Table of Contents
ToggleResuscitation of a Newborn
Resuscitation is a mean of restoring life to a baby from the state of asphyxia.
It is a single intervention of birth asphyxia (Devi, Upendra, and Bard, 2017). Resuscitation is helping a baby to breath.
The first 28 days of life is called neonatal period and incontrovertibly, it is the most vulnerable and high risk time in life because of the highest mortality and morbidity that occur in this period. The day of birth is the riskiest time to a baby (Sajjad, 2012; and WHO, 2015).
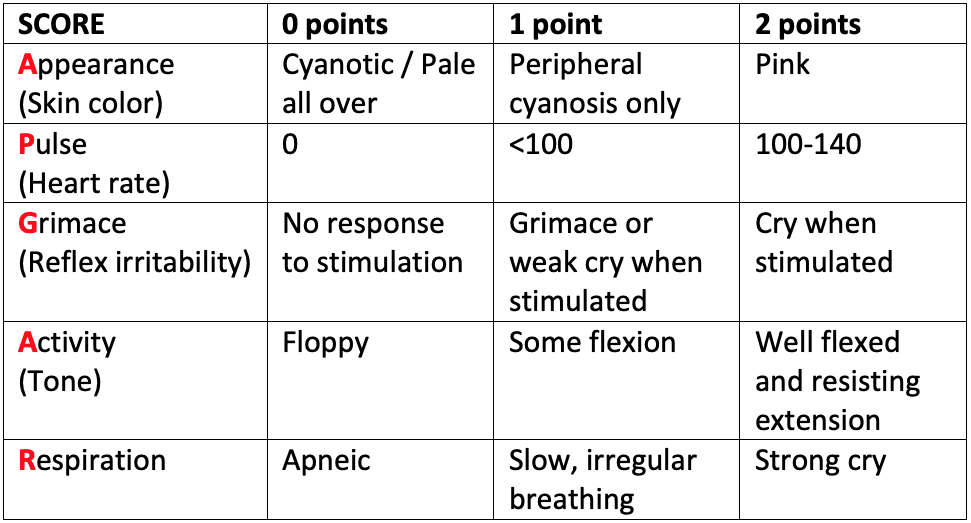
APAGAR SCORE
Aims of Management.
- To initiate and/or restore respiration /breathing
- To prevent infection
- To prevent other complications
- To Prevent hypothermia
Requirements
- A pair of surgical gloves
- Warm baby’s clothes.
- Suction device e.g bulb syringe
- Ventilation bag and mask (ambu bag)
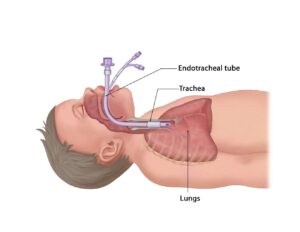
- Endotracheal tube to give oxygen direct to the lungs (size 1mm for full term or 0.5mm preterm babies)
- laryngoscope
- Nasal gastric tube
- 3 Gallipots
- 3 Receivers
- Mothers chart
- Tray containing a gallipot of wet swab, syringes.
- Pediatric stethoscope
- Strapping
- Naso prongs (oxygen catheters)
Drugs
- Naloxone hydrochloride 1mg ampoule 400mg/1ml
- Adrenaline (Epinephrine) 1:1000
- Normal saline 0.9%
- Ringers lactate
- Sodium bicarbonate 4.2%
- Dextrose 10%
- Vitamin K
- Sterile water
Bed side
- Resuscitation table
- Timer (clock watch)
- Light source
- Oxygen source
- Displayed chats for steps
Principles of Management.
- Temperature regulation. Ensure adequate warmth for the baby to prevent hypothermia which leads to decreased metabolic which cause additional stress to the baby.
- Ensure adequate oxygenation to the baby to prevent hypoxia by administration of oxygen and monitoring oxygen perfusion. An endotracheal tube should be inserted and oxygen administered
- Prevention of hypoglycemia by regular monitoring blood glucose and if risk for hypoglycemia is identified administer dextrose as per prescription.
Steps for Resuscitation
TABCs of resuscitation
STEP 1
- Dry the baby, wipe the baby’s mouth with gauze and remove any wet cloth.
STEP 2
Clear the air way by;
- Suck blood or mucus from mouth using a bulb syringe or mucus extractor.
- Position baby’s head in a neutral position with head extended.
- Place a small towel under the shoulders to maintain the position.

STEP 3
Support breathing by;
- Stand at the baby`s head, apply ambu-bag and a small mask to the baby’s face ensuring that the mask covers the face and mouth to form a seal.
- Give five inflation breaths (each 2-3seconds duration).
- Observe response by looking at the chest movements (chest rising) or increase in the heart rate. (if chest does not rise then reapply mask, reposition baby’s head, and suction.)
- Continue ventilating at a rate of 30-40 breathes for a minute.
- Circulation/External Cardiac Massage
- Chest compression should be performed when the heart rate is less than 100b/m and falling inspite adequate ventilation
- If no heart beats are recorded after one minute, do external compressions.
- Wrap your palms around the baby`s chest, placing the thumbs / first finger over the lower part of the sternum.
- Chest is compressed at rate of 100–120 times 1 minute at a ratio of 3 compressions to one ventilation
- Use the thumb to gently compress the chest, depressing it ½ to ¾ inch each time.
- If in 20 minutes the breathing is not established. Consider intubation.
- When the infant has no spontaneous breathing then continuous positive pressure ventilation (CPPV) should be started with bag and mask.
- The rate of chest compressions in one minute should be 90 along with 30 PPVs, (3:1), a total of 120 events.
- If the heart rate is <60, despite of effective ventilation, chest compression and two intravenous doses of adrenaline (Epinephrine), the sodium bicarbonate 4.2% solution (0.5mmol/ml) can be administered using 2–4ml / kg (1-2mmol/ml) by slow intravenous.
Adrenaline (Epinephrine)
- This is indicated if the heart rate is <60, despite 1 min of effective ventilation and chest compression. An initial dose of 0.1-0.3 ml/kg of 1:10,000 solution give i.v. repeated after 3 minutes for a further two doses.
10% dextrose
- (Hypoglycemia is not usually a problem) 3mls/kg i.v via the umbilical vein to correct low blood sugar of <2.5mmol/L
- Volume replacement
- On rare occasions, bradycardia will not respond to volume expansion and bradycardia that does not respond to chest compressions or drugs is suggestive of hypovolemia–0.9% normal saline 10 ml /kg initially via the umbilical vein.
Naloxone hydrochloride
- This is not an emergency drug parse it is a powerful anti-opioid drug used to reverse the effects of maternal narcotic drugs given towards the end of first stage of labour (Preceding 3hours.)
- Dose 0.1–0.2 mg per kilogram body weight intramuscular.
Calcium gluconate
- A dose of 100mg kg body weight and 150 adrenaline 0.1-0.5mg/kg 1 min given for severe bradycardia or cardiopulmonary arrest
- Vitamin K–given prophylaxis against bleeding disorder.
Drugs
- If there is no heart beat after 1 minute of breathing for the baby:
- Inject 0.5 mls of 1;10,000 adrenaline solution intravenously or through the umbilical vein. Give 1 to 2 mls per kilogram body weight of 25% dextrose solution intravenously.
- Continue to monitor response to resuscitation by using APGAR score.
-
- If the baby responds to resuscitation keep the baby warm and transfer to the special unit (NICU).
- If baby is breathing well, keep reassuring the mother
- If baby is breathing well, breast feeding should be encouraged. If no response discontinue resuscitation.


You stated give mls per kg body weight of 25%dextrose solution iv. What is that a mount of mls..?. Thank you very much for that excellent work.
Give 1 to 2 mls per kilogram body weight of 25% dextrose solution intravenously.
Thanks, we really appreciate
Any suggestion to improve delivery of notes.
What is the specific nursing management of neonatal resuscitation
But neonatal resuscitation is a management itself!
The information has helped me learn alot because it’s understandable
I do appreciate
Thanks very much, you make me understand easily
I will not struggle for notes now excellent notes here DNE is gonna be crushable for me
Thanks so much for the detailed explanation.however I suggest for such procedures u drop a video for more clarification.thx👏
I have learnt that resuscitation is a big deal as far as neonatal life is concerned and must be done by a competent skilled personnel who have gotten access to this kind of well elaborate notes ….
Thank you much