Parkinson’s Disease is a slowly progressive degenerative neurologic disorder affecting the brain centers that are responsible for control and regulation of movement where there is loss of brain cells that produce dopamine that leads to insufficient production of dopamine.
Parkinsonism disease is called shaking disease or shaking palsy or paralysis agitans. It’s a degenerative disease of the nervous system related to cerebral atherosclerosis. This extrapyramidal disorder was named after James Parkinson in 1817 who describe it as a movement disorder.
Table of Contents
TogglePredisposing factors
The cause of the disease is mostly unknown (idiopathic) but research suggests several causative factors;
(i) Postencephalitic Parkinsonism (encephalitis lethergica): feature may develop 20 years later and may include oculogyric crisis
ii) Drug may induce Parkinsonism such as haloperidol, metoclopramide, phenothiazine and lithium
iii) Hypoxia due excess carbon monoxide
iv) Toxic substances like manganese
v) Vascular abnormalities like atherosclerosis
- Genetics,
- Atherosclerosis,
- Viral infections e.g. viral encephalitis,
- Head trauma,
- Exposure to industrial pollutant,
- chemical toxin such as manganese,
- Herbicides,
- Chemical solvents or poly chlorinated biphenyls.,
- Antipsychotic drug
- Age
- Sex
Pathophysiology of Parkinsonism
Parkinson’s disease is associated with the degeneration of dopamine producing neurons in the substantia nigra of neurum an area in basal ganglia (deep in cerebral hemisphere). Dopamine is a neurotransmitter responsible for controlling and refining motor movement as an inhibitor co-paired to acetylcholine which is muscle exciters like coordination and posture.
When excitory activity of acetylcholine is not balanced by dopamine difficulty in controlling and initiating voluntary movements occur and acetylcholine effects are exaggerated. Cellular degeneration in Parkinson’s disease leads to impairment in the extrapyramidal tracts that control semiautomatic and coordinated movements. The exact cause is unknown though it can be caused by drugs, genetical and environmental factors.
Clinical Manifestations of Parkinson’s Disease
Cardinal Signs and Symptoms of Parkinson’s Disease
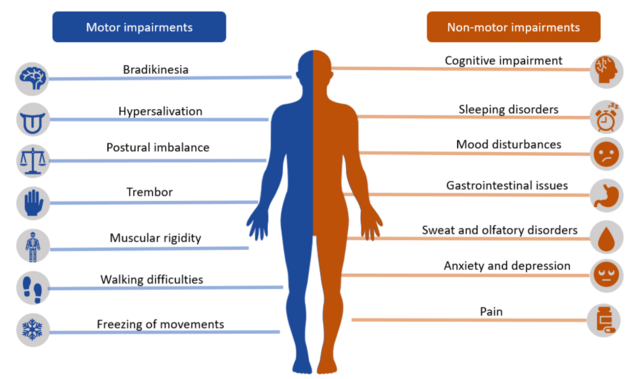
- Tremors: Tremor present at rest but not during sleep characterized by rhythmic movements of 4 – 5 cycles a second and can occur in the head, facial muscles, limbs, jaw and lips. Micrographic (tiny hand writing) pill rolling character due to movement of the thumb across the palm also occur. Tremors are increased by emotions.
- Rigidity: Rigidity: muscles are stiff with pain in severe cases; rigidity may be continuous or intermittent. Fine limb movements are difficult to perform.
- Akinesia: Loss or impairment in power of voluntary movement. Bradykinesia (slowness in walking) and hypokinesia (loss of movement): rising from a chair
becomes difficult and takes several attempts of falling back. - Posture and Balance: Change in gait: tendency to walk forward on toes with small steps may be accelerated. Fascination (work with short steep with no arm swinging) propels patient either forward or back ward propulsively until falling is inevitable
Changes in balance ie stooped over posture when up right, difficult in entertaining balance
when sited erect and semi flexed arms.
Other signs and symptoms include;
- The patient walks backwards if pulled from the back (pull test)
- Speech is soft monotonous and slurred with difficulty in starting speech.
- Slowness in thought and disinterest
- Autonomic symptoms like constipation, dysuria, postural hypotension
- Sensory function and tendon reflexes are normal
Differential Diagnosis
- Essential tremor
- Dementia with Lewy bodies
- Multiple system atrophy
- Alzheimer’s disease
- Drug induced parkinsonism
- CBD cortical basal degeneration and PSP progressive supranuclear palsy
Management of Parkinson’s Disease
Medical Management
There is no cure treatment for Parkinsonism disease; the victims can be helped with drugs that improve akinesia, rigidity and tremors.
- Dopaminergic Agents e.g. Levodopa – it’s a chemical that is converted to dopamine in the brain.
- Dopamine antagonistic e.g. bromopride. Butaclamol can mimic natural dopamine in the brain.
- Dopamine agonists reduce bradykinesia tremor and rigidity such as bromocriptine merylate, levodopa, carbidopa, pramipexole etc
- MAO-B inhibitor e.g. phenelzine and tranylcypromine, help reduce breakdown of dopamine in the brain. These drugs led to nausea, hypotension. Palpitation, dry mouth and sleep disturbance
- Anti-cholinergics; e.g. chlorpromazine (Thorazine) to help reduce tremor, acetylcholine in CNS e.g. cycrimine, procyclidine, benztropine, biperiden and Benzhexol (aten) also relieves tremors
As a nurse avoid drug with similar effects like antihistamine, antispasmodics and tricyclic antidepressants. Monitor side effects such as delirium, blurred vision, constipation, agitation, hallucination anxiety and confusion - Amantadine help to improve muscle control and relief stiffness
Surgical Management of Parkinson’s disease.
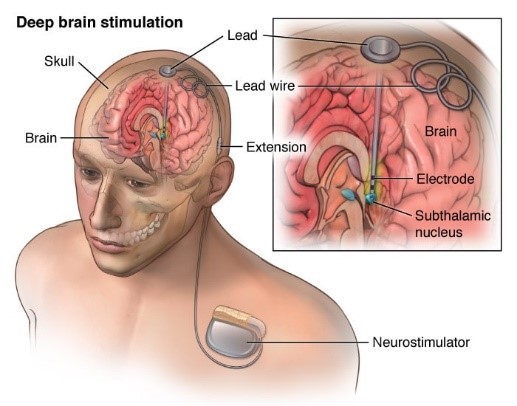
Deep Brain Stimulation (D.B.S):
- Is a surgical procedure in which electrodes are placed in specific areas of the brain, electrodes are connected to a generator which is programed to send electrical pulses to the brain.
- The procedure may help to alleviate the following symptoms; tremor, rigidity, stiffness & slowed movement
Facial Nerve Decompression Surgery
- Management of acute facial paralysis may involve facial nerve decompression surgery in cases of virally-induced facial paralysis (Bell’s palsy, Ramsay-Hunt syndrome) or primary facial nerve repair/grafting in cases of resection or transection of the facial nerve

Nursing Care
- Perform motion exercises to all joints 3 time a day, massage skeletal muscles to relieve stiffness and use a broad base support when ambulating.
- Advise patient care givers to avoid pyridoxine protein food and alcohol when using levodopa
- Modify home environment to remove hazards and alert the patient on effects of stress, heat and excitement
- Avoid staying in one position for a long time and try walking with hand clasped behind.
- Motor patient weight weekly, follow plans for small frequent meals and avoid eating high protein meals at medication time. Ensure adequate fiber and fluid intake.
- Perform exercise voice regulation by singing or reading loud.
- Monitor sleep pattern, thought disorders and hallucination.
- Respond promptly to the urge of urination, defecation and ensure emptiness. Use stool softeners if needed, keep urinal at bedside and monitor bowel habits.
- Avoid carpets and rugs on floor as a patient sticks on them, use walking aids and offer shoes that are easy to put with smooth soles on to the patient.
- Alternative medicine ie massage, tai chi , yoga, pet therapy ,meditation
- Joining support groups
Diagnosis
- PET Scan (positron emission tomography)—decreased dopaminergic activity in the substantia nigra
- Unified Parkinson’s Disease Rating Scale—cognitive interview
- Normal CT
- Normal MRI
Complications
- Dysphagia (difficulty in chewing and swallowing)
- Depression
- Anxiety
- Dementia
- Constipation
- Smell dysfunctions , sexual dysfunction ,orthostatic hypotension , bladder problems , constipation, sleep disorders


Some samples quixon parkinson’s disease please
Very good note indeed
Welcome