Table of Contents
ToggleNURSING PROCESS
The Nursing process is an organized, systematic, dynamic method of giving individualized nursing care that focuses on identifying and treating unique responses of individuals or groups, to actual or potential alterations in health. (Nursing procedure Manual, 2015)
OR:
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient–focused care.
Outline the CHARACTERISTICS of the nursing process
- Cyclic and Dynamic: – it is an ongoing continuous process throughout the stages of illness and treatment and ends with the cease of the illness.
- Goal directed and Client oriented: The nursing process is intended to treat the patient and is in the best interest of the patient.
- Interpersonal and Collaborative: This goes to explain the amount of interaction that might be necessary between nurses, patients of similar illnesses and the medical team.
- Universally applicable: This process is universally standard and no matter what the institution it may be, the process remains the same.
- Scientific and Systematic: Every symptom or sign is a result of a scientific fact which leads to scientific methods of treatment and follow-ups. It is systematic and goes from step to step as in the phases mentioned below.
- Requires critical thinking: The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
Explain the components of the nursing process
1. Assessment
2. Diagnosis
3. Planning
4. Implementation
5. Evaluation
ASSESSMENT PHASE
The first phase of the nursing process is assessment.
It involves collecting, organizing, validating, and documenting the clients’ health status. Assessment involves data collection which is the process of gathering information regarding a client’s health status. The main methods used to collect data are health interviews and physical examination.
Types of data collected
- Subjective data or symptoms: This is information obtained from the patient through an interview. It also includes symptoms felt by the patient only. It is only the patient who can tell you information e.g. present complaints, past medical history, past surgical history etc
- Objective data or signs: This is the information that is measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing e.g. vomiting, distended abdomen, presence of edema, lung sounds, crying, skin color, and presence of diaphoresis.
NURSING DIAGNOSIS PHASE.
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an
individual, family, group, or community.
NB: Medical diagnosis is different from a nursing diagnosis because nursing diagnosis refers to human response to health conditions whereas the medical diagnosis focuses on health conditions.
Types of the nursing diagnosis:
1. Actual nursing diagnosis
- These are presenting response to current health condition
- The actual nursing diagnosis has three parts i.e. Diagnosis, relation to (pathophysiology) and evidence.
Scenario A: A patient complaining of fevers, on thermometer reading it indicates 38°C.
From NANDA 2024 – 2026 fevers have hyperthermia i.e.
Hyperthermia related to increased leukocyte activity evidenced by the thermometer reading of 38°C.
Scenario B: A patient complained of headache of the forehead since the last 2 days after a minor head injury following a fight. On examination the pain was at 3 on a 0 – 5 pain scale.
From NANDA 2024 – 2026 headache is described as Acute pain since it has been present less than 3 months.
-Acute pain related to trauma to the head evidenced by the patient’s verbalization of feeling headache of 3 on a 0 – 5 pain scale.
2. Potential Nursing diagnosis:
- This is an issue that could occur incase the current symptoms is not properly managed.
- The potential nursing diagnosis has two parts that is the nursing diagnosis and the relation (pathophysiology) only.
Scenario: A patient reported vomiting for 1 day after ingesting chips and chicken. On examination the patient had no signs of dehydration.
From NANDA 2024 – 2026 vomiting does not have an actual nursing diagnosis it only has a potential nursing diagnosis which is risk for inadequate fluid volume.
–Risk for inadequate fluid volume related to vomiting.
PLANNING PHASE
The planning stage is where goals and outcomes are formulated that directly impact patient care.
Planning phase is divided into
1. Goals
2. Expected outcomes
Goals
- These are the aims of the nursing interventions to be provided.
- Therefore they should be smart
Goals should be:
- Specific or on point
- Measurable or Meaningful
- Attainable or Action-Oriented
- Realistic: it should represent things in a way that is accurate and true to life
- Timely or Time-Oriented
Goals are divided into 3 categories i.e.
1. Short term goals: these are goals having time limit ranging from minutes to 5 days.
2. Intermediate goals: these are goals having time limit ranging from 5 days to 30 days.
3. Long term goals: these are goals having time limit ranging from 30 days to years.
Expected Outcome
- This what a nurse expects the patient to present after provision of the nursing interventions
Its divided into 2 i.e. short term and long term outcomes.
IMPLEMENTATION PHASE
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect.
It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care.
The implementation phase is divided into two parts
- Nursing Interventions
- Rationale
EVALUATION
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. This is the past tense of the outcome if they have been
achieved.
Explain the importance of using a nursing process
- The nursing process allows the nurse to provide effective care by prioritizing meaningful interventions based on their assessments and clinical diagnosis of the patient.
- At the end of the nursing process, the nurse evaluates the success of their care to ensure that effective care is being prioritized.
- It creates a standard of care where the nurse develops a nursing diagnosis and care plan based on their assessment of the patient.
- The nursing process provides care that is centered around the individual patient which reduces the time the client spends in the health care facility, and optimizes their health by minimizing complications in care.
- By setting defined goals with a clear timeline in the nursing process, the nurse can evaluate the effectiveness of the care they are providing and make changes to the care plan as needed.
SO IN BRIEF
Assessment:
- Subjective Data (Symptoms): Patient complaining of fevers.
- Objective Data (Signs): Thermometer reading indicates 38°C.
Diagnosis:
- Actual Nursing Diagnosis: Hyperthermia related to increased leukocyte activity evidenced by the thermometer reading of 38°C.
- Potential Nursing Diagnosis: Risk for fluid volume deficit related to vomiting.
Planning (Goals/Expected Outcomes):
Goals:
- Short Term: Reduce temperature to between 36.0°C to 37.4°C within 30 minutes.
- Intermediate Term: [Specify a goal if needed]
- Long Term: [Specify a goal if needed]
Expected Outcomes:
The patient will verbalize that he no longer feels feverish. Thermometer reading will be between 36.0°C to 37.4°C.
Implementation:
- [Specify nursing interventions here, e.g., tepid sponging.]
Rationale:
- [Explain why you did the intervention, e.g., To allow evaporative cooling.]
Evaluation:
- Patient verbalized that he no longer feels feverish, and the thermometer reading was 36.7 degrees Celsius after 30 minutes
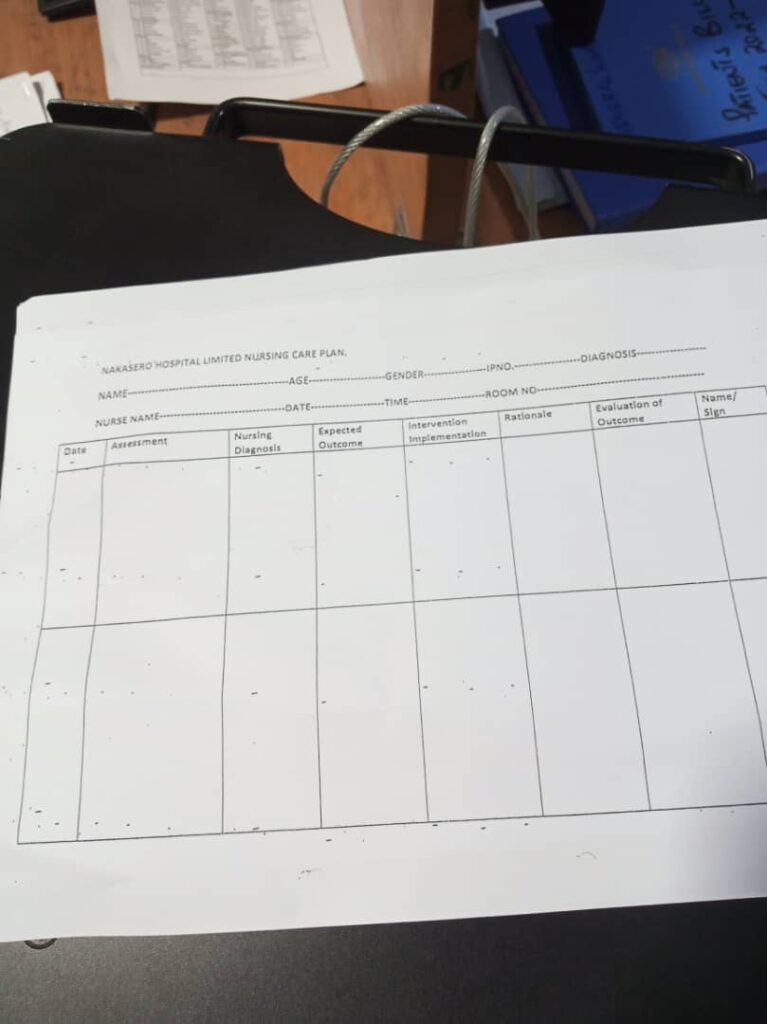
Sample Care Plan
Sample Nursing Care Plan for a patient with Malaria
Assessment | Diagnosis | Planning (Goals or Expected Outcomes) | Implementation/ Interventions | Rationale | Evaluation |
Fever | Hyperthermia related to leucocyte activity as evidenced by an elevated temperature of 39° C. | Reduce fever to 37° C within 30 minutes. | – Administer antipyretic medication as prescribed. – Encourage adequate fluid intake. – Apply cooling measures (e.g., tepid sponging). | – Antipyretic medication helps lower the fever. Adequate fluid intake prevents dehydration. Cooling measures aid in reducing body temperature. | Fever reduced to 37° C |
Headache | Acute Pain related to malarial infection evidenced by patient verbalizing headache. | Alleviate headache within 40 minutes. | – Administer analgesic medication as prescribed. – Provide a quiet and dimly lit environment. – Encourage relaxation techniques (e.g., deep breathing). | – Analgesic medication helps relieve pain. – A quiet environment reduces stimuli that may exacerbate the headache. – Relaxation techniques promote comfort. | Headache Alleviated with In 40 minutes With a pain Scale reading Of 1/10. |
Myalgias | Impaired Physical Mobility related to muscle pain and weakness as evidenced by difficulty in movement. | Improve mobility and reduce muscle pain within 5 days. | – Encourage gentle stretching exercises. Administer analgesic medication as prescribed. – Provide warm compresses to affected areas. | – Gentle stretching improves flexibility and reduces muscle pain – Analgesic medication helps relieve pain. – Warm compresses promote muscle relaxation. | Improved mobility and reduced muscle pain After 5 days. |
Nausea | Nausea related to changes in eating habits as evidenced by patient complaints and increased salivation | Alleviate nausea within 1 hour. | – Administer antiemetic medication as prescribed. – Encourage small, frequent meals. – Provide oral hygiene measures after vomiting episodes. | – Antiemetic medication helps alleviate nausea. – Small, frequent meals are easier to tolerate. – Oral hygiene measures prevent discomfort and promote a sense of well-being. | Patient vebalised That no nausea After 1 hour.. |
Vomiting | Risk for inadequate fluid volume related to unpleasant sensory stimuli | The client will report decreased severity or elimination of nausea and vomiting. | – Administer antiemetic medication as prescribed. – Monitor and record intake and output. – Provide oral rehydration solutions as needed. | – Antiemetic medication helps control vomiting. – Monitoring intake and output prevents dehydration. – Oral rehydration solutions restore fluid balance. | The client reported elimination of nausea and vomiting. |
Diarrhea | Risk for inadequate Nutritional intake related to less food intake as evidenced by watery stool. | Achieve optimal nutritional intake. | – Administer antidiarrheal medication as prescribed. – Encourage a bland and easily digestible diet. – Monitor and record bowel movements. | – Antidiarrheal medication helps control diarrhea. – A bland diet is easier on the digestive system. – Monitoring bowel movements informs about the effectiveness of interventions. | Achieved optimal nutritional intake |
Dehydration | Risk for impaired fluid volume balance related to diarrhea, nausea and vomiting. | Patient will maintain hydration as evidenced by adequate intake and output, vital signs, and skin turgor | Administer fluids intravenously as indicated. Offer high-water content foods like soups Administer antiemetics as indicated. | Fluids for fluid replacement To encourage rehydration and motility of the bowel. To reduce vomiting episoded | Patient maintained hydration. |
Summary NANDA
Expected outcomes:
- Patients will demonstrate bowel sounds within normal limits.
- Patients will exhibit normal eating habits without experiencing nausea, vomiting, abdominal discomfort, dyspepsia, bloating, and early satiety.
- Patient will exhibit balanced nutrition as evidenced by the absence of malnutrition
- Patient will regain and maintain adequate body weight for age and gender
- Patient will verbalize two strategies to reduce nausea and improve comfort.
- Patient will express improved comfort as evidenced by improved sleep and mood.
- Patient will verbalize relief from nausea
- Patient will be able to demonstrate strategies that prevent nausea
- Patient will maintain hydration as evidenced by adequate intake and output, vital signs, and skin turgor


Wowww, this is good, is there any way one can download it as a book
But I think finding it here at anytime is better that opening book or pdfs, and we constantly update the notes, yet books cant be updated without getting a new copy.
Very nice guys
I have really liked this topic of. Nu
Thanks so much
Understanding nursing process had been an unsolved issues, until I found here a very simplified and revised notes.
Thank you so much 👍😊
I guess your enjoying my HALLO ‘s
I used to misunderstand the difference between Nursing and medical diagnosis.
But thank you so much.
Now I am good and confident to have my patient-care go on another Level.
Stay blessed, for the fact that I’ve become well versed with the broad topic today ie nursing Dx
Thanks so much for simplifying my work
Thanks so much for the wonderful explanation on nursing process at least I gained more knowledge
God bless the author. I have enjoyed reading it and am going to get better results end .Thks
How can i download this book
Wowww, u guys are blessed already…
Its a great Job to us
Wow thank you people
This is wonderful
I have love it…..I like this idea
I really appreciate it and I’m so happy to be part this group
This group is fantastic and so educative, I really love it.
Wow this is wonderful, i have really enjoyed reading the topic.
This is really good, i have enjoyed reading the topic
Very awesome I humbly appreciate it thanks alot, May God bless you for this kindness.
I have enjoyed and understood this nursing process very well thanks to the authors
I would like to join the WhatsApp group please
Some help
Me to l want to join it
I really appreciate you people
How can I download this piece
Like the content
Wow !!!! brilliant thanks a lot be blessed
Thank you so much the content is easier to understand.
Wow, I have just found my best tutor here😊😊,after months of struggling to understand nursing process, I have finally got it very clearly today, thanks so much for this simplicity
Great work, well done. Very good reference material to enhance self study
It has been my greatest weakness but now I believe am a good teacher of the NP, thanks alot for u’ve made a difference in me
It’s just good work ✌️
This is very good and helpful, thanks to those who developed it.
For sure you have made it for me thanks
More explanation on Nursing care plan
Thanks for educating
Great work 👍
This is fantastic
It’s well summarized and have loved it but nursing care plan and specific nursing action should also be highlighted please
This is a good job well understood may God almighty bless you
This is a job well done may God almighty bless you
I really appreciate ur great work, I was confused on how to state the diagnosis
This is good
Thank you so much for keeping us updated with the relevant information but please make it possible for us to download it for review. Thank you
GBU
I used to hate this topic but now I understand something
It’s a good 👍 detailed Nursing process