Table of Contents
ToggleAsphyxia neonatorum
Asphyxia neonatorum is one of the pediatric emergencies and is the leading cause of neonatal mortality and morbidity. It is also an important cause of developmental delay and neurological problems in both term and preterm infants. It is crucial for midwives and nurses to have the knowledge and skills to care for babies with this condition.
Definition of asphyxia neonatorum
This is a failure of the baby to initiate and sustain normal respiration at birth.
A normal baby has good muscle tone at birth and moves their arms and legs actively, while asphyxia neonatorum infants are completely limp and unable to move their limbs.
This condition is a neonatal emergency as it may lead to hypoxia (lowering of oxygen supply to the brain and tissues), and possible brain damage or death if not correctly managed.
Types of Asphyxia
Asphyxia livida (Blue asphyxia) or stage of cyanosis:
- Primarily due to respiratory failure with Apgar score 4-6.
- The most common cause is the blockage of the airway.
Asphyxia pallida or stage of shock:
- This is due to combined respiratory and vasomotor failure with Apgar score 0-3.
- Depending on the Apgar scoring system, a score of 0-3 indicates severe depression, 4-6 indicates moderate depression, and 7-10 indicates no depression.
Pathophysiology of asphyxia
Birth asphyxia is related to a reduction in arterial oxygen tension, accumulation of carbon dioxide, and a fall in pH. Acidosis occurs due to the anaerobic utilization of glucose, production of lactic acid, and accumulation of carbon dioxide.
These biochemical changes result in constriction of muscular pulmonary arterioles and raised pulmonary arterial pressure, leading to reduced filling of the left heart.
Hypoglycemia occurs due to glucose utilization and depletion of glycogen stores. Petechial hemorrhage occurs due to anorexic capillary changes. Cerebral edema develops due to the intracellular collection of sodium and inappropriate release of ADH.
In prolonged asphyxia, myocardial function and cardiac output deteriorate. Blood flow to all organs is reduced, and progressive organ damage results.
Initial deprivation of oxygen results in rapid breathing. If asphyxia continues, respiratory movements stop, and the heart rate begins to fall with the gradual diminution of neuromuscular tone. Then, the baby enters a period of apnea known as primary apnea. In this stage, stimulation and exposure to oxygen may induce respiration.
But if asphyxia continues, the neonate develops deep gasping respiration, blood pressure falls, the baby becomes flaccid, respiration becomes weaker, and weaker until the neonate takes a last gasp and enters a period of secondary apnea.
The baby becomes unresponsive to stimulation and will not spontaneously resume respiratory efforts unless resuscitation with assisted ventilation and oxygenation is initiated promptly.
Primary and secondary apnea are difficult to distinguish, and all apnea at birth should be considered as secondary apnea, requiring immediate resuscitation to prevent brain damage and multi-organ system dysfunction.
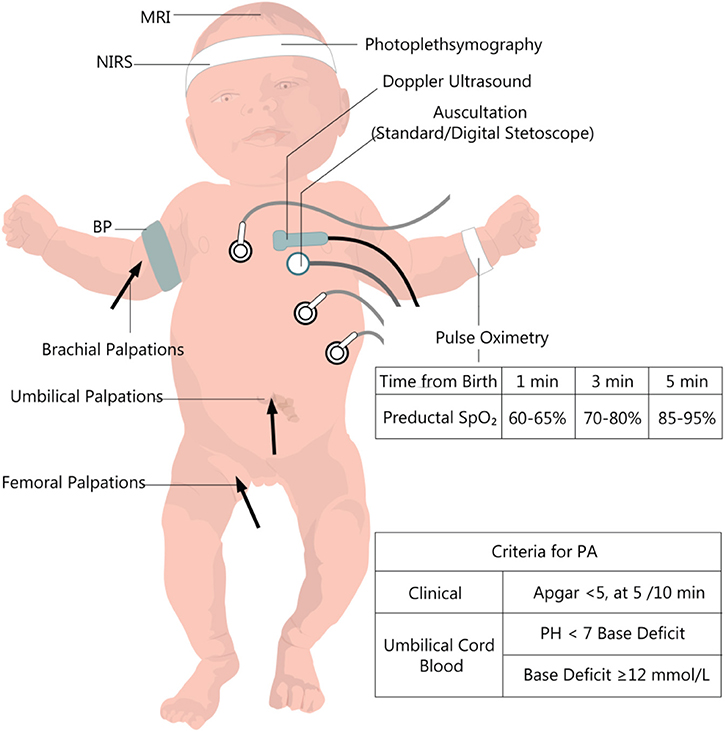
Signs & Symptoms
- The baby does not breathe but may make an attempt to breathe or gasp.
- The period of apnea is usually short (less than 30 seconds) but cries vigorously.
- The color is blue.
- Muscle tone is good.
- The cord is pulsating strongly and feels firm.
- The heartbeat is strong but rather slow.
- Apgar score is 4 – 6.
Aetiology
Approximately 90% of asphyxia events occur as a result of placental insufficiency due to ante partum and intra partum factors. Postnatal factors account for the remaining.
Ante partum factors include:
- Placental insufficiency due to conditions like pre-eclampsia, hypertension, anemia, diabetes mellitus, and post-maturity.
Other factors like;
- Antepartum hemorrhage,
- Malpresentation,
- Multiple pregnancies,
- Poor fetal growth,
- Rhesus immunization, bad obstetrical history, maternal systemic diseases (e.g., asthma, heart disease),
- Polyhydramnios or oligohydramnios,
- Maternal drug therapy (e.g., lithium) or maternal drug abuse,
- Vascular anomalies of the cord, and congenital anomalies of the fetus.
Intrapartum factors include:
- Fetal distress,
- Preterm labor,
- Antepartum hemorrhage (placenta previa, abruptio placentae),
- Cord prolapse, tight umbilical cord around the fetal neck,
- Prolonged labor exceeding 24 hours, prolonged second stage lasting more than 2 hours, maternal distress (dehydration, hypotension, and acidosis),
- The use of anesthesia and narcotics during labor,
- Birth trauma resulting in increased intracranial pressure due to hemorrhage, and difficult deliveries in malpresentation.
Postnatal factors include;
- They are mainly related to pulmonary, cardiovascular, and neurological abnormalities of the neonate,
- Including aspiration causing airway obstruction,
- Circulatory collapse due to blood loss and shock, preterm birth resulting in weak respiratory muscles,
- Poor pulmonary expansion, low alveolar surfactant, and an inefficient respiratory center.
Management
Maternity center:
- A baby of this type of Asphyxia responds to treatment promptly.
- As soon as the baby’s head is delivered, clear the airway and suck out the mucus from the nose with a mucus extractor.
- When a baby is completely delivered, put it over the mother’s abdomen and continue sucking out mucus.
- Clamp and cut the cord and separate the baby from the mother. Apgar score is assessed within one minute.
- In the absence of any respiratory effort, resuscitation measures are commenced.
- Put the baby on the resuscitation table, position the baby with the head slightly extended and the baby lying flat (NEUTRAL position), continue to clear the airway.
- Maintain warmth throughout the procedure.
- Give 0₂, 1 liter per minute (PRN).
In hospital management:
- The management is the same as that in a maternity center, except in the hospital, the doctor has to be informed, and oxygen must be administered.
- If necessary, place the baby in a cot with the head turned to one side.
- In summary:
- Put the baby in a neutral position.
- Clear the airway.
- Give oxygen.
Severe Asphyxia
This is one of the neonatal emergencies, and it’s a serious condition in a newborn. The baby is lacking oxygen and is deeply shocked at birth.
Signs of severe asphyxia:
- Slow, feeble heart rate.
- Baby not breathing, later shallow breathing with occasional gasps occurs.
- Poor muscle tone.
- Pale, grey.
- Cord pulsates feebly and slowly.
- Feels flabby if the cord pulsates below 100 and is weak. Immediate resuscitation is necessary.
- Apgar score less than 4.
Management of severe asphyxia
Management in a maternity center:
Aims:
- To establish and maintain respiration as soon as possible.
- To clear the airway.
- Provision of 0₂.
- Prevention of the condition from getting worse.
This is one of the neonatal emergencies, and no time should be wasted as it’s a matter of life and death. This condition should never be allowed to be treated in a maternity center unless the mother comes in the second stage.
In summary, we consider the following:
- Position: Baby’s shoulders may be elevated on a small towel, causing slight extension of the head and straightening the trachea.
- Ventilation: Clear the airway, insert a neonatal airway.
- External cardiac massage: Chest compression should be performed if the heart rate is less than 60-100 b/m and falling despite adequate ventilation. Chest is compressed at a rate of 100-120 times per minute at a ratio of 3 compressions to one ventilation
Resuscitation: The components of neonatal resuscitation procedure are described as the acronym TABCD’s of resuscitation..
Aims of resuscitation:
- Establish and maintain a clear airway by oxygenation.
- Ensure effective circulation.
- Correct acidosis.
- Prevent hypothermia.
- Hypoglycemia and hemorrhage.
T – Maintenance of temperature:
- Provision of a radiant heat source.
- Dry the baby.
- Remove wet linen.
A – Establishment of open airway:
- Position the infant.
- Suction the mouth, nose, and, in some instances, the trachea (in meconium-stained liquor).
- If necessary, insert an ET tube to ensure an open airway.
B – Initiation of breathing:
- Tactile stimulation to initiate respirations.
- Positive pressure ventilation (PPU) using either a bag and mask or a bag and ET tube.
C – Maintenance of circulation:
- Stimulate and maintain blood circulation by chest compressions.
D – Drugs:
- Dexamethasone (dose will depend on the general condition of the baby).
- 25% dextrose.
Prevention of asphyxia:
Prevention includes;
- Good antenatal care and early detection of predisposing factors,
- Screening mothers early and referring them to the hospital,
- Health education to mothers about nutrition and prevention of infections,
- Early treatment of infections that could lead to placental insufficiency (e.g., syphilis),
- Examination of blood to rule out conditions like rhesus incompatibility,
- Good intranatal care, prevention of prolonged labor, and proper observation during labor for maternal and fetal conditions.
Complications:
Complications of asphyxia neonatorum may include;
- Brain damage due to a lack of oxygen,
- Intracranial hemorrhage,
- Mental retardation,
- Hypothermia due to damage to the heat-regulating center, and
- Respiratory complications such as pneumonia.

The notes are well summerised and nice to read