Autism Spectrum Disorder (ASD)
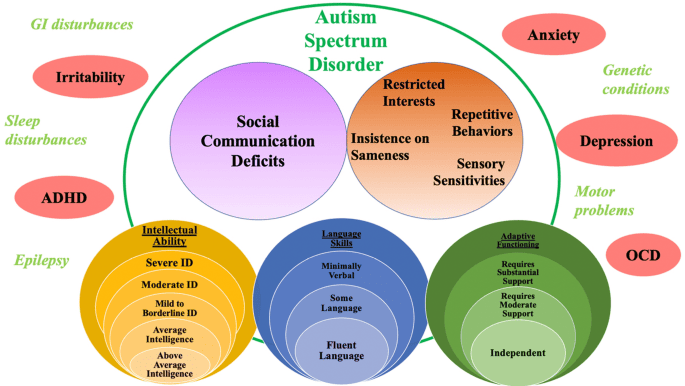
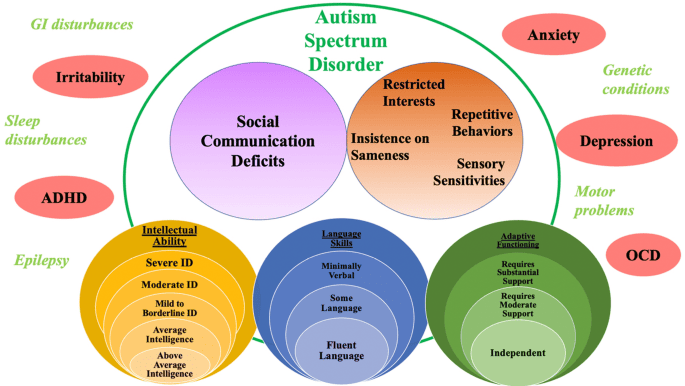
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental disorder characterized by persistent challenges in social interaction, verbal and nonverbal communication, and by restricted, repetitive patterns of behavior, interests, or activities.
The term "spectrum" reflects the wide variation in the type and severity of symptoms experienced by individuals with ASD.
Key Characteristics of the Definition:
- Neurodevelopmental Disorder: This classification indicates that ASD originates in early brain development. It affects how the brain functions, impacting areas such as social perception, communication, and processing sensory information.
- It is not a mental illness, although co-occurring mental health conditions are common.
- The signs and symptoms typically emerge in early childhood, often before the age of three, and can be lifelong.
- Persistent Challenges in Social Communication and Social Interaction: This deficit manifests in various ways, including:
- Difficulties with social-emotional reciprocity: Problems with back-and-forth conversation, reduced sharing of interests, emotions, or affect; failure to initiate or respond to social interactions.
- Deficits in nonverbal communicative behaviors used for social interaction: Atypical use of eye contact, body language, facial expressions, gestures; difficulty understanding and using nonverbal cues.
- Deficits in developing, maintaining, and understanding relationships: Challenges adjusting behavior to suit different social contexts, difficulties in sharing imaginative play or making friends, absence of interest in peers.
- Restricted, Repetitive Patterns of Behavior, Interests, or Activities: This characteristic also presents in diverse forms, such as:
- Stereotyped or repetitive motor movements, use of objects, or speech: (e.g., hand flapping, finger flicking, rocking; lining up toys or flipping objects; echolalia, idiosyncratic phrases).
- Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior: (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals).
- Highly restricted, fixated interests that are abnormal in intensity or focus: (e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interests).
- Hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment: (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
II. The "Spectrum" Concept:
The diagnostic criteria for ASD are presented on a spectrum because the presentation varies significantly among individuals. This variability encompasses:
- Severity of Symptoms: Some individuals have mild challenges that may require minimal support, while others have severe impairments necessitating substantial support.
- Developmental Profile: Intellectual ability can range from profound intellectual disability to giftedness.
- Language Skills: Communication abilities range from being nonverbal to having highly advanced vocabulary but still struggling with social pragmatics (the social rules of language).
- Co-occurring Conditions: The presence and impact of other medical or psychiatric conditions vary widely.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), published by the American Psychiatric Association, consolidated previous separate diagnoses (Autistic Disorder, Asperger's Disorder, Childhood Disintegrative Disorder, Pervasive Developmental Disorder Not Otherwise Specified) into one overarching diagnosis of "Autism Spectrum Disorder." This change aimed to better reflect the continuum of symptoms and presentations. The DSM-5 also introduced severity levels to specify the amount of support an individual needs.
Etiology and Risk Factors for ASD
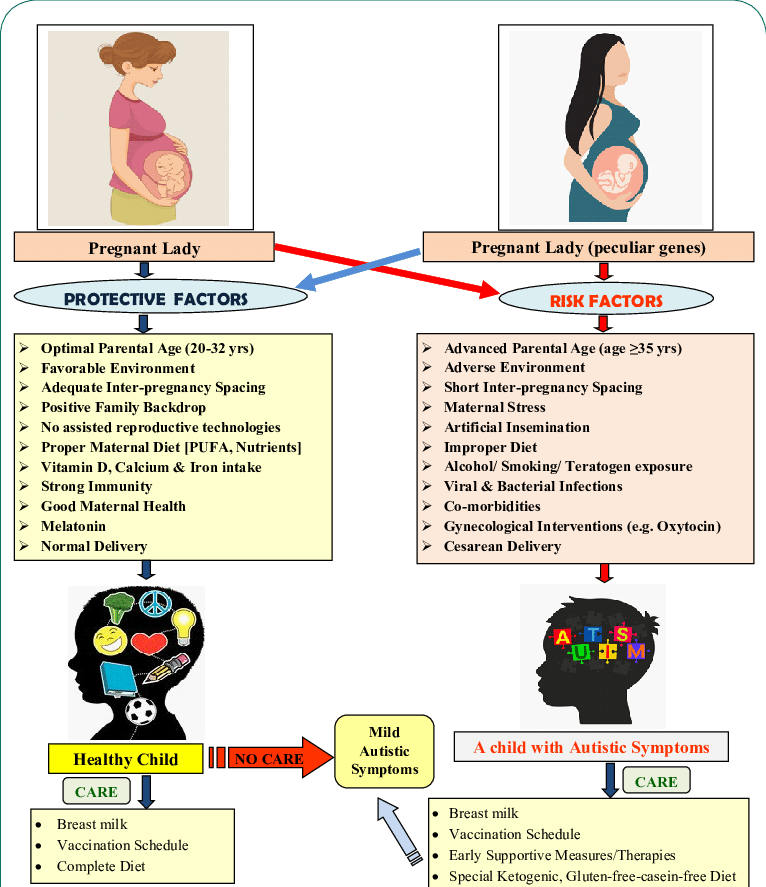
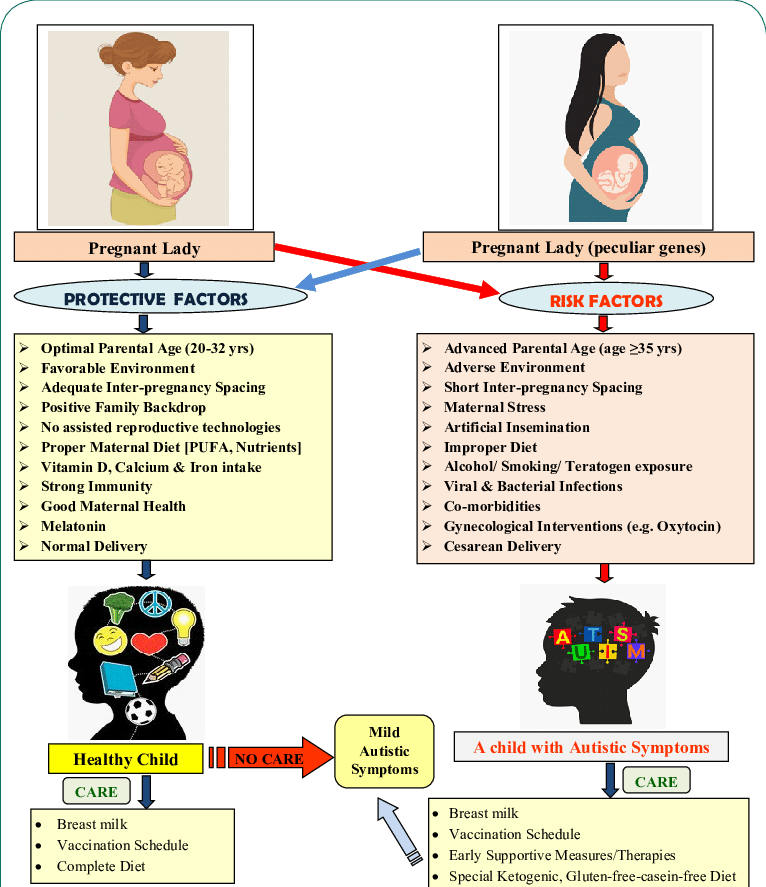
The widely accepted etiology of ASD is primarily genetic in origin, with a significant contribution from various environmental factors that interact with genetic predispositions.
I. Genetic Factors (Primary Contribution):
Genetics play the most substantial role in the etiology of ASD.
- Heritability: ASD has a high heritability rate, estimated to be between 70% and 90%. This means that genetic factors account for a large proportion of the variation in ASD susceptibility.
- Rare Genetic Variants: like De Novo Mutations: Genetic mutations that occur spontaneously in the egg or sperm cell, or during early embryonic development, and are not inherited from either parent. These can have a significant impact.
- Copy Number Variants (CNVs): Duplications or deletions of segments of DNA that can include multiple genes. Examples include deletions on chromosome 16p11.2, which are strongly associated with ASD.
- Single-Gene Disorders: A small percentage of ASD cases are directly linked to specific genetic syndromes (e.g., Fragile X syndrome, Rett syndrome, Tuberous Sclerosis Complex). These disorders have a known genetic cause and frequently present with ASD symptoms.
- Sibling Risk: If one child in a family has ASD, the risk of a subsequent child also having ASD is significantly higher than in the general population (around 2-18%, depending on the study and specific genetic factors).
- Twin Studies: High concordance rates in identical (monozygotic) twins (70-90%) compared to fraternal (dizygotic) twins (10-30%) strongly support a genetic basis.
II. Environmental Factors (Interact with Genetic Predisposition):
Environmental factors are not considered direct causes of ASD but rather as modulators that can interact with genetic vulnerabilities to influence the risk. The timing of exposure is often critical, typically during prenatal or early postnatal development.
Prenatal Factors:
- Maternal Illnesses: Certain maternal infections during pregnancy (e.g., rubella, cytomegalovirus) or metabolic conditions (e.g., gestational diabetes, maternal obesity, untreated celiac disease).
- Maternal Medications: Exposure to certain medications during pregnancy, such as valproate (an anti-epileptic drug) or thalidomide.
- Nutritional Deficiencies: Folic acid deficiency during the periconceptional period has been studied, with some evidence suggesting that adequate folic acid supplementation may reduce risk.
- Maternal-Paternal Age: Both advanced maternal and paternal age have been associated with a slightly increased risk of ASD.
- Birth Complications: Perinatal complications such as birth asphyxia, very low birth weight, and prematurity have been identified as risk factors, possibly due to their impact on brain development.
Environmental Toxins:
- Exposure to certain environmental toxins (e.g., air pollution, pesticides) during critical windows of neurodevelopment is an area of ongoing research, though their specific role in ASD etiology is not yet fully understood.
Important Clarifications and Misconceptions:
- Vaccines DO NOT Cause Autism: This myth has been thoroughly debunked by numerous large-scale, rigorous scientific studies around the world. Major medical and scientific organizations (e.g., CDC, WHO, AAP) have unequivocally stated that there is no link between vaccines (specifically the MMR vaccine or thimerosal) and ASD.
- ASD is NOT Caused by "Bad Parenting": This outdated and harmful theory has no scientific basis.
- It is NOT a "Choice" or a "Lifestyle": ASD is a biological disorder with complex neurodevelopmental underpinnings.
Diagnostic Criteria and Clinical Manifestations of ASD
The diagnosis of Autism Spectrum Disorder (ASD) is made based on specific behavioral criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). These criteria are divided into two main domains, both of which must be met for a diagnosis, alongside the onset of symptoms in early development and significant functional impairment.
I. Core Diagnostic Criteria (DSM-5):
A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (all three must be present):
- Deficits in social-emotional reciprocity: This refers to the back-and-forth nature of social interaction.
- Manifestations:
- Failure of normal back-and-forth conversation (e.g., not initiating or responding to social overtures).
- Reduced sharing of interests, emotions, or affect (e.g., not showing or bringing objects of interest to others).
- Lack of spontaneous seeking to share enjoyment, interests, or achievements with other people.
- Absence of reciprocal interaction (e.g., difficulty engaging in give-and-take play).
- Deficits in nonverbal communicative behaviors used for social interaction: This encompasses difficulties in using and understanding nonverbal cues that facilitate social communication.
- Manifestations:
- Poorly integrated verbal and nonverbal communication.
- Atypical eye contact (e.g., reduced, fleeting, or overly intense).
- Lack of facial expressions or very limited range of expressions, or inappropriate use of facial expressions.
- Atypical use of gestures (e.g., not pointing to share interest, unusual or repetitive gestures).
- Difficulty understanding body postures and gestures of others.
- Deficits in developing, maintaining, and understanding relationships: This criterion addresses challenges in forming and navigating social bonds beyond immediate family.
- Manifestations:
- Difficulties adjusting behavior to suit various social contexts (e.g., being overly formal with friends, too casual with authority figures).
- Difficulties in sharing imaginative play or making friends.
- Absence of interest in peers or struggles in understanding peer relationships.
- Difficulties with perspective-taking (understanding others' thoughts and feelings).
B. Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history:
- Stereotyped or repetitive motor movements, use of objects, or speech: These are actions that are often rigid, lacking apparent purpose, and repeated.
- Manifestations:
- Motor stereotypies: Simple motor stereotypies (e.g., hand flapping, finger flicking, body rocking), complex whole-body movements.
- Use of objects: Lining up toys, flipping objects, spinning wheels on toy cars in a non-functional way.
- Speech: Echolalia (immediate or delayed repetition of words/phrases), idiosyncratic phrases, repetitive questions.
- Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior: This reflects a need for predictability and resistance to change.
- Manifestations:
- Extreme distress at small changes (e.g., route to school, arrangement of items).
- Difficulties with transitions between activities.
- Rigid thinking patterns (e.g., needing to follow specific rules for a game exactly).
- Ritualized greetings or specific patterns in daily activities.
- Highly restricted, fixated interests that are abnormal in intensity or focus: These are passions that are often narrow in scope and pursued with an unusual level of dedication.
- Manifestations:
- Preoccupation with unusual objects (e.g., drains, fans, specific types of fabric).
- Excessively circumscribed or perseverative interests (e.g., an intense focus on train schedules, vacuum cleaner models, specific historical dates).
- These interests are often consuming and can interfere with other activities.
- Hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment: This refers to atypical responses to sensory stimuli.
- Manifestations:
- Hyperreactivity: Apparent indifference to pain/temperature, excessive smelling or touching of objects, visual fascination with lights or movement.
- Hyporeactivity: Adverse response to specific sounds (e.g., vacuum cleaner, fire alarms), textures (e.g., certain clothing), or tastes; resistance to grooming activities.
- Some individuals may seek out intense sensory experiences (e.g., deep pressure, spinning).
- C. Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life).
- D. Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
- E. These disturbances are not better explained by intellectual developmental disorder or global developmental delay. (Intellectual developmental disorder and ASD frequently co-occur; to make co-occurring diagnoses of ASD and intellectual developmental disorder, social communication should be below that expected for general developmental level).
II. Specifiers and Severity Levels:
The DSM-5 also includes specifiers to describe the individual's presentation:
- With or without accompanying intellectual impairment.
- With or without accompanying language impairment.
- Associated with a known medical or genetic condition or environmental factor.
- Associated with another neurodevelopmental, mental, or behavioral disorder.
- With catatonia.
Furthermore, severity levels are assigned for each of the two core domains, indicating the level of support an individual requires:
- Level 3: "Requiring very substantial support."
- Level 2: "Requiring substantial support."
- Level 1: "Requiring support."
Based on the degree of severity and level of support ASD are classified into 3 types.
| Severity level |
Social communication |
Restricted, repetitive behaviors |
Level 3
Requiring very substantial support |
- Severe deficits in verbal and non-verbal communication skills
- Severe impairment in functioning
- Very limited initiation of social interactions
- Minimal response to social overtures from others
|
- Inflexibility of behavior
- Extreme difficulty in coping with change
- Repeated behavior markedly interferes with functioning in all spheres
- Great distress/difficulty changing focus or action
|
Level 2
Requiring substantial support |
- Marked deficits in verbal and non-verbal communication skills
- Marked impairment in functioning
- Limited initiation of social interactions
|
- Difficulty in coping with change
- Distress/difficulty changing focus or action
- Repetitive behaviors occur frequently
|
Level 1
Requiring support |
- Without support, deficits in verbal and non-verbal communication skills
- Atypical and unusual social responses
|
- Interference with functioning in one or more context
- Problems of organization and planning hamper independence
|
Co-occurring Conditions (Comorbidities) with ASD
Comorbidity, or the simultaneous presence of two or more medical conditions in a patient, is exceptionally common in individuals with Autism Spectrum Disorder. These co-occurring conditions can significantly impact an individual's development, daily functioning, quality of life, and the complexity of their care.
I. Neurodevelopmental and Psychiatric Conditions:
- Attention-Deficit/Hyperactivity Disorder (ADHD):
- Prevalence: Very high, estimated to occur in 30-50% of individuals with ASD.
- Impact: Symptoms like inattention, impulsivity, and hyperactivity can worsen executive function difficulties, further impacting learning, social interactions, and daily living skills.
- Clinical Consideration: Distinguishing ADHD from ASD-related difficulties with focus or restlessness can be challenging but is important for appropriate intervention.
- Anxiety Disorders:
- Prevalence: Extremely common, affecting 40-80% of individuals with ASD. Includes Generalized Anxiety Disorder, Social Anxiety Disorder, Specific Phobias, Obsessive-Compulsive Disorder (OCD), and Panic Disorder.
- Impact: Can manifest as heightened distress in social situations, extreme reactions to changes in routine, specific fears (e.g., loud noises, certain objects), or repetitive behaviors driven by anxiety. OCD-like symptoms (e.g., compulsions) are often distinct from ASD's restricted, repetitive behaviors in their underlying motivation.
- Clinical Consideration: Anxiety can significantly interfere with learning, social engagement, and quality of life.
- Depression:
- Prevalence: Common, especially in adolescents and adults with ASD, with estimates ranging from 10-70%.
- Impact: Can present with typical depressive symptoms (sadness, anhedonia, sleep/appetite changes) but may also manifest atypically (e.g., increased irritability, aggression, withdrawal, or exacerbation of repetitive behaviors).
- Clinical Consideration: Often underdiagnosed in ASD due to communication challenges and atypical presentation. Suicide risk can be elevated.
- Intellectual Developmental Disorder (IDD):
- Prevalence: Approximately 30-50% of individuals with ASD also have IDD.
- Impact: IDD significantly impacts cognitive and adaptive functioning, influencing learning capacity, communication strategies, and the level of support required.
- Clinical Consideration: When both are present, social communication deficits should be below that expected for the general developmental level.
- Language Disorders:
- Prevalence: High.
- Impact: Can range from being nonverbal to having fluent but pragmatically impaired speech.
- Tourette Syndrome/Tic Disorders:
- Prevalence: More common in ASD than in the general population.
- Impact: Involuntary motor or vocal tics can add to functional challenges and social difficulties.
II. Medical and Physical Conditions:
- Epilepsy/Seizure Disorders:
- Prevalence: Significantly higher in individuals with ASD, affecting approximately 20-30%, compared to 1% in the general population. The risk increases with intellectual disability.
- Impact: Seizures can significantly impair cognitive function, safety, and quality of life.
- Clinical Consideration: Screening for seizure activity is important, as some seizure types (e.g., absence seizures) can be subtle.
- Gastrointestinal (GI) Issues:
- Prevalence: Highly prevalent, with estimates ranging from 9-90%. Includes chronic constipation, diarrhea, abdominal pain, reflux, and feeding difficulties.
- Impact: GI discomfort can contribute to irritability, sleep disturbances, and challenging behaviors, especially in nonverbal individuals who cannot express their pain.
- Clinical Consideration: Careful assessment of diet, stool patterns, and GI symptoms is crucial.
- Sleep Disturbances:
- Prevalence: Very common, affecting 40-80% of individuals with ASD. Includes difficulty falling asleep, frequent night awakenings, and altered sleep architecture.
- Impact: Chronic sleep deprivation can exacerbate behavioral challenges, attention deficits, anxiety, and impact overall family functioning.
- Clinical Consideration: Behavioral interventions and sometimes pharmacological approaches are used.
- Sensory Processing Differences:
- Prevalence: Nearly universal in ASD, though not a standalone diagnosis in DSM-5.
- Impact: Hyper- or hyporeactivity to sensory stimuli can lead to sensory overload, distress, avoidance behaviors, or sensory-seeking behaviors, profoundly affecting daily routines and participation.
- Clinical Consideration: Integrated into many therapeutic approaches (e.g., Occupational Therapy).
- Feeding Issues and Nutritional Deficiencies:
- Prevalence: Common due to sensory sensitivities, rigid food preferences, and GI issues.
- Impact: Can lead to inadequate nutrition, growth concerns, and increased family stress.
- Obesity and Metabolic Syndrome:
- Prevalence: Higher risk, particularly in adults with ASD, due to medication side effects, sedentary lifestyles, and restrictive diets.
Nursing Diagnoses for Individuals with ASD
For individuals with Autism Spectrum Disorder (ASD), nursing diagnoses address the specific challenges related to their social communication deficits, restricted/repetitive behaviors, sensory processing differences, and common comorbidities.
I. Communication and Social Interaction Related Diagnoses:
- Impaired Social Interaction
- Related to: Altered neurological development affecting social cognition, difficulty understanding social cues, expressive language deficits, rigid adherence to routines.
- As evidenced by: Lack of eye contact, limited reciprocal social gestures, absence of interest in peers, difficulty initiating or maintaining conversations, limited shared enjoyment, inappropriate social responses.
- Impaired Verbal Communication
- Related to: Altered neurological processing, developmental delay, limited ability to express needs/emotions, difficulty with abstract concepts.
- As evidenced by: Absence of speech, limited vocabulary, echolalia, tangential or repetitive speech, difficulty using nonverbal cues to supplement communication, inability to understand or use social pragmatics.
- Risk for Impaired Social Interaction (for younger children or those with milder presentations)
- Related to: Limited opportunities for social engagement, parental anxiety, lack of understanding of social norms.
- As evidenced by: (Potential for) isolation, difficulty forming friendships, social withdrawal.
II. Behavioral and Emotional Regulation Related Diagnoses:
- Disturbed Thought Processes
- Related to: Altered neurological processing, difficulty with abstract thinking, concrete interpretation of language, preoccupation with specific interests.
- As evidenced by: Rigid adherence to routines, difficulty with transitions, repetitive questions, literal interpretation of language, limited insight into social situations.
- Risk for Self-Mutilation / Risk for Other-Directed Violence
- Related to: Inability to verbally express needs/frustration/pain, sensory overload, anxiety, impulsivity, communication deficits, change in routine.
- As evidenced by: (Potential for) head banging, biting self, scratching, hitting others, property destruction, aggression. Note: These are serious risks and often require immediate intervention and careful assessment of triggers.
- Excessive Anxiety
- Related to: Sensory overload, fear of change, difficulty processing unpredictable situations, social communication challenges, inability to express concerns.
- As evidenced by: Increased repetitive behaviors, withdrawal, irritability, agitation, sleep disturbances, physiological signs of distress (e.g., increased heart rate, sweating).
- Maladaptive Coping
- Related to: Limited problem-solving skills, difficulty with emotional regulation, rigidity in thinking, sensory sensitivities.
- As evidenced by: Increased repetitive behaviors, tantrums, aggression, withdrawal when faced with stress or change, difficulty adapting to new situations.
III. Self-Care and Daily Living Related Diagnoses:
- Impaired Home Maintenance (often for family)
- Related to: Complexity of care for child with ASD, need for structured environment, high energy demands of child.
- As evidenced by: Disorganized home environment, family fatigue, frequent changes to daily schedule to accommodate child's needs.
- Feeding Self-Care Deficit
- Related to: Sensory sensitivities (texture, taste, smell), ritualistic eating patterns, difficulty adapting to new foods, G.I. issues.
- As evidenced by: Refusal of certain foods, extremely limited food repertoire, malnutrition, weight loss/gain.
- Sleep Pattern Disturbance
- Related to: Altered neurological function, anxiety, sensory sensitivities (noise, light), lack of consistent bedtime routines, medication side effects.
- As evidenced by: Difficulty initiating or maintaining sleep, frequent night awakenings, restless sleep, daytime fatigue, behavioral problems due to lack of sleep.
IV. Family-Focused Diagnoses:
- Compromised Family Coping
- Related to: Chronic stress of caring for a child with special needs, limited support systems, financial burdens, difficulty managing challenging behaviors.
- As evidenced by: Verbalization of helplessness, family role disruption, impaired communication among family members, neglectful care of other family members.
- Caregiver Role Strain
- Related to: Complexity of care, demands of therapies and appointments, lack of respite, emotional and physical burden.
- As evidenced by: Caregiver fatigue, withdrawal, expressions of frustration or anger, health problems of caregiver, difficulty performing care activities.
Interventions and Management Strategies for ASD
The management of Autism Spectrum Disorder is highly individualized, multifaceted, and involves a combination of behavioral, educational, developmental, medical, and family-focused interventions.
I. Aims of Management:
- Promoting Communication and Social Interaction: Fostering the ability to express needs, understand others, and engage in meaningful relationships.
- Reducing Challenging Behaviors: Addressing behaviors that impede learning, social integration, or safety (e.g., aggression, self-injury, severe tantrums).
- Supporting Cognitive and Behavioral Development: Enhancing learning, problem-solving, adaptive skills, and emotional regulation.
- Optimizing Outcomes Through Early Intervention: Early identification and the initiation of appropriate interventions as early as possible are crucial.
II. Interventions and Therapeutic Approaches:
- Behavioral Therapies (e.g., Applied Behavior Analysis - ABA): A highly structured and intensive intervention based on learning theory, utilizing systematic methods to teach new skills (e.g., communication, social, self-help, academic) and decrease undesirable behaviors by analyzing antecedents, behaviors, and consequences (ABC model).
- Speech and Language Therapy (SLT): Addresses a wide range of communication challenges, from developing spoken language to improving pragmatic (social) language skills. Uses techniques like Picture Exchange Communication System (PECS), Augmentative and Alternative Communication (AAC) devices, and social stories.
- Occupational Therapy (OT):: Addresses fine and gross motor skills, visual-perceptual skills, and sensory processing differences, helping individuals adapt to their environment and develop self-care skills.
- Physical Therapy (PT): Focuses on gross motor skills, balance, coordination, and motor planning.
- Developmental, Individual Difference, Relationship-based (DIR) Model / Floortime: Focuses on building foundational capacities for relating, communicating, and thinking by following the child's lead and engaging them in activities they enjoy, emphasizing emotional development and interaction.
- Treatment and Education of Autistic and Related Communication-Handicapped Children (TEACCH): A structured teaching approach utilizing visual supports (schedules, task organizers, clearly defined areas) to make the environment predictable and understandable.
III. Pharmacological Management:
Medications do not treat the core symptoms of ASD but can be effective in managing co-occurring conditions and challenging behaviors that significantly impair functioning.
- Atypical Antipsychotics (Risperidone, Aripiprazole):
- Use: approved for irritability associated with ASD (e.g., aggression, self-injury, temper tantrums).
- Considerations: Significant side effects (weight gain, metabolic issues, sedation).
- SSRIs (Selective Serotonin Reuptake Inhibitors):
- Use: Often used off-label for anxiety, OCD-like behaviors, and repetitive behaviors.
- Considerations: Monitor for side effects (agitation, sleep disturbances).
- Stimulants (Methylphenidate, Amphetamines):
- Use: To manage symptoms of co-occurring ADHD.
- Considerations: May exacerbate anxiety or tics in some individuals with ASD.
- Other Medications: For sleep disturbances (e.g., melatonin), seizures (anti-epileptics), or severe mood dysregulation.
IV. Nursing Interventions for Symptom Management and Support:
- Promote Communication Skills:
- Encourage and support the development of communication skills using visual aids, augmentative and alternative communication (AAC) devices, and social stories.
- Provide a communication-friendly environment and use simple, short, and concise language to facilitate understanding.
- Repeat instructions, provide explanations and clarifications, and avoid assuming understanding.
- Implement Structure and Routine:
- Establish consistent routines and visual schedules to provide predictability and reduce anxiety.
- Help the child understand and follow daily routines through visual cues and verbal prompts.
- Introduce one activity at a time and be specific while teaching skills.
- Manage Sensory Sensitivities:
- Create a sensory-friendly environment by reducing excessive noise, bright lights, and other sensory triggers.
- Offer sensory breaks or provide sensory tools like fidget toys or weighted blankets to help the child self-regulate.
- Support Social Interaction:
- Facilitate social interactions by creating opportunities for the child to engage with peers, such as structured play activities or social groups.
- Teach and reinforce appropriate social skills (e.g., good eye contact, smiling, helping others).
- Train social skills and reward positive behaviors.
- Provide Emotional Support and Behavior Management:
- Recognize and address the emotional needs of the child with ASD. Use calming techniques, such as deep breathing exercises or sensory input, to help manage anxiety or emotional distress.
- Develop a trusting relationship with the child and convey acceptance of the child separate from the unacceptable behavior.
- Develop a symptom management plan for the child, including improving communication, promoting good social interaction, enhancing the child’s interests, and reducing repetitive behaviors.
- Create tasks with a high chance of success, such as guided play and introducing stimulative activities with rewards.
- Ensure the child’s attention by calling their name and establishing eye contact before giving instructions.
- Facilitate Self-Care Skills:
- Teach and encourage age-appropriate self-care skills, such as grooming, dressing, and feeding.
- Use visual cues and step-by-step instructions to assist the child in developing independence and promoting self-confidence.
- Simplify activities and teaching techniques when necessary.
- Provide assistance during task performance.
- Be patient and tolerant. Gradually decrease assistance and the number of assistants, while assuring the patient that assistance is still available when necessary.
V. Family Support and Education (Crucial for Long-Term Success):
- Comprehensive Family Education:
- Provide support and education to families, including accurate and up-to-date information about ASD, available resources, and effective strategies for managing challenges at home.
- Educate the child and family on the use of psycho stimulants (if prescribed) and practice strategies for dealing with the child’s behaviors.
- Provide information and materials related to the child’s disorder and effective parenting techniques to the parents or guardians, using written or verbal step-by-step explanations.
- Coping Strategies and Resources:
- Offer guidance on coping strategies, community resources, and access to support groups.
- Be sensitive to parents’ needs, as they often experience exhaustion of parental resources due to prolonged coping with the child. Assess parenting skill levels, considering intellectual, emotional, physical strengths, and limitations.
- Advocacy:
- Advocate for the child's needs within healthcare and educational settings.
- Serve as an advocate for the child with ASD and ensure their needs are met in various settings (school, community, healthcare). Communicate with teachers, caregivers, and other professionals to promote understanding and inclusion.
VI. Coordinated and Individualized Care:
- Individualized Care Plans:
- Collaborate with families, educators, and therapists to develop personalized plans that address the unique strengths and challenges of each individual. These plans include specific goals, strategies, and accommodations to optimize the individual’s functioning and well-being.
- Coordinate overall treatment plans with schools, collateral personnel, the child, and the family.
- Multidisciplinary Team Collaboration:
- Work closely with the child’s healthcare team, including therapists, psychologists, and educators, to ensure coordinated and comprehensive care. Share relevant information and collaborate on treatment plans and interventions.
Role of the Nurse in the Care of Individuals with ASD
The nurse plays a role in the care of individuals with Autism Spectrum Disorder (ASD), serving as a clinician, educator, advocate, coordinator, and supporter throughout the individual's life journey.
I. Early Identification and Screening (Infancy/Early Childhood):
- Developmental Surveillance: Nurses are often the first point of contact in primary care settings (e.g., well-child visits). They conduct ongoing developmental surveillance, observing children, listening to parental concerns about atypical development (e.g., lack of eye contact, delayed speech, repetitive behaviors), and monitoring milestones.
- ASD-Specific Screening: Administering and interpreting standardized screening tools like the M-CHAT-R/F at recommended ages (18 and 24 months).
- Referral: Recognizing "red flags" and making timely referrals for comprehensive diagnostic evaluations to specialists (e.g., developmental pediatricians, child psychologists). Early referral is critical for early intervention.
II. Diagnosis and Initial Management (Childhood):
- Emotional Support and Education: Providing emotional support to families receiving an ASD diagnosis, which can be overwhelming. Educating parents about ASD, explaining the diagnosis in understandable terms, and dispelling myths.
- Information Provision: Supplying accurate and evidence-based information about ASD, available therapies, resources, and support groups.
- Care Coordination: Initiating the coordination of care among the multidisciplinary team (e.g., developmental pediatricians, psychologists, speech therapists, occupational therapists, educators).
- Baseline Assessment: Conducting comprehensive nursing assessments to establish a baseline of the child's communication, social, behavioral, self-care, and sensory needs.
III. Intervention and Ongoing Management (Childhood and Adolescence):
- Implementing Nursing Interventions:
- Promoting Communication: Using visual aids, AAC, social stories; employing simple, concise language; ensuring attention before giving instructions; repeating and clarifying.
- Establishing Structure and Routine: Helping families implement consistent schedules and visual cues to reduce anxiety and manage transitions.
- Managing Sensory Sensitivities: Identifying sensory triggers and strategies (e.g., creating a sensory-friendly environment, providing sensory tools, advocating for sensory breaks).
- Supporting Social Interaction: Facilitating structured social opportunities and reinforcing appropriate social behaviors.
- Behavioral Management: Collaborating with behavioral therapists (e.g., ABA providers), educating families on behavior modification techniques, and developing symptom management plans for challenging behaviors. Developing trusting relationships and conveying acceptance.
- Self-Care Skill Development: Teaching and reinforcing age-appropriate self-care skills (e.g., hygiene, dressing, feeding) using step-by-step instructions and visual supports.
- Medication Management: Monitoring effectiveness and side effects of prescribed medications for co-occurring conditions (e.g., anxiety, ADHD, seizures, irritability), educating families on proper administration.
- Advocacy: Advocating for the child's educational needs, ensuring appropriate IEPs are in place, and promoting inclusion in school and community settings.
- Family Support: Assessing caregiver role strain, providing guidance on coping strategies, connecting families to support groups, and providing respite resources. Being sensitive to parents' needs and providing practical parenting techniques.
IV. Transition to Adulthood and Adult Care:
- Transition Planning: Assisting individuals and families in navigating the complex transition from pediatric to adult healthcare services. This includes planning for independent living, vocational training, higher education, and continued therapies.
- Health Promotion: Educating on general health maintenance, healthy lifestyle choices, and preventive care, considering common comorbidities in adults with ASD (e.g., obesity, metabolic syndrome).
- Sexual Health Education: Providing age-appropriate education on sexual health, consent, and safe practices, addressing unique communication and social understanding challenges.
- Mental Health Support: Continuing to monitor for and address mental health conditions such as anxiety and depression, which can be highly prevalent in adults with ASD.
- Vocational Support: Advocating for job coaching, supported employment programs, and workplace accommodations.
- Community Integration: Facilitating involvement in community activities, promoting independence, and addressing ongoing social support needs.
V. General Roles of the Nurse Across the Lifespan:
- Care Coordinator/Navigator: Serving as a central point of contact for families, helping them navigate complex healthcare and educational systems, scheduling appointments, and ensuring continuity of care.
- Educator: Providing ongoing education to the individual with ASD (at their developmental level), family members, and other healthcare providers about ASD, its management, and specific strategies.
- Advocate: Championing the rights and needs of individuals with ASD, ensuring access to appropriate services, accommodations, and promoting understanding and acceptance within society.
- Counselor/Support Person: Offering emotional support, active listening, and guidance to individuals with ASD and their families, especially during challenging times.
- Clinical Expertise: Utilizing specialized knowledge of ASD to anticipate needs, identify potential problems, and implement appropriate interventions.
- Collaboration: Working effectively as part of a multidisciplinary team to ensure holistic and integrated care.