Table of Contents
ToggleSPIRITUALITY IN PALLIATIVE CARE
Spirituality is defined as a way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred.
Spirituality means different things to different people. Religion and faith might be part of someone’s spirituality, but spirituality isn’t always religious.
Everyone has spiritual needs throughout their lives whether they follow a religion or not. Spiritual wellbeing is often described as feeling at peace.
Spiritual distress – also called spiritual pain or suffering – can occur when people are unable to find sources of meaning, hope, love, peace, comfort, strength and connection in their life. This distress can also affect their physical and mental health. Terminal illness can often cause spiritual distress in patients as well as their family and friends.
Spiritual needs
Spiritual needs are those needs and expectations which humans have to find meaning, purpose, and value in their life.
- Forgiveness: Needs of being forgiven by God or others; forgiving self, others, and God.
- Relatedness: Need of being related or connected to something, group or community in points of life of a patient.
- Reassurance: Need of removing one’s doubts or fears by cheering up or provision of solace.
- Acceptance: Need of being received by others the way you are
- Peace: Need of being in a state or period in which there is no war.
- Hope: Need of something to happen in future
- Self-esteem: Need to feel good about one’s self achievement.
- Control of your life, behavior, choices
- Dignity: Need of being worthy of respect
- Personal worth: Need of respect from others
- Gratitude: Need of being thankful
Assessment of spiritual needs
- Creating a good rapport to the patient
- Encourage patients to talk about how they’re feeling. Someone might have unmet spiritual needs if they are: searching for meaning, for example asking questions such as ‘Why is this happening?’, ‘Why me?’, ‘Who am I?’ and ‘How will I be remembered?’ becoming more withdrawn and isolated, afraid of being alone, refusing care saying they feel scared or worried.
- Many health and social care professionals find it hard to discuss spirituality with their patients. Some of the reasons for this include: lack of training, not knowing what to say, being concerned about saying something inappropriate.
- Using spiritual assessment tools.
Spiritual assessment tools
a) HOPE tool
- H – Hope: Requires assessing the patient’s sources of hope, strength, comfort and peace.
- O – Organized religion: Requires assessing the patient’s religion or faith and how it is important to the patient.
- P – Personal spirituality and practices: Involves assessing the patient’s sense of meaning and purpose in life and how it adds sense to his/her identity.
- E – Effects on medical care and of life issues: Involves assessing how medical care of the patients affects his purpose and meaning of life.
a) FICA tool
- F – Faith, belief, meaning: Involves determining whether or not the patient identities with a particular belief system of spirituality at all
- I – importance and influence: Involving understanding the importance of spirituality in a patient’s life and the influence on health care decisions.
- C – Community: It involves finding out if the patient is part of a religious or spiritual community or if they rely on their community for support
- A – Address/Action: Involves addressing spiritual issues of the patient with regards to caring for the patient.
Questions to ask under each spiritual assessment tool:
a) HOPE tool:
H – Hope:
- What are the sources of hope, strength, comfort, and peace in your life?
- How do these sources of hope help you cope with challenging situations?
- Can you provide examples of times when hope has played a significant role in your life?
O – Organized religion:
- Do you follow a particular religion or faith?
- How important is your religion or faith to you?
- In what ways does your religion or faith provide support and guidance in your life?
P – Personal spirituality and practices:
- What activities or practices give you a sense of meaning and purpose in life?
- How do these practices contribute to your overall well-being?
- Can you share any experiences where these practices have had a positive impact on your life?
E – Effects on medical care and life issues:
- Has your illness affected your ability to engage in activities that give your life meaning and purpose?
- Are there any specific spiritual practices or beliefs that we should consider when providing your care?
- Would you like to discuss any concerns or questions related to spirituality and its connection to your medical care?
b) FICA tool:
F – Faith, belief, meaning:
- Do you identify with a particular belief system or spirituality?
- How does your spirituality or belief system influence your daily life?
- Do you find meaning or purpose in your spiritual or religious beliefs?
I – Importance and influence:
- How important is spirituality in your life?
- Have your spiritual beliefs influenced any decisions you’ve made regarding your health or healthcare?
- Do you seek spiritual guidance or support when facing medical challenges?
C – Community:
- Are you part of a religious or spiritual community?
- Do you find support or strength from your community in times of need?
- How does your community contribute to your spiritual well-being?
A – Address/Action:
- How can we address any spiritual concerns or needs you may have during your care?
- Are there any specific ways we can incorporate your spirituality into your treatment plan?
- Would you like assistance in connecting with a spiritual or religious counselor?
Remember to ask these questions with sensitivity and respect, allowing the patient to express their thoughts and beliefs openly.
Spiritual interventions a Nurse can encourage a patient to consider.
Spiritual interventions are tailored to the individual patient’s needs and cultural background.
Respecting one’s own dignity and worth: Recognizing and honoring the value and importance of oneself as a spiritual being.
Developing/using your own spiritual resources: Exploring and utilizing personal beliefs, practices, and strengths to find comfort and support.
Praying and meditating: Engaging in prayer or meditation as a means to connect with one’s spirituality, seek solace, or find guidance.
Joining a prayer group: Participating in a community of individuals who come together to pray and offer mutual support.
Participating in religious services: Attending religious ceremonies or services that align with one’s faith or belief system.
Actively forgiving ‘those who have trespassed against you’: Practicing forgiveness towards others who may have caused harm or hurt, fostering emotional and spiritual healing.
Forgiving your own frailty and mistakes: Extending forgiveness and compassion towards oneself, acknowledging and accepting imperfections.
Creating and nurturing inner peace: Engaging in activities that promote a sense of tranquility and harmony within oneself.
Seeking help from your religious/spiritual adviser: Consulting with a trusted religious or spiritual counselor for guidance, support, and counsel.
Spending time appreciating nature: Connecting with the natural world, finding solace and inspiration in the beauty and serenity of the environment.
Listening to sacred music: Engaging with music that holds spiritual or religious significance, allowing it to uplift and provide comfort.
Surrounding yourself with people who have sound ethical principles: Being in the company of individuals who embody values and principles that align with one’s own spiritual beliefs.
Using gentle humor with oneself and others: Incorporating lightheartedness and humor in a compassionate and respectful manner to promote well-being and positive relationships.
Actively striving for wholeness: Engaging in personal growth and self-care practices that foster physical, emotional, and spiritual well-being.
Personal awareness
Personal awareness is the ability to know and understand oneself, including one’s values, beliefs, strengths, weaknesses, and emotions.
It is an important skill for anyone who provides palliative care, as it allows us to be more sensitive to the needs of our patients and their families.
Benefits of personal awareness in palliative care:
- We are more in charge of our lives. When we know ourselves well, we are better able to make decisions that are in our best interests. This is especially important when we are providing care to others, as we need to be able to set boundaries and take care of ourselves.
- We develop greater sensitivity to our own feelings and to those of others. When we are aware of our own emotions, we are better able to understand and respond to the emotions of others. This is essential in palliative care, as we are often dealing with people who are experiencing a wide range of emotions, such as grief, fear, and anger.
- Reflecting on our own experiences in life can help us to help others. When we reflect on our own experiences, we can gain insights that can help us to understand the experiences of others. This can be especially helpful when we are working with people who are facing challenges that we have faced ourselves.
- We are better able to resolve our own problems or life issues, if we know ourselves well. When we know ourselves well, we are better able to identify and address our own problems. This can help us to be more effective in our work, as we will be less likely to be distracted by our own personal issues.
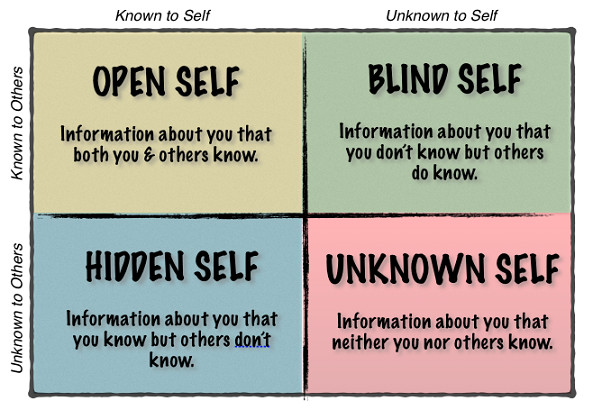
The Johari window: model of self-awareness
The Johari window is a model that is useful for understanding oneself and others. It was developed by Joseph Luft and Harry lngham in the 1950’s. They devised four windows that represent the areas of the mind and it’s functioning within us and others.
(i) Open area:
This is the area of an individual that is known to self and others.
- Examples of information that might be in the open area include:
- Your name, age, and occupation.
- Your hobbies and interests.
- Your likes and dislikes.
- Your strengths and weaknesses.
- Your values and beliefs.
The aim should be to develop this area for every person as it leads to effectiveness and productiveness in the way we handle patients and families receiving palliative care.
Here good communication and cooperation occur, free from distractions, mistrust confusion and misunderstanding.
(ii) Blind area.
This is the area of an individual that is unknown to self but is known to others. ∙ By soliciting feedback from others. the aim should be to reduce this area and thus increase the open area (increase self-awareness)
∙ This area also includes issues that others are deliberately withholding from the person. It includes information that others have observed about the person, but the person themselves is not aware of.
- Examples of information that might be in the blind area include:
- Your body language.
- Your tone of voice.
- Your facial expressions.
- Your habits.
- Your blind spots.
(iii) Hidden area
This is the area of an individual that is known to self but unknown to others and we usually prefer it to remain unknown to others.
It includes information that the person does not want others to know about.
- Examples of information that might be in the hidden area include:
- Your secrets.
- Your fears.
- Your insecurities.
- Your vulnerabilities.
- Your past mistakes.
Represents information, sensitiveness, fears, hidden agendas, manipulative intentions, secrets that one knows but does not reveal
Reducing the hidden areas reduces the potential for confusion, misunderstanding, poor communication, etc. which can all distract from and undermine effectiveness
The extent to which an individual discloses personal feelings and information, and the issues that are disclosed, and to whom, must always be at the individual’s own discretion. Should disclose at a pace and depth that is comfortable for the individual
(iv) Dark area
This is the area of an individual that is unknown to self and unknown to others. This is normally an area of potential for personal growth and development.
∙ Contains information, feelings, latent abilities, aptitudes, experiences that are unknown to the person him/herself and unknown to others in the group.
This is normally an area of potential for personal growth and development.
- Examples of information that might be in the unknown area include:
- Your latent abilities.
- Your aptitudes.
- Your experiences.
- Your potential.
- Your shadow self.
Large unknown areas would typically be expected in younger people, than those who lack experience or self-belief.
Counselling can uncover unknown issues, but this would then be known to the person and by one other rather than by a group. Providing people with the opportunity to try out new things, with no great pressure to succeed, is often a useful way to discover unknown abilities, and thereby reduce the unknown area. ∙ Creating a culture, climate and expectation for self-discovery helps people to fulfill their potential and achieve fore.
Discovery through sensitive communications, active listening and experience will reduce the unknown area.
A guide to developing self-awareness
The following questions are a good guide for better understanding of self.
| Questions | Factors to Consider |
|---|---|
| Where am I in my life journey? | |
| What social and cultural factors influence me? | – Country |
| – Tribe | |
| – Social norms | |
| – Beliefs (cultural, religious, etc.) | |
| – Judgments and principles | |
| From birth, what influences me? | – Family |
| – Family I marry into | |
| – Education | |
| – Opportunities | |
| – Work | |
| – Friends | |
| What do I think about my physical appearance? | – How I see myself |
| – Am I satisfied with my appearance? | |
| What is my image of God? | – Distant or near? |
| – Loving Father or Judge? | |
| – Existing or not? | |
| What are my weaknesses? | – What frightens me? |
| – What makes me angry? | |
| How do I deal with difficult situations? | – At work |
| – At home | |
| – Consider using a model of reflection | |
| What unique gifts, talents, and skills do I bring to | |
| this world? | |
| What gives me meaning and purpose in life? |

