Table of Contents
TogglePERITONSILLAR ABSCESS
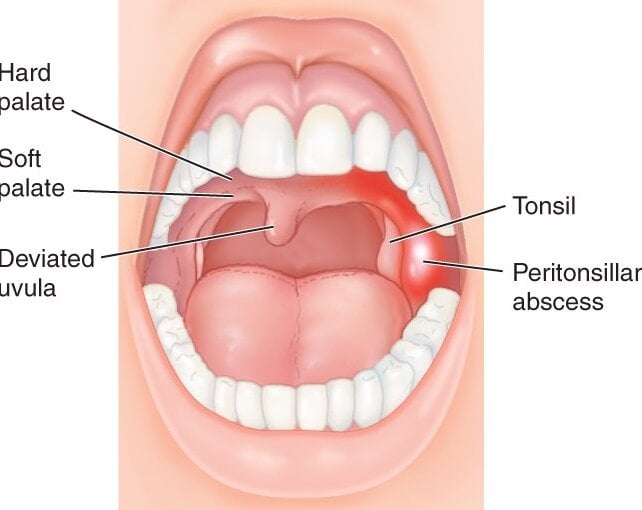
Peritonsillar Abscess (Quincy) is defined as an abscess between the tonsil capsule and the lateral wall of the pharynx.
Peritonsillar abscess (Quincy) is a bacterial streptococcal infection that usually begins as a complication of untreated tonsillitis(often mild).
It generally involves a pus-filled pocket that forms near one of your tonsils. It is a collection of pus around the tonsils. It usually begins as a complication of untreated streptococcal throat or tonsillitis infection
- If left untreated, the infection can spread deep into the neck and chest. Rarely in adults.
CAUSES OF PERITOSILLAR ABSCESS
Peritonsillar abscesses usually occur as a complication of tonsillitis. If the infection breaks out of a tonsil and spreads to the surrounding area, an abscess can form. Peritonsillar abscesses are becoming less common due to the use of antibiotics in the treatment of strep throat and tonsillitis.
Peritonsillar abscesses are caused by bacteria and these include,
- Streptococcus pyogenes (the same that causes strep throat & tonsillitis
- Fuso bacteria necrophorum (causes mastoiditis, sinusitis &meningitis
- Staphylococcus
- Haemophilus
Mononucleosis (commonly referred to as mono) can also cause peritonsillar abscesses, as well as tooth and gum infections. In much rarer cases, it’s possible for peritonsillar abscesses to occur without an infection. This is generally due to inflammation of the Weber glands. These glands are under the tongue and produce saliva.
CLINICAL PRESENTATION
- Inability to open the mouth, salvation and dribbling
- Severe throat pain
- Dysphagia
- Bad mouth odor (Halitosis)
- Ptylism (excessive salvation)
- Thickened muffled(un clear) speech
- Ear pain -Fever, headache, malaise, rigors
- Enlarged cervical lymph nodes
- Tonsil and soft palate are reddish & edematous
- Swelling pushing the uvula to opposite side (May be pointing(bulging collection of pus)
- Otalgia (earache)
- Enlarged cervical lymph nodes
- Difficult in swallowing
- Impaired speech
- Swelling of the neck and face
- Difficulty swallowing saliva (drooling)
- Swelling of the face or neck
Investigations
- Physical Examination: A thorough physical examination of the throat, neck, and oral cavity is essential to assess the presence of an abscess. The doctor will examine the tonsils, check for swelling, redness, and the presence of pus or fluctuance (a soft, fluid-filled area).
- Throat Swab: A swab may be taken from the throat to identify the causative organism. This helps guide appropriate antibiotic therapy.
- Complete Blood Count (CBC): A CBC test is performed to assess the white blood cell count. In cases of infection, the white blood cell count is often elevated, indicating an inflammatory response.
- Ultrasound: An ultrasound may be performed to assess the size and location of the abscess. It can help differentiate between a peritonsillar abscess and other possible causes of throat pain.
- CT Scan: In some cases, a computed tomography (CT) scan of the neck may be ordered. It provides detailed imaging of the area and helps determine the extent and location of the abscess.
- Blood Cultures: Blood cultures may be obtained to identify the causative organism and guide appropriate antibiotic therapy, especially in severe or complicated cases.
Management Of Peritonsillar
Aims:
- To drain the abscess
- Promote healing by relieving symptoms & treating the cause
- Prevent complications
Admission
- The patient is admitted in surgical ward& on complete bed rest
- Baseline vital observations are taken and recorded
- In severe cases, where the patient’s airway is affected, oxygen therapy is provided.
- Pain is managed with analgesics like diclofenac 75 mgs or tramadol 50mgs start.
- General and systemic examination is done, to rule out other health problems.
- After this, an iv line is secured and intravenous fluids are administered eg dextrose alternate with normal saline are administered to maintain the body fluids
- Antibiotics like penicillin may be given to control the spread of infection before the operation
PRE-OPERATIVE CARE.
- Explain to the patient what is going to happen
- Gaining an informed consent from the patient is very essential.
- Pass an NGT to help in feeding after surgery.
- Oral care is performed to minimise infection after surgery.
IN OPERATING THEATRE;
- Incision and drainage of the abscess is done.
- Tonsillectomy is performed (simultaneous tonsillectomy with open abscess drainage and oral packing to control bleeding.
ON WARD
- Suction for oral secretions to prevent aspiration.
- Fluid resuscitation as necessary i.e I.V N/S
- Anti-pyretics and analgesics are prescribed and administered
- Bleeding is prevented by gentle handling of the patient avoiding coughing, laughing, and opening the mouth widely.
- Soft food and drinks can be tried later.
- Oral hygiene is maintained until full recovery.
- Antibiotics are administered as prescribed to prevent infection.
- Nsaids like ibuprofen are administered to control inflammation and fever.
- IV benzyl penicillin 2 mu 6 hly for 48hrs then switch to Amoxil 500mgs tds for 7days or
- Alternative iv ceftriaxone 1 g od for 7 days
Children 50mg/kg iv
- Plus Iv metronidazole 500mg 8hrly .if unable to take oral fluids, set up an IV drip of Normal saline
- Daily routine Nursing care is provided till the patient is fit for discharge.
Advice:
- Early treatment for streptococcal throat.
- Oral hygiene.
NURSING CARE PLAN.
| Assessment | Diagnosis | Planning (Goals/Expected Outcomes) | Implementation | Rationale | Evaluation |
|---|---|---|---|---|---|
| Inability to open the mouth, salvation and dribbling, severe throat pain, dysphagia, bad mouth odor (Halitosis), Ptylism (excessive salvation), thickened muffled(un clear) speech. | Impaired Oral Mucous Membrane related to peritonsillar abscess evidenced by difficulty swallowing, thickened speech, excessive salvation, and bad mouth odor. | Maintain oral hygiene and alleviate discomfort. | – Administer prescribed antibiotics and analgesics. – Encourage regular oral care, including gentle rinsing with saline solution. – Provide pain management interventions (e.g., cold compresses). | – Antibiotics target the bacterial infection. – Regular oral care prevents secondary infections and promotes comfort. – Pain management interventions reduce discomfort. | Maintained oral hygiene, reduced discomfort. |
| Fever, headache, malaise, rigors, enlarged cervical lymph nodes. | Hyperthermia related to systemic infection evidenced by fever, malaise, headache, and rigors. | Reduce fever and promote comfort. | – Administer antipyretic medication as prescribed. – Encourage adequate fluid intake. – Provide cooling measures (e.g., tepid sponging). | – Antipyretic medication helps lower fever. – Adequate fluid intake prevents dehydration. – Cooling measures aid in reducing body temperature. | Fever reduced, improved comfort. |
| Swelling pushing the uvula to the opposite side, otalgia, and difficulty in swallowing. | Impaired Swallowing related to swelling and pain evidenced by difficulty swallowing and drooling. | Improve swallowing function and reduce pain. | – Encourage small, frequent meals and fluids. – Administer analgesic medication as prescribed. – Monitor and record intake and output. | – Small, frequent meals are easier to swallow. – Analgesic medication helps relieve pain. – Monitoring intake and output prevents dehydration. | Improved swallowing function, reduced pain. |
| Swelling of the neck and face. | Disturbed Body Image related to visible swelling evidenced by patient distress. | Support patient’s body image and self-esteem. | – Provide emotional support and encourage expression of feelings. – Educate the patient about the temporary nature of the swelling. – Collaborate with the healthcare team to explore potential interventions to reduce visible swelling. | – Emotional support and education reduce anxiety and distress.<br>- Understanding the temporary nature of the swelling helps manage patient expectations. – Exploring interventions shows commitment to addressing patient concerns. | Enhanced body image and self-esteem. |

The work is well organized, however other conditions are not opening.
Would you be specific about the conditions that aren’t opening.
What investigations can be done?
1. Physical Examination: A thorough physical examination of the throat, neck, and oral cavity is essential to assess the presence of an abscess. The doctor will examine the tonsils, check for swelling, redness, and the presence of pus or fluctuance (a soft, fluid-filled area).
2. Throat Swab: A swab may be taken from the throat to identify the causative organism. This helps guide appropriate antibiotic therapy.
3. Complete Blood Count (CBC): A CBC test is performed to assess the white blood cell count. In cases of infection, the white blood cell count is often elevated, indicating an inflammatory response.
4. Ultrasound: An ultrasound may be performed to assess the size and location of the abscess. It can help differentiate between a peritonsillar abscess and other possible causes of throat pain.
5. CT Scan: In some cases, a computed tomography (CT) scan of the neck may be ordered. It provides detailed imaging of the area and helps determine the extent and location of the abscess.
6. Blood Cultures: Blood cultures may be obtained to identify the causative organism and guide appropriate antibiotic therapy, especially in severe or complicated cases.
this is great flow of information thank you
State the actual and potential nursing diagnosis, then nursing interventions and management of peritonsilor.
What are the complications of perritonsal abscess
Airway obstruction: The abscess can grow in size and obstruct the airway, leading to difficulty breathing and potentially life-threatening situations.
Cellulitis: The infection can spread to the surrounding tissues, causing cellulitis, which is a painful and potentially serious condition.
Sepsis: If the infection spreads to the bloodstream, it can lead to sepsis, a potentially life-threatening condition characterized by a systemic inflammatory response.
Ludwig’s angina: This is a severe form of cellulitis that affects the floor of the mouth and can lead to swelling and potential airway compromise.
Lemierre’s syndrome: This is a rare but serious complication in which the infection spreads from the tonsils to the internal jugular vein, leading to septic thrombophlebitis and potential septic emboli.
Mediastinitis: In severe cases, the infection can spread to the mediastinum, the area in the middle of the chest, leading to a potentially life-threatening condition called mediastinitis.
Retropharyngeal abscess: In some cases, the infection can spread to the retropharyngeal space, leading to the formation of an abscess in this area, which can cause difficulty swallowing and potential airway compromise.
What are the complications of peritonsillar abscess