of pus confirms the diagnosis of an abscess. It is also the initial therapeutic step.
- Culture: The aspirated pus should be sent for Gram stain and culture to identify the causative organisms and determine antibiotic sensitivity.
- Acute Tonsillitis (Severe): While PTA often stems from tonsillitis, simple tonsillitis generally presents with bilateral tonsillar swelling and exudates. Trismus, uvular deviation, and a distinct "hot potato" voice are typically absent or much less pronounced in uncomplicated tonsillitis. The pain, while significant, is usually not as unilaterally intense as in PTA.
- Key Distinction: No localized collection of pus in the peritonsillar space.
- Peritonsillar Cellulitis: This is an inflammatory stage before pus formation in the peritonsillar space. Patients have similar symptoms to PTA (severe sore throat, dysphagia, sometimes trismus), but on examination, there is marked erythema and swelling without the distinct bulging of an abscess or uvular deviation. Imaging (like ultrasound or CT) can differentiate cellulitis from a true abscess by showing inflammation without a distinct fluid collection.
- Key Distinction: Inflammation and swelling of the tissues without a defined pocket of pus.
- Epiglottitis: A life-threatening condition characterized by inflammation and swelling of the epiglottis. Key symptoms include rapid onset of sore throat, severe dysphagia, drooling, high fever, and stridor (a high-pitched inspiratory sound indicating airway obstruction). Patients often lean forward in a "sniffing" or tripod position. Trismus and uvular deviation are not features.
- Key Distinction: Airway obstruction with stridor; swelling is primarily of the epiglottis, not the peritonsillar area.
- Retropharyngeal Abscess: A collection of pus in the space behind the pharynx, more common in young children. Symptoms include high fever, severe sore throat, difficulty swallowing, drooling, and neck stiffness (torticollis). On examination, there may be bulging of the posterior pharyngeal wall. Trismus and uvular deviation are usually absent. Imaging (CT scan) is essential for diagnosis.
- Key Distinction: Abscess is located posterior to the pharynx, not lateral to the tonsil; typically presents with neck stiffness.
- Parapharyngeal Abscess: A deeper and more dangerous infection in the space lateral to the pharynx. Symptoms can include severe sore throat, fever, difficulty swallowing, and often external neck swelling and tenderness, particularly along the sternocleidomastoid muscle. Trismus can be present. Swelling in the lateral pharyngeal wall may be observed, but not the specific peritonsillar bulging and uvular deviation of PTA. CT scan is the diagnostic tool.
- Key Distinction: Deeper neck infection with external neck swelling; swelling is in the lateral pharyngeal wall, not specific peritonsillar bulging.
- Mononucleosis (Infectious Mononucleosis): Caused by the Epstein-Barr virus, it can cause severe tonsillitis with massive bilateral tonsillar enlargement and exudates, along with fatigue, fever, and generalized lymphadenopathy. Splenomegaly is also common. While it can cause significant pharyngeal pain and dysphagia, it does not typically lead to the distinct unilateral bulging and uvular deviation of a PTA. A Monospot test or EBV serology confirms the diagnosis.
- Key Distinction: Viral etiology, bilateral tonsillar enlargement, generalized symptoms (fatigue, splenomegaly), absence of localized peritonsillar bulging.
- Deep Neck Space Infections (General): These are a broader category that includes retropharyngeal and parapharyngeal abscesses. They can present with severe sore throat, fever, and neck pain/swelling. Differentiation from PTA is crucial as they can involve vital structures and have a higher mortality rate. Imaging is essential.
- Key Distinction: More extensive and deeper infections requiring specific imaging and management.
- Dental Abscess (Periapical or Periodontal): An infection originating from a tooth. While it can cause significant facial and jaw pain, swelling, and sometimes trismus, the pain is typically localized to the tooth/jaw, and the pharyngeal examination will not show peritonsillar bulging or uvular deviation.
- Key Distinction: Originates from a dental source; pharyngeal examination is normal for PTA signs.
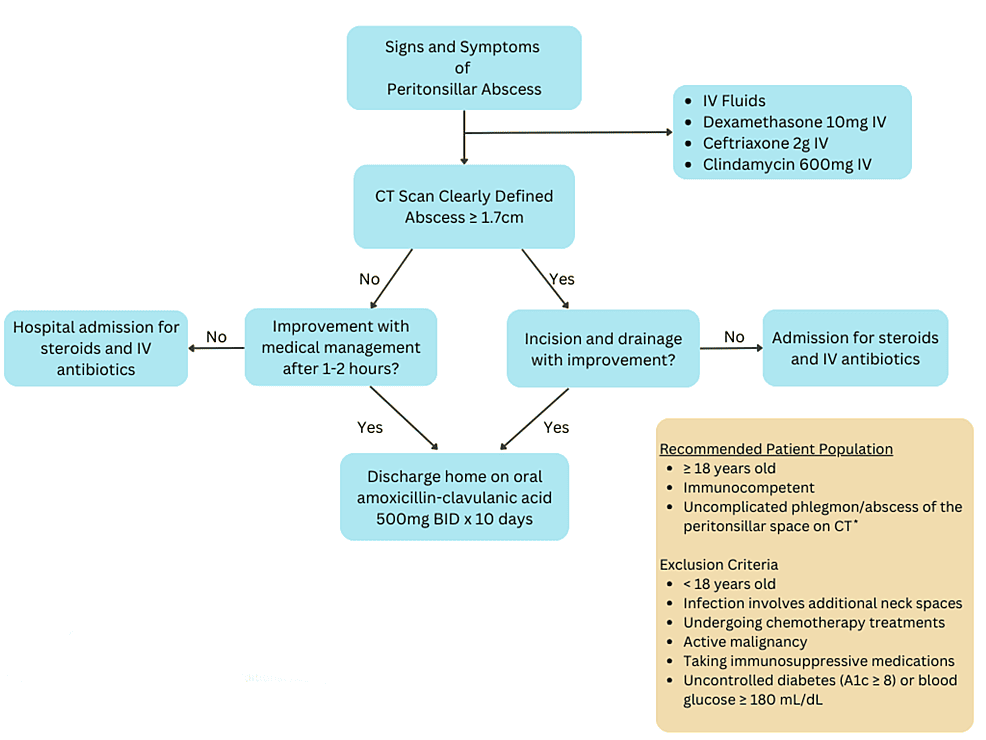
The management of a peritonsillar abscess (PTA) aims to relieve symptoms, eradicate the infection, prevent complications, and often involves both surgical (drainage) and medical (antibiotic) interventions.
- To drain the abscess
- Promote healing by relieving symptoms & treating the cause
- Prevent complications
- The patient is admitted in surgical ward & on complete bed rest
- Baseline vital observations are taken and recorded
- In severe cases, where the patient’s airway is affected, oxygen therapy is provided.
- Pain is managed with analgesics like diclofenac 75 mgs or tramadol 50mgs start.
- General and systemic examination is done, to rule out other health problems.
- After this, an iv line is secured and intravenous fluids are administered eg dextrose alternate with normal saline are administered to maintain the body fluids
- Antibiotics like penicillin may be given to control the spread of infection before the operation
- Assessment: The first and most important step is to assess the patient's airway. Significant swelling can compromise the airway, especially in children.
- Intervention: If there is any sign of impending airway obstruction (e.g., stridor, severe respiratory distress), urgent medical intervention (e.g., intubation, tracheostomy) may be necessary before addressing the abscess itself.
- Explain to the patient what is going to happen
- Gaining an informed consent from the patient is very essential.
- Pass an NGT to help in feeding after surgery.
- Oral care is performed to minimise infection after surgery.
Removing the pus provides immediate relief and allows the infection to resolve. This can be achieved through:
- Needle Aspiration:
- Method: A small-gauge needle attached to a syringe is inserted into the most prominent bulging part of the abscess, and pus is aspirated.
- Advantages: Less invasive, can be done in an outpatient setting, quick, and can be repeated if necessary. Often performed under local anesthesia.
- Disadvantages: May not completely drain all loculations of pus, potentially requiring repeat aspirations.
- Guidance: Can be guided by intraoral ultrasound for enhanced safety and efficacy.
- Pus Culture: The aspirated pus should always be sent for Gram stain and culture to identify the causative organisms and their antibiotic sensitivities.
- Incision and Drainage (I&D):
- Method: A small incision is made in the most fluctuant (bulging) part of the abscess, allowing the pus to drain freely. A small hemostat may be used to gently open the incision further.
- Advantages: Provides more complete drainage than aspiration.
- Disadvantages: More invasive, carries a slightly higher risk of bleeding.
- Anesthesia: Often performed under local anesthesia, but general anesthesia may be considered for uncooperative patients, severe trismus, or young children.
- Tonsillectomy (Quinsy Tonsillectomy):
- Method: Removal of the tonsil and the associated abscess.
- Indications:
- Historically, this was a more common acute treatment.
- Now, it is often reserved for specific situations:
- Failure of needle aspiration or I&D.
- Recurrent PTA.
- Existing indications for elective tonsillectomy (e.g., recurrent severe tonsillitis).
- Patients with significant bleeding risk where conventional drainage is more hazardous.
- Advantages: Eliminates the source of the abscess and prevents recurrence.
- Disadvantages: More invasive procedure, longer recovery time, and higher risk of bleeding compared to aspiration or I&D.
- Suction for oral secretions to prevent aspiration.
- Fluid resuscitation as necessary i.e I.V N/S
- Anti-pyretics and analgesics are prescribed and administered
- Bleeding is prevented by gentle handling of the patient avoiding coughing, laughing, and opening the mouth widely.
- Soft food and drinks can be tried later.
- Oral hygiene is maintained until full recovery.
- Antibiotics are administered as prescribed to prevent infection.
- Nsaids like ibuprofen are administered to control inflammation and fever.
- IV benzyl penicillin 2 mu 6 hly for 48hrs then switch to Amoxil 500mgs tds for 7days or
- Alternative iv ceftriaxone 1 g od for 7 days
- Children 50mg/kg iv
- Plus Iv metronidazole 500mg 8hrly .if unable to take oral fluids, set up an IV drip of Normal saline
- Daily routine Nursing care is provided till the patient is fit for discharge.
- Advice:
- Early treatment for streptococcal throat.
- Oral hygiene.
Antibiotics are an essential component of treatment, whether or not drainage is performed, to combat the bacterial infection.
- Initial Empiric Therapy:
- Coverage: Broad-spectrum antibiotics covering both aerobic and anaerobic bacteria are initiated immediately after diagnosis, often intravenously due to the severity and difficulty swallowing.
- Common Choices: Penicillin-based antibiotics (e.g., ampicillin-sulbactam, clindamycin for penicillin-allergic patients) are frequent first-line choices given the prevalence of Group A Strep and anaerobes. Metronidazole can be added for enhanced anaerobic coverage.
- Culture-Guided Therapy:
- Adjustment: Once culture and sensitivity results are available from the aspirated pus, the antibiotic regimen can be narrowed or adjusted to target the specific pathogens more effectively.
- Duration: Treatment typically continues for 10-14 days to ensure complete eradication of the infection.
- Pain Management:
- Medication: Oral or intravenous analgesics (e.g., NSAIDs, opioids if necessary) are important for pain relief, especially post-drainage.
- Hydration:
- Importance: Due to odynophagia and fever, patients are often dehydrated. Intravenous fluids are given initially, followed by oral fluids once swallowing improves.
- Oral Hygiene:
- Method: Gentle warm saline gargles (for older children/adults) can help soothe the throat and maintain cleanliness.
- Steroids:
- Role: A short course of corticosteroids (e.g., dexamethasone) can sometimes be given to reduce inflammation and swelling, which can improve trismus and facilitate swallowing. This is typically used as an adjunct to drainage and antibiotics.
- Hospitalization: Often required for initial management, especially for severe cases, dehydration, significant airway concern, or if I&D is performed. IV antibiotics and fluids can be administered.
- Outpatient: Once stable, well-hydrated, able to take oral medications, and showing signs of improvement, patients can often be discharged to complete their antibiotic course at home, with clear instructions for follow-up.
Complications from a peritonsillar abscess can range from bothersome to life-threatening, stemming primarily from the local spread of infection and the mass effect of the abscess.
- Airway Obstruction: The significant swelling and displacement of the soft palate and uvula can physically impede the flow of air. Edema can also extend into the laryngeal region.
- Spread of Infection (Deep Neck Space Infections):
- The peritonsillar space is adjacent to several other potential spaces in the neck, and infection can spread to these areas.
- Parapharyngeal Abscess: Infection extending laterally from the peritonsillar space into the parapharyngeal space.
- Retropharyngeal Abscess: Less common from PTA, but possible if the infection tracks posteriorly into the retropharyngeal space.
- Mediastinitis: If a deep neck infection (e.g., parapharyngeal or retropharyngeal abscess) ruptures or spreads downwards into the chest cavity (mediastinum).
- The peritonsillar space is adjacent to several other potential spaces in the neck, and infection can spread to these areas.
- Internal Jugular Vein Thrombophlebitis (Lemierre's Syndrome): Infection from the peritonsillar or parapharyngeal space can spread to the internal jugular vein, causing inflammation and clot formation. Often caused by Fusobacterium necrophorum.
- Carotid Artery Erosion/Rupture: While rare, particularly aggressive or prolonged infection in the parapharyngeal space can erode into the wall of the carotid artery, leading to life-threatening hemorrhage.
- Aspiration Pneumonia: Due to severe dysphagia and drooling, there is a risk of aspirating saliva, food, or even pus into the lungs, leading to pneumonia.
- Sepsis / Septic Shock: Uncontrolled bacterial infection can lead to a systemic inflammatory response, culminating in sepsis and, in severe cases, septic shock with multi-organ dysfunction.
- Recurrence: While not a "complication" in the same acute sense, inadequate drainage or failure to treat the underlying cause can lead to repeat episodes of peritonsillar abscess.
- Dehydration: Severe odynophagia (painful swallowing) makes it very difficult for patients to consume adequate fluids, leading to dehydration.
- Persistent Symptoms/Pain: If drainage is incomplete or antibiotics are ineffective, the abscess may not resolve fully, leading to prolonged pain and discomfort.
Nursing care for a patient with a peritonsillar abscess focuses on managing symptoms, preventing complications, promoting recovery, and providing education.
- Related to: Pharyngeal swelling, pain, accumulated secretions, potential for airway obstruction.
- Defining Characteristics: Stridor, dyspnea, muffled voice ("hot potato" voice), drooling, restlessness, anxiety.
| Intervention | Rationale |
|---|---|
| Monitor Respiratory Status Continually | Early detection of changes in breathing patterns, rate, depth, presence of stridor, or increased work of breathing is paramount for preventing life-threatening airway compromise. |
| Position for Optimal Airway Patency | Elevate the head of the bed to a semi-Fowler's or high-Fowler's position to promote lung expansion and reduce pressure on the airway from pharyngeal swelling. |
| Assess for Trismus and Uvular Deviation | These are key indicators of the severity of the abscess and its potential impact on airway patency and ability to manage secretions. |
| Have Emergency Airway Equipment Readily Available | Be prepared for immediate intervention (e.g., intubation tray, tracheostomy kit, oxygen, suction) if acute airway obstruction occurs. |
| Encourage Effective Coughing and Secretion Management | If the patient is able, encourage gentle coughing or swallowing secretions. Provide suction as needed for drooling or excessive oral secretions. |
| Administer Oxygen as Prescribed | To maintain adequate oxygen saturation and reduce respiratory effort. |
- Related to: Inflammatory process, tissue swelling, nerve irritation, surgical intervention (drainage).
- Defining Characteristics: Patient verbalization of pain (severe sore throat, ear pain), facial grimacing, guarding behavior, difficulty swallowing, restlessness, increased heart rate/blood pressure.
| Intervention | Rationale |
|---|---|
| Assess Pain Characteristics Regularly (PQRST method) | Obtain a comprehensive understanding of the pain's nature, intensity, and location to guide effective management. Note if pain is unilateral. |
| Administer Analgesics as Prescribed | Provide scheduled and PRN pain medication (e.g., NSAIDs, opioids) to keep pain at a manageable level, allowing for rest and improved comfort. |
| Provide Non-Pharmacological Pain Relief | Offer cool compresses to the neck, encourage quiet environment, and provide distractions to complement pharmacological interventions. |
| Educate on Importance of Pain Control | Explain that adequate pain control improves ability to swallow, facilitates rest, and reduces anxiety. |
| Monitor Effectiveness of Pain Interventions | Reassess pain levels after administering interventions to ensure they are providing sufficient relief. |
- Related to: Inability to swallow due to severe pain (odynophagia) and dysphagia, fever, increased metabolic demands.
- Defining Characteristics: Dry mucous membranes, decreased urine output, poor skin turgor, increased heart rate, low blood pressure, patient reports of thirst.
| Intervention | Rationale |
|---|---|
| Monitor Hydration Status Closely | Track intake and output, assess skin turgor, mucous membranes, urine specific gravity, and daily weights. |
| Administer Intravenous Fluids as Prescribed | Provide necessary hydration and electrolytes until the patient can tolerate oral fluids. |
| Encourage Oral Fluid Intake as Tolerated | Offer small, frequent sips of cool, non-acidic liquids (e.g., water, clear broth, diluted juices) once swallowing improves. Avoid extremely hot or cold liquids initially. |
| Educate Patient on Signs of Dehydration | Empower the patient to recognize and report symptoms, promoting proactive self-care. |
- Related to: Pain upon swallowing, fear of swallowing, nausea/vomiting from antibiotics, general malaise, increased metabolic needs due to infection.
- Defining Characteristics: Weight loss, refusal to eat, patient reports of inadequate intake, weakness.
| Intervention | Rationale |
|---|---|
| Assess Nutritional Status | Evaluate current dietary intake, weight changes, and presence of any nausea/vomiting. |
| Provide Small, Frequent, Soft, Bland Meals | Easier to swallow and less likely to irritate the inflamed throat. Examples include mashed potatoes, yogurt, pureed soups. |
| Encourage High-Calorie, High-Protein Supplements | To meet increased metabolic demands and prevent further weight loss. |
| Collaborate with Dietary Services | Ensure appropriate meal planning that considers patient preferences and tolerance. |
| Monitor for Nausea and Administer Antiemetics as Prescribed | To improve appetite and ability to eat. |
- Related to: Bacterial infection, incomplete drainage, non-adherence to antibiotic regimen.
- Defining Characteristics: Elevated WBC count, fever, chills, purulent drainage, patient statements of non-adherence.
| Intervention | Rationale |
|---|---|
| Administer Antibiotics as Prescribed (Dose, Route, Frequency) | Ensure therapeutic levels to eradicate the bacterial infection and prevent complications. Emphasize completing the entire course. |
| Monitor for Signs of Infection Spread | Regularly assess for worsening pain, increasing swelling in the neck or face, new onset of fever/chills, changes in respiratory status, or signs of deeper neck space infection. |
| Educate on Wound Care (Post-Drainage) | Instruct on proper oral hygiene, gentle gargles with warm saline, and reporting any foul-smelling discharge. |
| Patient Education on Completing Antibiotic Course | Stress the importance of taking all prescribed antibiotics, even if feeling better, to prevent recurrence and antibiotic resistance. |
| Advise on Follow-Up Care | Emphasize the need for follow-up appointments to ensure complete resolution and to discuss potential tonsillectomy for recurrent cases. |
- Related to: Acute illness, severe pain, difficulty breathing, fear of choking, uncertainty about prognosis.
- Defining Characteristics: Verbalization of anxiety/fear, restlessness, irritability, increased heart rate, difficulty sleeping.
| Intervention | Rationale |
|---|---|
| Provide Clear and Concise Information | Explain procedures, treatment plan, expected outcomes, and how to manage symptoms in an understandable manner. |
| Maintain a Calm and Reassuring Demeanor | Reduces patient anxiety and promotes trust. |
| Ensure Adequate Pain Control and Airway Patency | Addressing immediate physical discomforts directly reduces anxiety. |
| Encourage Presence of Supportive Family/Friends | Provides emotional support to the patient. |
| Allow for Questions and Expression of Feelings | Active listening and addressing concerns can alleviate fear. |

The work is well organized, however other conditions are not opening.
Would you be specific about the conditions that aren’t opening.
What investigations can be done?
1. Physical Examination: A thorough physical examination of the throat, neck, and oral cavity is essential to assess the presence of an abscess. The doctor will examine the tonsils, check for swelling, redness, and the presence of pus or fluctuance (a soft, fluid-filled area).
2. Throat Swab: A swab may be taken from the throat to identify the causative organism. This helps guide appropriate antibiotic therapy.
3. Complete Blood Count (CBC): A CBC test is performed to assess the white blood cell count. In cases of infection, the white blood cell count is often elevated, indicating an inflammatory response.
4. Ultrasound: An ultrasound may be performed to assess the size and location of the abscess. It can help differentiate between a peritonsillar abscess and other possible causes of throat pain.
5. CT Scan: In some cases, a computed tomography (CT) scan of the neck may be ordered. It provides detailed imaging of the area and helps determine the extent and location of the abscess.
6. Blood Cultures: Blood cultures may be obtained to identify the causative organism and guide appropriate antibiotic therapy, especially in severe or complicated cases.
this is great flow of information thank you
State the actual and potential nursing diagnosis, then nursing interventions and management of peritonsilor.
What are the complications of perritonsal abscess
Airway obstruction: The abscess can grow in size and obstruct the airway, leading to difficulty breathing and potentially life-threatening situations.
Cellulitis: The infection can spread to the surrounding tissues, causing cellulitis, which is a painful and potentially serious condition.
Sepsis: If the infection spreads to the bloodstream, it can lead to sepsis, a potentially life-threatening condition characterized by a systemic inflammatory response.
Ludwig’s angina: This is a severe form of cellulitis that affects the floor of the mouth and can lead to swelling and potential airway compromise.
Lemierre’s syndrome: This is a rare but serious complication in which the infection spreads from the tonsils to the internal jugular vein, leading to septic thrombophlebitis and potential septic emboli.
Mediastinitis: In severe cases, the infection can spread to the mediastinum, the area in the middle of the chest, leading to a potentially life-threatening condition called mediastinitis.
Retropharyngeal abscess: In some cases, the infection can spread to the retropharyngeal space, leading to the formation of an abscess in this area, which can cause difficulty swallowing and potential airway compromise.
What are the complications of peritonsillar abscess
Hy, did u pass nursing diploma, hw was it
good notices
thanks