PARKINSON’S DISEASE
Parkinson’s disease is a neurodegenerative disorder characterized by the progressive loss of dopamine-producing cells in a specific region of the brain called the substantia nigra.
This loss of dopamine leads to abnormal brain activity and the manifestation of various motor and non-motor symptoms.
Cause of Parkinson’s Disease
The exact cause of Parkinson’s disease remains unclear, but it is believed to involve a combination of genetic and environmental factors. The exact cause of Parkinson’s Disease (PD) is unknown.
A combination of genetics and environmental factors is believed to trigger PD.
Factors that contribute to PD include:
- Dopamine deficiency: Parkinson’s disease is characterized by the loss of dopamine-producing neurons in the brain. Dopamine is a neurotransmitter that plays a crucial role in movement control, so a deficiency leads to motor symptoms like tremors and rigidity.
- Loss of norepinephrine: Norepinephrine is another neurotransmitter affected in Parkinson’s disease. It regulates various functions, including blood pressure, heart rate, and mood. Its loss can contribute to non-motor symptoms such as fatigue and changes in blood pressure.
- The protein alpha-synuclein: This protein can form abnormal clumps called Lewy bodies in the brains of people with Parkinson’s disease. These clumps are thought to damage nerve cells and contribute to the development of the disease.
- Genetics: While most cases of Parkinson’s disease are not directly inherited, certain genetic mutations can increase a person’s risk of developing the condition.
- Environmental factors: Exposure to certain environmental toxins, such as pesticides and heavy metals, has been linked to an increased risk of Parkinson’s disease.
- Mitochondria: Dysfunction of mitochondria (the energy-producing structures within cells) may play a role in Parkinson’s disease by leading to oxidative stress and cell damage in the brain.

Pathophysiology of Parkinson’s disease:
Parkinson’s disease is a progressive neurological disorder that affects movement. The disease is believed to be caused by the death of dopamine-producing cells in the substantia nigra, a part of the brain that helps control movement.
This leads to a depletion of dopamine, a neurotransmitter that helps regulate movement. The loss of dopamine causes problems with nerve signaling in the brain, which leads to the characteristic symptoms of Parkinson’s disease, such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability. These symptoms arise due to the imbalance of excitatory and inhibitory neurotransmitters in the corpus striatum.
In details;
- Initiating Factors: Antipsychotic drugs, encephalitis, and other causes can initiate the process.
- Substantia Nigra Affected: These factors affect the substantia nigra (SN), a brain region critical for motor control.
- Destruction of Dopaminergic Neurons: Leads to the destruction of dopaminergic neuronal cells within the substantia nigra, located in the basal ganglia.
- Depletion of Dopamine: This destruction causes a depletion of dopamine stores, a key neurotransmitter involved in movement.
- Degeneration of Nigrostriatal Pathway: The dopaminergic nigrostriatal pathway, which connects the substantia nigra to the corpus striatum, degenerates.
- Neurotransmitter Imbalance: An imbalance occurs between excitatory (acetylcholine, Ach) and inhibitory neurotransmitters in the corpus striatum, disrupting normal signaling.
- Motor Control Impairment: Results in difficulty controlling and initiating voluntary movements.
- Parkinson’s Disease Manifestation: Ultimately leads to the manifestation of Parkinson’s disease, characterized by:
- Tremors
- Rigidity
- Bradykinesia (slowness of movement)
- Postural changes
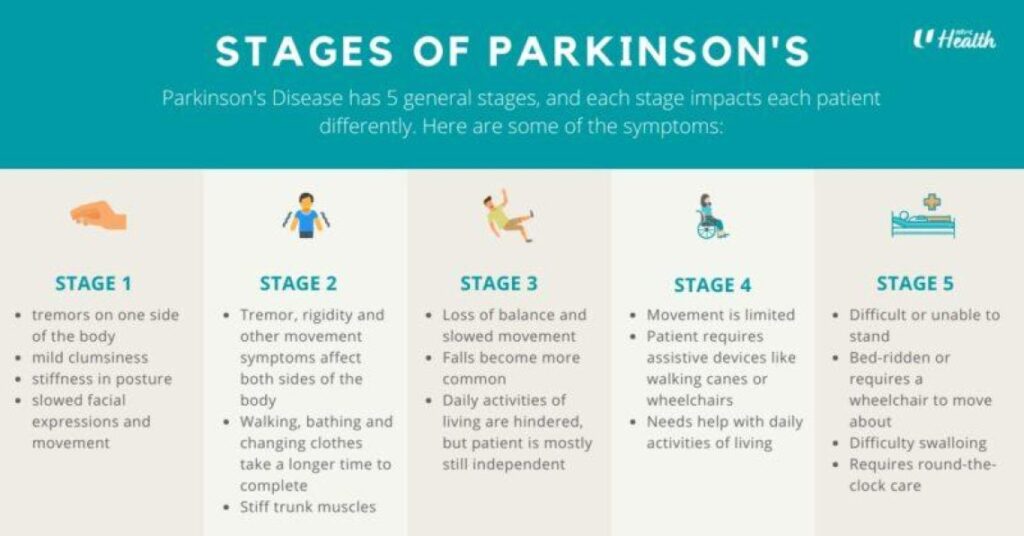
The 5 Stages of Parkinson's Disease
In the beginning, symptoms are very mild and only affect one side of the body. You might notice a patient has a slight tremor (shaking) in one hand or leg, or some stiffness. One side of their face may also show less expression. At this stage, the person can usually continue with their daily activities without much trouble.
The stiffness and tremors now spread to affect both sides of the body. The person's posture may start to change, and they may walk more slowly. Their face might look more "mask-like" with less blinking, and their speech can become softer or slower. Balance is not yet a major problem, but everyday tasks will take longer to complete.
This is the middle stage where loss of balance becomes the main problem. The person's movements are much slower, and falls become more common. They can still be independent in many ways (like dressing and eating), but activities are now more difficult. They might need some help to stay safe.
At this stage, the symptoms are severe. The person needs help to stand up and walk, and may use a walker or other assistive device. They are no longer able to live alone safely and will need a lot of help with daily care. While they may still be able to stand or walk for short periods, it is very difficult.
This is the most advanced stage. Severe stiffness in the legs may make it impossible to stand or walk, so the person may be in a wheelchair or bed-bound. They require 24-hour nursing care for all their needs. Some patients may also experience confusion, hallucinations (seeing things that are not there), or dementia.

Clinical Features of Parkinson’s Disease
1. Motor Symptoms:
- Tremors: Tremor present at rest but not during sleep characterized by rhythmic movements of 4 – 5 cycles a second and can occur in the head, facial muscles, limbs, jaw and lips. Micrographic (tiny handwriting) pill rolling character due to movement of the thumb across the palm also occurs. Tremors are increased by emotions.
- Rigidity: Muscles are stiff with pain in severe cases; rigidity may be continuous or intermittent. Fine limb movements are difficult to perform. Stiffness or resistance in muscles, making movements less fluid and causing muscle pain or discomfort.
- Akinesia: Loss or impairment in power of voluntary movement. Bradykinesia (slowness in walking) and hypokinesia (loss of movement): rising from a chair
becomes difficult and takes several attempts of falling back. - Imbalance: Change in gait, tendency to walk forward on toes with small steps may be accelerated. Fascination (work with short steep with no arm swinging) propels patient either forward or backward propulsively until falling is inevitable
- Postural Instability: Changes in balance ie stooped over posture when up right, difficult in entertaining balance when sited erect and semi flexed arms. Impaired balance and coordination, resulting in a tendency to stoop, shuffle while walking, and increased risk of falls.
- Bradykinesia: This means slowness of movement and speed (or progressive hesitations/halts) as movements are continued. It is one of the cardinal symptoms of Parkinson’s disease (PD). You must have bradykinesia plus at least either tremor or rigidity for a Parkinson’s diagnosis to be considered.
2. Non-Motor Symptoms:
- Cognitive Changes: Some individuals with Parkinson’s disease may experience mild cognitive impairment, memory problems, difficulty with executive functions, and in later stages, dementia.
- Sleep Disorders: Including insomnia, restless leg syndrome, excessive daytime sleepiness, and rapid eye movement sleep behavior disorder (acting out dreams during sleep).
- Autonomic Dysfunction: Symptoms may include orthostatic hypotension (low blood pressure upon standing), constipation, urinary problems, excessive sweating, and sexual dysfunction.
- Mood and Behavioral Changes: Depression, anxiety, apathy, and changes in mood or behavior are common in Parkinson’s disease.
- Sensory Symptoms: Loss of sense of smell (anosmia) and visual disturbances such as blurred or double vision.
- Speech and Swallowing Difficulties: Speaking softly, slurred speech, difficulty swallowing (dysphagia), and drooling may occur.
- Pain and Fatigue: Some individuals with Parkinson’s disease may experience pain, muscle cramps, and fatigue.
Diagnosis of Parkinson’s Disease
1. Medical History: The doctor will begin by taking a detailed medical history, including asking about the patient’s symptoms, their duration, and any family history of Parkinson’s disease.
2. Physical Examination: A thorough physical examination will be conducted to assess motor symptoms such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability. The doctor will also look for other possible causes of these symptoms.
3. Assessment of Symptoms: The doctor may use standardized rating scales, such as the Unified Parkinson’s Disease Rating Scale (UPDRS), to evaluate the severity of symptoms and track disease progression.
4. Response to Medication: Parkinson’s disease symptoms often respond positively to dopaminergic medications. The doctor may prescribe a trial of medication, such as levodopa, to observe if there is a significant improvement in symptoms. This can help support the diagnosis of Parkinson’s disease.
5. Neurological Examination: A neurological examination may be performed to evaluate other neurological signs and rule out alternative diagnoses.
6. Imaging Studies: While imaging studies are not mandatory for diagnosis, they can help exclude other conditions that mimic Parkinson’s disease. Imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can be used to assess the brain structure and rule out other causes.
7. Laboratory Tests: There are no specific blood tests to diagnose Parkinson’s disease. However, blood tests may be performed to rule out other medical conditions that can present with similar symptoms.
Management of Parkinson’s Disease
Unfortunately, as of 2025, Parkinson’s disease can’t be cured, but medicines can help control the symptoms. Medicines often work very well. When medicine is no longer helping, Surgery may be considered.
Aims of Management
- The primary goal in the management of PD is to treat the symptomatic motor and nonmotor features of the disorder, with the objective of improving the patient’s overall quality of life.
- To relieve symptoms and maintain functioning to improve quality of life.
Medical Management
1. Levodopa (L-Dopa) – Class: Dopamine Precursor
- Dosage: 50 – 125 mg three times daily immediately after meals.
- Side Effects: Nausea, vomiting, orthostatic hypotension (low blood pressure upon standing), dyskinesias (involuntary movements), hallucinations, confusion, and sleep disturbances. – Contraindications: Use with caution in patients with a history of psychosis, glaucoma, or melanoma. Avoid concurrent use with non-selective monoamine oxidase inhibitors (MAOIs).
2. Carbidopa-Levodopa – Class: Dopamine Precursor with Decarboxylase Inhibitor
- Dosage: The dosage is based on the ratio of carbidopa to levodopa, such as 25/100 8 hourly or 25/250 8 hourly.
- Side Effects: Similar to levodopa alone, but carbidopa helps reduce the peripheral side effects of levodopa, such as nausea and vomiting.
3. Dopamine Agonists – Class: Dopamine Receptor Agonists
- Examples: Pramipexole, Ropinirole, Rotigotine
- Dosage: The dosage varies depending on the specific medication and individual needs. It is initiated at a low dose and gradually increased.
- Side Effects: Nausea, dizziness, orthostatic hypotension, hallucinations, impulse control disorders (such as gambling or hypersexuality), and sleep disturbances.
4. MAO-B Inhibitors – Class: Monoamine Oxidase-B Inhibitors
- Examples: Selegiline, Rasagiline
- Dosage: The dosage varies depending on the specific medication. It is usually taken once or twice daily.
- Side Effects: Nausea, headache, insomnia, and potential interactions with certain foods and other medications.
- Contraindications: Use with caution in patients with a history of psychosis, cardiovascular disease, or peptic ulcer disease. Avoid concurrent use with non-selective MAOIs.
Specific Nursing Interventions for a patient with Parkinson’s disease:
1. Promote Safety:
– Assess the patient’s environment for potential hazards and remove obstacles to prevent falls.
– Encourage the use of assistive devices such as canes or walkers to improve stability and reduce the risk of falls.
– Provide education to the patient and their caregivers about fall prevention strategies and home safety modifications.
2. Assist with Mobility:
– Encourage regular physical exercise and activities tailored to the patient’s abilities to improve mobility, balance, and coordination.
– Collaborate with physical and occupational therapists to develop a personalized exercise and rehabilitation plan.
– Use appropriate techniques to assist the patient with transfers, ambulation, and maintaining proper body alignment.
3. Facilitate Communication:
– Encourage the patient to speak slowly and clearly, taking breaks between phrases to improve speech clarity.
– Use visual cues, gestures, or written communication aids to supplement verbal communication.
– Refer the patient to a speech therapist for evaluation and management of speech difficulties.
4. Support Swallowing:
– Provide the patient with a modified diet, including texture modifications or swallowing strategies as recommended by a speech therapist.
– Offer small, frequent meals to minimize fatigue and aid digestion.
– Encourage the patient to maintain an upright position while eating and drinking to facilitate swallowing.
5. Optimize Medication Management:
– Collaborate with the healthcare team to ensure timely administration of prescribed medications for symptom management.
– Monitor the patient’s response to medications and report any side effects or changes in symptoms.
– Educate the patient and caregivers about the importance of medication adherence and the proper administration of medications.
6. Manage Constipation:
– Encourage the patient to maintain a high-fiber diet and an adequate fluid intake.
– Recommend regular exercise and physical activity to promote bowel regularity.
– Discuss with the healthcare team the use of stool softeners or laxatives if necessary.
7. Provide Emotional Support:
– Offer empathetic and compassionate care to address the emotional and psychological impact of the disease.
– Encourage the patient to express their feelings and concerns, providing a supportive and non-judgmental environment.
– Refer the patient and their caregivers to support groups or counseling services to connect with others facing similar challenges.
8. Monitor Mental Health:
– Assess the patient for signs of depression, anxiety, or cognitive impairment.
– Collaborate with the healthcare team to manage and treat mental health symptoms.
– Encourage engagement in activities that promote mental stimulation, such as puzzles, reading, or social interactions.
9. Promote Sleep Hygiene:
– Educate the patient about good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime.
10. Educate the Patient and Caregivers:
– Provide education on Parkinson’s disease, its symptoms, and expected progression.
– Teach self-management strategies, including medication management, exercise, and symptom recognition.
– Inform the patient and caregivers about available community resources and support services.
Possible Nursing Diagnosis
1. Impaired Physical Mobility related to bradykinesia and rigidity as evidenced by inability to initiate movement, staying in the same position for long and needing support to carry out voluntary movement.
– Explanation: The characteristic motor symptoms of Parkinson’s disease, such as bradykinesia, rigidity, and postural instability, can significantly impair the patient’s ability to move, walk, and perform daily activities independently. Observation of the patient’s gait abnormalities, reduced range of motion, and difficulty with motor tasks can provide evidence for this diagnosis.
2. Risk for Falls related to tremors and orthostatic hypotension:
– Explanation: Parkinson’s disease can increase the risk of falls due to postural instability, gait disturbances, and reduced coordination. The patient may exhibit shuffling gait, decreased arm swing, and a stooped posture. History of falls, presence of orthostatic hypotension, and environmental hazards in the patient’s living area can further support this diagnosis.
3. Impaired Swallowing related to muscle weakness involved in swallowing as evidenced by difficulty in swallowing, choking during eating, coughing and food sticking in the throat(verbalisation/facial grimace) :
– Explanation: Parkinson’s disease can lead to dysphagia (difficulty swallowing) due to muscle weakness, impaired coordination, and decreased mobility of the muscles involved in swallowing. The patient may exhibit prolonged meal times, coughing or choking during meals, or complaints of food sticking in the throat. Evaluation by a speech therapist and observations during meals can provide evidence for this diagnosis.
4. Risk for Impaired Verbal Communication related to speech muscle involvement:
– Explanation: Parkinson’s disease can affect the muscles involved in speech production, leading to reduced volume, slurred speech, and monotone voice. The patient may demonstrate difficulty in articulating words and expressing thoughts. Assessment by a speech therapist and observation of the patient’s speech patterns can support this diagnosis.
5. Risk for Impaired Skin Integrity related to immobility, incontinence:
– Explanation: The combination of bradykinesia, rigidity, and postural instability in Parkinson’s disease can lead to decreased mobility and changes in body alignment. These factors, along with sensory disturbances, can increase the risk of pressure ulcers and skin breakdown. Observation of the patient’s skin condition, areas of pressure, and assessment of skin integrity can provide evidence for this diagnosis.
Surgical Management of Parkinson’s disease.
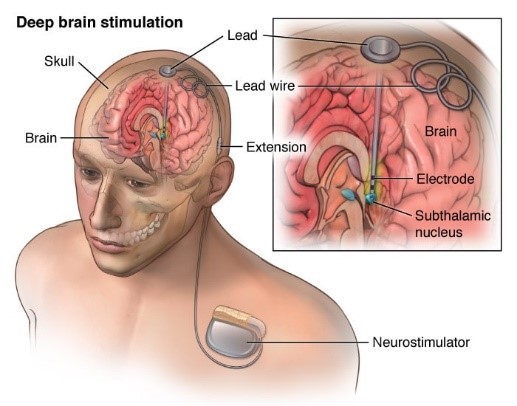
Deep Brain Stimulation (D.B.S):
- Is a surgical procedure in which electrodes are placed in specific areas of the brain, electrodes are connected to a generator which is programed to send electrical pulses to the brain.
- The procedure may help to alleviate the following symptoms; tremor, rigidity, stiffness & slowed movement
Facial Nerve Decompression Surgery
- Management of acute facial paralysis may involve facial nerve decompression surgery in cases of virally-induced facial paralysis (Bell’s palsy, Ramsay-Hunt syndrome) or primary facial nerve repair/grafting in cases of resection or transection of the facial nerve

Nursing care
- Perform motion exercises to all joints 3 time a day, massage skeletal muscles to relieve stiffness and use a broad base support when ambulating.
- Advise patient care givers to avoid pyridoxine protein food and alcohol when using levodopa
- Modify home environment to remove hazards and alert the patient on effects of stress, heat and excitement
- Avoid staying in one position for a long time and try walking with hand clasped behind.
- Motor patient weight weekly, follow plans for small frequent meals and avoid eating high protein meals at medication time. Ensure adequate fiber and fluid intake.
- Perform exercise voice regulation by singing or reading loud.
- Monitor sleep pattern, thought disorders and hallucination.
- Respond promptly to the urge of urination, defecation and ensure emptiness. Use stool softeners if needed, keep urinal at bedside and monitor bowel habits.
- Avoid carpets and rugs on floor as a patient sticks on them, use walking aids and offer shoes that are easy to put with smooth soles on to the patient.
- Alternative medicine i.e massage, tai chi , yoga, pet therapy ,meditation
- Joining support groups
Diagnosis of Parkinson’s Disease
1. Medical History: The doctor will begin by taking a detailed medical history, including asking about the patient’s symptoms, their duration, and any family history of Parkinson’s disease.
2. Physical Examination: A thorough physical examination will be conducted to assess motor symptoms such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability. The doctor will also look for other possible causes of these symptoms.
3. Assessment of Symptoms: The doctor may use standardized rating scales, such as the Unified Parkinson’s Disease Rating Scale (UPDRS), to evaluate the severity of symptoms and track disease progression.
4. Response to Medication: Parkinson’s disease symptoms often respond positively to dopaminergic medications. The doctor may prescribe a trial of medication, such as levodopa, to observe if there is a significant improvement in symptoms. This can help support the diagnosis of Parkinson’s disease.
5. Neurological Examination: A neurological examination may be performed to evaluate other neurological signs and rule out alternative diagnoses.
6. Imaging Studies: While imaging studies are not mandatory for diagnosis, they can help exclude other conditions that mimic Parkinson’s disease. Imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can be used to assess the brain structure and rule out other causes.
7. Laboratory Tests: There are no specific blood tests to diagnose Parkinson’s disease. However, blood tests may be performed to rule out other medical conditions that can present with similar symptoms.

Complications of Parkinson’s Disease
1. Falls and Fall-related Injuries:
– Due to impaired balance, postural instability, and motor symptoms, individuals with Parkinson’s disease are at an increased risk of falls. Falls can result in injuries such as fractures, head trauma, and soft tissue damage.
2. Dysphagia and Aspiration Pneumonia:
– Parkinson’s disease can lead to difficulty swallowing (dysphagia), which increases the risk of food or liquid entering the airway (aspiration). Aspiration pneumonia, a lung infection caused by inhaling foreign material, is a potential complication of dysphagia.
3. Psychiatric and Mood Disorders:
– Depression, anxiety, and apathy are common psychiatric conditions that can occur in Parkinson’s disease. These mood disorders can significantly impact the patient’s quality of life and may require treatment and psychological support.
4. Cognitive Impairment and Dementia:
– As Parkinson’s disease progresses, some individuals may develop cognitive impairment, including problems with memory, attention, and executive functions. In some cases, this can progress to Parkinson’s disease dementia, which affects thinking, judgment, and daily functioning.
5. Sleep Disorders:
– Parkinson’s disease is associated with various sleep disturbances, such as insomnia, restless leg syndrome, and rapid eye movement (REM) sleep behavior disorder. These sleep disorders can lead to excessive daytime sleepiness, fatigue, and overall reduced quality of sleep.
6. Medication-related Complications:
– Long-term use of medications for Parkinson’s disease, such as levodopa, can lead to complications known as motor fluctuations and dyskinesias. Motor fluctuations are changes in the response to medication, resulting in periods of good symptom control (on periods) and periods of poor symptom control (off periods). Dyskinesias are involuntary, abnormal movements that can occur during certain periods.
Nursing Care Plan: Parkinson’s Disease
Assessment | Nursing Diagnosis | Goals/Expected Outcomes | Interventions | Rationale | Evaluation |
Patient presents with resting tremors, bradykinesia, rigidity, and postural instability. Difficulty initiating voluntary movements. | Impaired Physical Mobility related to muscle rigidity and bradykinesia as evidenced by difficulty walking, shuffling gait, and tremors. | – Patient will demonstrate improved mobility and engage in physical activities with minimal assistance. – Patient will perform range-of-motion (ROM) exercises daily. – Patient will maintain safety while ambulating. | 1. Encourage regular physical activity, including passive and active ROM exercises. 2. Provide assistive devices (walker, cane) as needed. 3. Teach the patient to use the “rocking” technique to initiate movement. 4. Educate on maintaining an upright posture and taking large, deliberate steps. 5. Collaborate with a physical therapist for mobility training. | 1. Helps prevent stiffness and maintain joint flexibility. 2. Promotes independence and reduces fall risk.
3. Overcomes movement initiation difficulties.
4. Improves gait and reduces the risk of falls. 5. Enhances mobility and functional ability. | – Patient engages in physical activity with minimal assistance. – Patient reports improved mobility. – Patient remains free from falls and injuries. |
Patient reports difficulty holding utensils, dressing, and writing. Increased time required for daily tasks. (Dressing, Eating, Grooming) | Decreased Self-Care Deficit syndrome related to bradykinesia and tremors as evidenced by inability to button clothes, feed self, or use utensils effectively. | – Patient will demonstrate improved ability to perform self-care activities with minimal assistance. – Patient will use adaptive devices to enhance independence. – Patient will maintain personal hygiene and grooming. | 1. Encourage the use of adaptive utensils and clothing with Velcro fasteners. 2. Allow extra time for the patient to complete tasks. 3. Provide cues and step-by-step instructions for self-care activities. 4. Encourage family involvement in assisting the patient as needed. 5. Refer to an occupational therapist for fine motor skill training. | 1. Facilitates independence despite motor difficulties.
2. Reduces frustration and promotes dignity.
3. Supports cognitive function and task completion. 4. Ensures patient receives necessary support while promoting autonomy. 5. Helps improve the patient’s ability to perform daily activities. | – Patient demonstrates improved ability to dress, eat, and groom. – Patient uses adaptive devices effectively. – Patient experiences less frustration with self-care. |
Patient exhibits soft, monotone speech, masked facial expression, and difficulty swallowing. | Impaired Verbal Communication related to muscular rigidity and bradykinesia as evidenced by slow speech, decreased voice volume, and difficulty articulating words. | – Patient will use alternative communication methods as needed. – Patient will engage in speech therapy exercises. – Patient will demonstrate improved ability to express needs. | 1. Encourage the patient to speak slowly and exaggerate pronunciation. 2. Suggest deep breathing exercises to strengthen vocal cords. 3. Use communication aids such as writing boards or voice amplifiers. 4. Encourage speech therapy to improve articulation and voice control. 5. Provide a calm, quiet environment to enhance communication. | 1. Helps improve clarity of speech. 2. Strengthens respiratory muscles and voice projection.
3. Compensates for verbal communication difficulties. 4. Enhances the ability to communicate effectively. 5. Reduces frustration and improves comprehension. | – Patient reports improved ability to communicate. – Patient uses communication aids effectively. – Patient participates in speech therapy sessions. |
Patient has difficulty swallowing, risk of aspiration, and reports choking episodes. | Inadequate nutritional intake related to impaired swallowing (dysphagia) as evidenced by coughing, drooling, and difficulty swallowing food and liquids. | – Patient will swallow safely without signs of aspiration. – Patient will maintain adequate nutritional and hydration status. – Patient will use modified diet strategies to prevent aspiration. | 1. Assess swallowing ability and risk for aspiration. 2. Position patient upright (90-degree angle) during meals and for at least 30 minutes after eating. 3. Encourage small, frequent meals with thickened liquids if needed. 4. Teach patient to use the “chin tuck” technique while swallowing. 5. Refer to a speech therapist for swallowing evaluation and therapy. | 1. Identifies patients at high risk for aspiration.
2. Promotes safe swallowing and reduces aspiration risk.
3. Prevents choking and maintains adequate nutrition.
4. Helps direct food away from the airway.
5. Enhances swallowing ability and safety. | – Patient swallows safely without choking or aspiration. – Patient maintains adequate nutritional intake. – Patient follows recommended swallowing techniques. |
Patient expresses sadness, frustration, and social withdrawal due to disease progression. | Chronic confusion related to chronic illness and functional decline as evidenced by social isolation, low mood, and frustration with self-care difficulties. | – Patient will verbalize feelings and express emotions appropriately. – Patient will participate in social activities as tolerated. – Patient will demonstrate coping strategies to manage frustration. | 1. Encourage the patient to express emotions and frustrations. 2. Provide emotional support and active listening. 3. Encourage participation in support groups or therapy. 4. Promote enjoyable activities that the patient can engage in despite limitations. 5. Monitor for signs of severe depression or suicidal thoughts and refer to a mental health professional if needed. | 1. Helps the patient process emotions and reduce distress.
2. Provides reassurance and support.
3. Promotes socialization and reduces isolation.
4. Encourages engagement in life despite limitations.
5. Ensures early intervention for severe depression. | – Patient reports improved mood and emotional well-being. – Patient engages in social activities. – Patient verbalizes coping strategies effectively. |
Nursing Concerns in Parkinson’s Disease:
Risk of Falls:
Concern for the patient’s increased risk of falls due to impaired balance and coordination.
Implementation of fall prevention strategies and regular assessments of gait and stability.
Functional Independence:
Concern for the preservation of the patient’s functional independence.
Promotion of activities that enhance independence in daily living.
Psychosocial Well-being:
Concern for the patient’s mental health and emotional well-being.
Regular assessment of mood, addressing any signs of depression or anxiety.
Communication Difficulties:
Concern for potential communication challenges.
Monitoring the patient’s ability to express needs and facilitating communication support as required.
Nutritional Status:
Concern for maintaining adequate nutrition.
Regular assessments of the patient’s nutritional intake and collaboration with dietitians to address any deficits.


Some samples quixon parkinson’s disease please
Very good note indeed
Welcome
Am only left with answer,question approach😋😋😋
Good work
Very detailed notes and well explained indeed can use it to teach and also to manage patients with Parkinson’s disease
Any common questions about this condition would help us pass well