Table of Contents
ToggleAnxiolytic and Hypnotic Agents
Anxiolytic agents are drugs used to depress the central nervous system (CNS) to prevents the signs and symptoms of anxiety.
Hypnotic agents are drugs used to depress the CNS to causes sleep.
Common Terms
- Anxiety: unpleasant feeling of tension, fear, or nervousness in response to an environmental stimulus, whether real or
imaginary. - Barbiturate: former mainstay drug used for the treatment of anxiety and for sedation and sleep induction; associated
with potentially severe adverse effects and many drug–drug interactions, which makes it less desirable than some of the newer agents. - Benzodiazepine: drug that acts in the limbic system and the
reticular activating system to make gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter, more effective, causing interference with neuron firing; depresses CNS to
block the signs and symptoms of anxiety, and may cause
sedation and hypnosis in higher doses. - Hypnosis: extreme sedation resulting in CNS depression and sleep
- Sedation: loss of awareness of and reaction to environmental
stimuli. - Sedative: drug that depresses the CNS; produces a loss of
awareness of and reaction to the environment .
Drugs used as Anxiolytic and Hypnotic Agents
| BENZODIAZEPINES USED AS ANXIOLYTICS | BARBITURATES USED AS ANXIOLYTIC-HYPNOTICS | OTHER ANXIOLYTIC AND HYPNOTIC DRUGS |
|---|---|---|
| alprazolam (Xanax) | phenobarbital | promethazine (Phenergan) |
| diazepam (Valium) | butabarbital | zolpidem |
| clonazepam | amobarbital | buspirone |
| oxazepam | pentobarbital | meprobamate |
BENZODIAZEPINES USED AS ANXIOLYTICS
Benzodiazepines, the most frequently used anxiolytic drugs, prevent anxiety without causing much associated sedation. In addition, they are less likely to cause physical dependence than many of the older sedatives/hypnotics that are used to relieve anxiety.
Dose

Indications of Benzodiazepines used as Anxiolytics
The benzodiazepines are indicated for the treatment of the following conditions:
- anxiety disorders like, generalized anxiety disorder, social anxiety disorder, panic disorder
- alcohol withdrawal
- hyperexcitability and agitation
- Obsessive-compulsive disorder (OCD)
- preoperative relief of anxiety and tension to aid in balanced anesthesia.
Pharmacodynamics
- These drugs act in the limbic system and the RAS to make gamma aminobutyric acid (GABA) more effective, causing interference with neuron firing.
- GABA stabilizes the postsynaptic cell. This leads to an anxiolytic effect at doses lower than those required to induce sedation and hypnosis.
Note. The exact mechanism of action is not clearly understood.
Mechanism of Action
- Anxiolytics enhance the effect of gamma amino butyric acid (GABA) and depress the CNS, which in turn depresses the limbic system that integrates other systems governing emotions. GABA causes relaxation of skeletal muscles, anticonvulsive effects, and calming of emotional response.
- These drugs cause central nervous system (CNS) depression through potentiation of GABA, a neurotransmitter that decreases neuronal excitability in the brain.
Pharmacokinetics
- The benzodiazepines are well absorbed from the gastrointestinal (GI) tract, with peak levels achieved in 30 minutes to 2 hours.
- They are lipid soluble and well distributed throughout the body, crossing the placenta and entering breast milk.
- The benzodiazepines are metabolized extensively in the liver. Patients with liver disease must receive a smaller dose and be monitored closely.
- Excretion is primarily through the urine.
Contraindications and Cautions
- Allergy to any benzodiazepine.
- Psychosis, which could be exacerbated by sedation.
- Acute narrow-angle glaucoma, shock, coma, or acute alcoholic intoxication, all of which could be exacerbated by the depressant effects of these drugs.
- Pregnancy: Contraindicated in pregnancy because a predictable syndrome of cleft lip or palate, inguinal hernia, cardiac defects, microcephaly, or pyloric stenosis occurs when they are taken in the first trimester. Neonatal withdrawal syndrome may also result.
- Lactation: Breast-feeding is also a contraindication because of potential adverse effects on the neonate (e.g., sedation).
- Use with caution in elderly or debilitated patients because of the possibility of unpredictable reactions and in cases of renal or hepatic dysfunction, which may alter the metabolism
and excretion of these drugs, resulting in direct toxicity. Dose adjustments usually are needed for such patients
Adverse Effects and Side Effects
The adverse effects of benzodiazepines are associated with the impact of these drugs on the central and peripheral nervous systems.
Nervous system effects include;
- sedation
- drowsiness
- depression
- lethargy
- blurred vision
- headaches
- apathy
- light-headedness
- confusion
- GI conditions such as dry mouth, constipation, nausea, vomiting, and elevated liver enzymes may result.
- Cardiovascular problems may include hypotension, hypertension, arrhythmias, palpitations, and respiratory difficulties.
- Hematological conditions such as blood dyscrasias and anemia are possible.
- Genitourinary (GU) effects include urinary retention and
hesitancy, loss of libido, and changes in sexual functioning.
Note: Abrupt cessation of these drugs may lead to a withdrawal syndrome characterized by nausea, headache, vertigo, malaise, and nightmares.
Drug Interactions
- The risk of CNS depression increases if benzodiazepines are taken with alcohol or other CNS depressants, so such combinations should be avoided.
- Effects of benzodiazepines increase if they are taken with cimetidine, oral contraceptives, or disulfiram.
- Impact of benzodiazepines may be decreased if they are given with theophyllines or ranitidine.
Remember; Flumazenil is the antidote of benzodiazepine.
Special Nursing Considerations when using Benzodiazepines as Anxiolytics.
- Do not administer intra-arterially because serious arteriospasm and gangrene could occur. Monitor injection sites carefully for local reactions to institute treatment as soon as possible.
- Do not mix intravenous (IV) drugs in solution with any other drugs to avoid potential drug–drug interactions.
- Give parenteral forms only if oral forms are not feasible or available, and switch to oral forms, which are safer and less
likely to cause adverse effects, as soon as possible. - Give IV drugs slowly because these agents have been associated with hypotension, bradycardia, and cardiac arrest.
- Arrange to reduce the dose of narcotic analgesics in patients receiving a benzodiazepine to decrease potentiated effects and sedation.
- Maintain patients who receive parenteral benzodiazepines in bed for a period of at least 3 hours. Do not permit ambulatory patients to operate a motor vehicle after an injection to ensure patient safety.
- Monitor hepatic and renal function, as well as CBC, during long-term therapy to detect dysfunction and to arrange to taper and discontinue the drug if dysfunction occurs.
- Taper dose gradually after long-term therapy, especially in epileptic patients. Acute withdrawal could precipitate seizures
in these patients. It may also cause withdrawal syndrome. - Provide comfort measures to help patients tolerate drug effects, such as having them void before dosing, instituting a
bowel program as needed, giving food with the drug if GI upset is severe, providing environmental control (lighting, temperature, stimulation), taking safety precautions (use of side rails, assistance with ambulation), and aiding orientation. - Provide thorough patient teaching, including drug name, prescribed dose, measures for avoidance of adverse effects, and warning signs that may indicate possible problems. Instruct patients about the need for periodic monitoring and
evaluation to enhance patient knowledge about drug therapy
and to promote compliance. - Offer support and encouragement to help the patient cope with the diagnosis and the drug regimen.
- If necessary, use flumazenil , the benzodiazepine
antidote, for the treatment of overdose.

BARBITURATES USED AS ANXIOLYTIC-HYPNOTICS
The barbiturates were once the sedative/hypnotic drugs of choice.
Not only is the likelihood of sedation and other adverse effects greater with these drugs than with newer sedative/hypnotic drugs, but the risk of addiction and dependence is also greater. For these reasons, newer anxiolytic drugs have replaced the barbiturates in most instances.
Dose
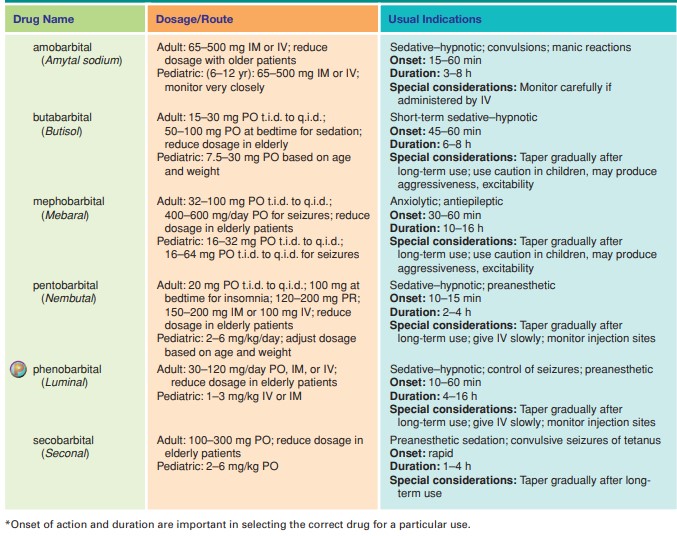
Indications
- For the relief of the signs and symptoms of anxiety
- For sedation, pre anesthesia,
- Sleep disorders like insomnia
- Treatment of seizures
Pharmacodynamics
- The barbiturates are general CNS depressants that inhibit
neuronal impulse conduction in the ascending RAS, depress
the cerebral cortex, alter cerebellar function, and depress motor output - Thus, they can cause sedation, hypnosis, anesthesia, and, in extreme cases, coma.
Pharmacokinetics
- The barbiturates are absorbed well, reaching peak levels in 20
to 60 minutes. - They are metabolized in the liver.
- Excreted in the urine.
- The longer-acting barbiturates tend to be metabolized slower
and excreted to a greater degree unchanged in the urine.
Contraindications
- Allergy to any barbiturate
- Addiction. Previous history of addiction to sedative/hypnotic drugs because the barbiturates are more addicting than most other anxiolytics.
- Porphyria, which may be exacerbated
- Hepatic impairment or nephritis, which may alter the metabolism and excretion of these drugs
- Respiratory distress or severe respiratory dysfunction, which could be exacerbated by the CNS depression caused by these drugs.
- Pregnancy is a contraindication because of potential adverse
effects on the fetus; congenital abnormalities have been
reported with barbiturate use.
Adverse Effects
The adverse effects caused by barbiturates are more severe than those associated with other, newer hypnotics. For this reason, barbiturates are no longer considered the mainstay for the treatment of anxiety.
- CNS effects may include drowsiness, somnolence, lethargy, ataxia, vertigo, a feeling of a “hangover,” thinking abnormalities, paradoxical excitement, anxiety, and hallucinations.
- GI signs and symptoms such as nausea, vomiting, constipation, diarrhea, and epigastric pain may occur.
- CVS effects may include bradycardia, hypotension (particularly with IV administration), and syncope.
- Respiratory, Serious hypoventilation may occur, and respiratory
depression and laryngospasm may also result, particularly
with IV administration. - Hypersensitivity reactions, including rash, serum sickness, and Stevens–Johnson syndrome, which is sometimes fatal, may also occur.
Drug Interactions
- Increased CNS depression results if these agents are taken with other CNS depressants, including alcohol, antihistamines, and other tranquilizers. If other CNS depressants are used, dose adjustments are necessary.
- There often is an altered response to phenytoin if it is combined with barbiturates.
- If barbiturates are combined with monoamine oxidase (MAO) inhibitors, increased serum levels and effects occur.
- The following drugs may not be as effective as desired if taken with barbiturates: oral anticoagulants, digoxin, tricyclic antidepressants (TCAs), corticosteroids, oral contraceptives, estrogens, acetaminophen, metronidazole, phenmetrazine, carbamazepine, beta-blockers, griseofulvin, phenylbutazones,
theophyllines, quinidine, and doxycycline, because of an enzyme induction effect of barbiturates in the liver.
Special Nursing Considerations when using Barbiturates used as Anxiolytic-Hypnotic.
- Do not administer these drugs intra-arterially because serious arteriospasm and gangrene could occur. Monitor injection sites carefully for local reactions.
- Do not mix IV drugs in solution with any other drugs to avoid potential drug–drug interactions.
- Give parenteral forms only if oral forms are not feasible or available, and switch to oral forms as soon as possible to avoid serious reactions or adverse effects.
- Give IV medications slowly because rapid administration may
cause cardiac problems. - Provide standby life-support facilities in case of severe respiratory depression or hypersensitivity reactions.
- Taper dose gradually after long-term therapy, especially in patients with epilepsy. Acute withdrawal may precipitate seizures or cause withdrawal syndrome in these patients.
- Provide comfort measures to help patients tolerate drug effects, including small, frequent meals; access to bathroom facilities; bowel program as needed; consuming food with the drug if
GI upset is severe; and environmental control, safety precautions, orientation, and appropriate skin care as needed. - Provide thorough patient teaching, including drug name, prescribed dosage, measures for avoidance of adverse effects, and warning signs that may indicate possible problems.
- Instruct patients about the need for periodic monitoring and
evaluation to enhance patient knowledge about drug therapy
and to promote compliance. - Offer support and encouragement to help the patient cope with the diagnosis and the drug regimen.
OTHER ANXIOLYTIC AND HYPNOTIC DRUGS
Other drugs are used to treat anxiety or to produce hypnosis
that do not fall into either the benzodiazepine or the barbiturate group.
• Antihistamines (promethazine [Phenergan], diphenhydramine [Benadryl]) can be very sedating in some people.
They are used as preoperative medications and postoperatively to decrease the need for narcotics.
• Buspirone (BuSpar), a newer antianxiety agent, has no sedative, anticonvulsant, or muscle relaxant properties, and its mechanism of action is unknown. However, it reduces the signs and symptoms of anxiety without many of the CNS effects and severe adverse effects associated with other anxiolytic drugs. It is rapidly absorbed from the GI tract, metabolized in the liver, and excreted in urine.
• Zaleplon (Sonata) and zolpidem (Ambien), both of which cause sedation, are used for the short-term treatment of insomnia. They are thought to work by affecting serotonin levels in the sleep center near the RAS(The reticular activating system ). These drugs are metabolized in the liver and excreted in the urine.
Other Indications and special consideration

Multiple Choice Questions.
1. Drugs that are used to alter a patient’s response to the environment are called
a. hypnotics.
b. sedatives.
c. antiepileptics.
d. anxiolytics.
The correct answer is d. anxiolytics. Anxiolytics are drugs that are used to reduce anxiety and alter a patient’s response to their environment. Hypnotics and sedatives are drugs that induce sleep or reduce agitation. Antiepileptics are drugs used to treat seizures.
2. The benzodiazepines are the most frequently used anxiolytic drugs because
a. they are anxiolytic at doses much lower than those needed for sedation or hypnosis.
b. they can also be stimulating.
c. they are more likely to cause physical dependence than older anxiolytic drugs.
d. they do not affect any neurotransmitters.
The correct answer is a. they are anxiolytic at doses much lower than those needed for sedation or hypnosis. Benzodiazepines are preferred as anxiolytic drugs because they are effective at much lower doses than those required for inducing sedation or hypnosis. They act by enhancing the effects of the neurotransmitter gamma-aminobutyric acid (GABA) in the brain, which results in a reduction of anxiety. While benzodiazepines can cause physical dependence with long-term use, they are not more likely to do so than older anxiolytic drugs. Some benzodiazepines can have stimulating effects, but this is not a reason why they are most frequently used as anxiolytic drugs.
3. Barbiturates cause liver enzyme induction, which could lead to
a. rapid metabolism and loss of effectiveness of other drugs metabolized by those enzymes.
b. increased bile production.
c. CNS depression.
d. the need to periodically lower the barbiturate dose to
avoid toxicity.
The correct answer is a. rapid metabolism and loss of effectiveness of other drugs metabolized by those enzymes. Barbiturates are known to cause liver enzyme induction, which can accelerate the metabolism of other drugs that are metabolized by those same enzymes. This can result in a loss of effectiveness of these other drugs and can even lead to drug interactions that can be harmful or life-threatening. Increased bile production (option b) is not a common effect of barbiturates, while CNS depression (option c) is a well-known effect of these drugs. The need to periodically lower the barbiturate dose to avoid toxicity (option d) is also a common concern when using these drugs, but it is not directly related to their liver enzyme-inducing properties.
4. A person who could benefit from an anxiolytic drug for short-term treatment of insomnia would not be prescribed
a. zolpidem.
b. chloral hydrate.
c. buspirone.
d. meprobamate.
The correct answer is c. buspirone. Buspirone is not typically used to treat insomnia, as it has a slower onset of action and is not as effective at inducing sleep as other drugs that are specifically indicated for insomnia. Zolpidem (option a) is a commonly used sleep aid that can also have anxiolytic effects. Chloral hydrate (option b) and meprobamate (option d) are older drugs that are sometimes used for short-term treatment of insomnia and anxiety, but they are not as commonly used as some of the newer drugs in these classes.
5. Anxiolytic drugs block the awareness of and reaction to the environment. This effect would not be beneficial
a. to relieve extreme fear.
b. to moderate anxiety related to unknown causes.
c. in treating a patient who must drive a vehicle for a living.
d. in treating a patient who is experiencing a stress
reaction.
The correct answer is c. in treating a patient who must drive a vehicle for a living. Anxiolytic drugs can produce a variety of effects on the patient’s awareness of and reaction to the environment, ranging from mild sedation to complete loss of consciousness. While these effects can be beneficial in some cases, such as in relieving extreme fear (option a) or moderating anxiety related to unknown causes (option b), they can be detrimental in situations where the patient’s ability to drive or operate machinery is critical. Therefore, treating a patient who must drive a vehicle for a living (option c) with an anxiolytic drug may not be appropriate. An anxiolytic drug may be beneficial in treating a patient who is experiencing a stress reaction (option d), but the decision to use such a drug would depend on the specific circumstances and the patient’s overall health status.
6. Mr. Jones is the chief executive officer of a large company and has been experiencing acute anxiety attacks. His physical examination was normal, and he was diagnosed with anxiety. Considering his occupation and his need to be alert and present to large groups on a regular basis, the following anxiolytic would be a drug of choice for Mr. Jones:
a. phenobarbital
b. diazepam
c. clorazepate
d. buspirone
The correct answer is d. buspirone. Given Mr. Jones’ occupation and need to be alert and present to large groups on a regular basis, an anxiolytic drug with minimal sedative effects would be the drug of choice. While all of the drugs listed can be used as anxiolytics, phenobarbital (option a) and diazepam (option b) are known to have sedative effects and can impair alertness and cognition, making them less than ideal choices for Mr. Jones. Clorazepate (option c) is less sedating than phenobarbital and diazepam, but it can still cause drowsiness and impair cognitive function. Buspirone (option d) is a non-benzodiazepine anxiolytic drug that does not have sedative effects and is well-suited for individuals who need to remain alert and attentive.
7. The benzodiazepines react with
a. GABA-receptor sites in the RAS to cause inhibition of neural arousal.
b. norepinephrine-receptor sites in the sympathetic nervous system.
c. acetylcholine-receptor sites in the parasympathetic nervous system.
d. monoamine oxidase to increase norepinephrine breakdown.
The correct answer is a. GABA-receptor sites in the RAS to cause inhibition of neural arousal. Benzodiazepines are a class of drugs that act as positive allosteric modulators of the GABA-A receptor, which is an inhibitory receptor in the central nervous system. When benzodiazepines bind to the GABA-A receptor, they enhance the effect of GABA and increase the inhibitory tone of the central nervous system, leading to sedative, anxiolytic, and anticonvulsant effects. The RAS (reticular activating system) is a group of nuclei in the brainstem that play a key role in regulating arousal and wakefulness, and the inhibition of neural arousal in this system is one of the mechanisms by which benzodiazepines produce their effects. Benzodiazepines do not react with norepinephrine-receptor sites in the sympathetic nervous system (option b), acetylcholine-receptor sites in the parasympathetic nervous system (option c), or monoamine oxidase (option d).
8. A pediatric patient is prescribed phenobarbital preoperatively to relieve anxiety and produce sedation. After giving the injection, you should assess the patient for
a. acute Stevens–Johnson syndrome.
b. bone marrow depression.
c. paradoxical excitement.
d. withdrawal syndrome.
The correct answer is c. paradoxical excitement. Phenobarbital is a barbiturate that can produce sedative effects by enhancing the activity of GABA, an inhibitory neurotransmitter in the central nervous system. However, in some patients, especially pediatric patients, barbiturates can produce paradoxical excitement instead of sedation, which is characterized by restlessness, agitation, and hyperactivity. Therefore, after giving phenobarbital to a pediatric patient preoperatively, it is important to assess the patient for paradoxical excitement, as this may require additional sedation or alternative anxiolytic medications to achieve the desired effect. Acute Stevens-Johnson syndrome (option a) and bone marrow depression (option b) are not expected adverse effects of phenobarbital at therapeutic doses, and withdrawal syndrome (option d) is a potential adverse effect of prolonged use of phenobarbital or other barbiturates, but it is not a concern in a single preoperative dose.


Wonderful notes