Table of Contents
ToggleUnder Water Seal Drainage
Under water seal drainage is a system that allows drainage of the pleural space using an airtight system to maintain sub-atmospheric intrapleural pressure.
Under water seal drainage is used to remove blood, air, pus, or serous fluid from the pleural cavity after thoracotomy, chest injury, pleural effusion, or pneumothorax.
- The underwater seal acts a one-way valve.
Uses of Under Water Seal Drainage
UWSD are inserted to allow
- drainage of the plural spaces of air, blood or fluid into the pleural cavity, allowing expansion of the lungs and restoration of negative pressure in the thoracic cavity.
- It also prevents backflow of air or fluid into the pleural cavity.
NB: Water seal is important in drainage systems because it acts as a one-way valve as it allows air to exit through the system while preventing air from re-entering the pleural space, which could lead to accumulation of pneumothorax.

3 bottle system
- In a 3-bottle system, a third bottle, called the manometer bottle, is added after the underwater-seal bottle. This manometer bottle has a vent tube under water to regulate the negative pressure generated by suction. The maximum negative pressure (in cm H2O) generated by suction equals to the distance (in cm) this vent tube is below the water line.
- Many single-use composite 3-bottle drainage systems made of plastic are available commercially. The Pleuravac and the Aqua-Seal Dual Drainage systems are some examples.
METHOD OF USE
3-bottle system
- A trap or collection bottle is interposed between the intercostal catheter and the underwater-seal bottle and a third bottle, called the manometer or pressure-regulating bottle, is added after the underwater-seal bottle.
- Modern drains incorporate three separate bottles into one unit.
- Trap bottle = fluid trap or collection bottle, can be independently emptied and allows accurate record of drainage amount.
- Under wate seal bottle = underwater seal drain, maintained at a predetermined level whilst still allowing for drainage of pleural fluid (if bubbling continuously -> bronchopleural fistula).
- Manometer bottle = manometer or pressure-regulating bottle allows suction to be attached and should bubble continuously.
- The maximum negative pressure (in cm H2O) generated by suction equals to the distance (in cm) the vent tube is below the water line (this can be adjusted).
- The negative pressure generated by the vent tube is independent of the amount of pleural drainage that is collected in the trap bottle.
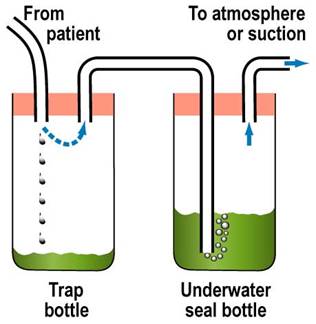
2-bottle system
- The working principle of the 2-bottle system is the same as the 1-bottle system except a trap bottle is placed between the drain tube and the underwater-seal bottle.
- In both the 1-bottle and the 2-bottle system, the vent tube may be connected to a high- volume/low-pressure suction system (e.g., the Vernon-Thompson pump) set at a level of -10 to -20 cm H2O. A low-volume pump (e.g., the Roberts pump) is inappropriate.

1-bottle system
- Chest drain is connected by collecting tubing to a tube approximately 3 cm under water (the seal) in the underwater-seal bottle.
- Another vent tube is open to atmosphere
- Pleural pressure greater than +3 cm water will force air or fluid from the pleural space into the bottle while negative pressure in the pleural space will suck fluid up the tube.
- As long as the underwater-seal bottle is well below the patient (e.g., on the floor beside the patient), the hydrostatic pressure of the fluid column in the tube will counterbalance the negative pleural pressure and prevent water from being sucked into the pleural space.
- The hydrostatic pressure is proportional to the height of the fluid column.
- A disadvantage of this single bottle system is that, as liquid content (blood, pus, effusion fluid) is expelled from the pleural space and collects in the underwater-seal bottle, the seal tube becomes immersed deeper under water and the pressure required to force more contents into the bottle increases thus impeding the clearance of the pleural collection.
OTHER INFORMATION
Safety features
- First tube connecting drain to drainage bottles must be wide to decreased resistance.
- Volume capacity of this tube should exceed ½ of patient’s maximum inspiratory volume (otherwise H2O may enter chest).
- Volume of H2O in bottle B should exceed ½ patient’s maximum inspiratory volume to prevent in drawing of air during inspiration.
- Drain should always stay at least 45cm below patient (prevention of removed fluid or H2O refluxing into patient).
- Clamp drain when moving.
- H2O level above tube in the manometer bottle determines the amount of suction applied before air drain through tube (safety suction limiting device).
- If suction is turned off then tubing must be unplugged so that air can escape into atmosphere (otherwise a tension pneumothorax).
- Should not be applied following pneumonectomy.
Requirements of Under Water Seal Drainage
STERILE TROLLEY
Top Shelf
- A trochar and cannular intercostals tubing and an introducer.
- Artery forceps in a receiver.
- Scalpel.
- Suturing material.
- Safety pin.
- A large Winchester bottle containing water or normal saline to a level of about 6cm.
- A rubber cork pierced by a short and long glass tub or by rigid plastic tubes.
Bottom Shelf
- A pair of gloves
- Chest X-ray investigations and ultra sound scan results
- A dressing pack
- A patient’s file
Bedside
- Hand washing equipment
- Suction machine
- Screen
- Patient’s file
- Emergency tray
PROCEDURE FOR UNDERWATER SEAL DRAINAGE (UWSD)
Preparation of equipment
- Preferably a graduated bottle is used for correct reading of the drainage fluid.
- Assist doctor to sub merge the long tube in the water at 2 – 3cm but must not touch the bottom of the bottle. The short tube acts as an escape route for air in the vacuum space in the bottle.
- Assist the doctor to connect tube to the top of the underwater to the patient’s inter-costal drainage tube. To drain fluid from the pleural cavity.
PROCEDURE
- Explain the procedure carefully to the patient, to understand the importance of limited movements during the period of UWSD hence encouraging patient’s cooperation & relieves anxiety.
- Take the trolley to the bedside, screen the bed and close near by windows to provide privacy.
- Wash and dry hands and be ready to assist the doctor to promote hygiene measures.
- Position the patient leaning over the bed table supported by pillows. The patient’s arm which is on the side where the tube will be inserted must be placed forward and supported by a nurse. This position gives best access to the second or third intercostals space.
- Observe the patient’s colour, pulse and respiration throughout the procedure to detect any change in patient’s condition and manage accordingly.
- The doctor, cleans the patient’s skin, places a drape in position and injects local anesthesia. A scalpel is used to make an incision through the skin and muscle of the intercostals space using the introducer, the tubing is inserted and secures it with a stitch. Local anesthesia helps to retrieve pain.
- The nurse connects the tube to underwater seal drainage bottle once the introducer is removes, then clamp the tube with two pairs of clamps until all the connection s of the apparatus are sealed. This is done to clip the tube so as to prevent air going to the lungs.
- Remove the clamps and the functioning of the apparatus by nothing if the fluid in the tube rises and falls in rhythm with the patient’s respirations so as to ensure that the system is air tight and no air leakages and no risk of emphysema.
- Apply a dressing to the wound that makes an air tight seal at the incision site and prevents infection.
- Wash hands, clear away the equipment and leave the patient comfortable to prevent spread of infections.
CHANGING THE BOTTLE
- Securely clamp off the drain with two clamps but for a short time to minimize re-infection of the patient.
- Disconnect the tubing and put used apparatus to one side so as to minimize the re-infection of patient.
- Connect new tubing & bottle and remove the clamps.
- Monitor the fluid in tubing whether it is moving up and down in rhythm with the patient’s respiration rate so as to ensure that the tube is in situ and functioning.
- Record the amount of drainage on the fluid balance chart and note any abnormalities. It is effective assessment of progress of therapy and the patient.
- Wash hands, clear away and clean the used apparatus and equipment to prevent the spread of infections.
POINTS TO REMEMBER
- Make sure that all connections are secure to avoid leakages.
- Check that the patient is not compressing or kicking any part of the drainage system, to avoid obstructing the tube.
- The bottle must always remain below the level of the patient’s chest and should preferably be in as stand to avoid being easily knocked over, to prevent back flow of fluid from drainage chamber to pleural cavity and to maintain the water seal.
COMPLICATIONS.
- Kinking
- Occlusion
- Retrograde flow of fluid may occur if the collection chamber is raised above the level of the patient
- Clamping may cause a tension pneumothorax
- Glass bottles can break.

The lecture was so movalous