Social Aspects of Diseases and Hospitalization
Social Aspects of Diseases and Hospitalization
Medical sociology is a field that deeply explores how social factors influence health, illness, and healthcare systems. It moves beyond a purely biological view of disease to understand the broader human experience of sickness.
Social Aspects of Diseases
Illness is never just a biological event confined to the individual body; it is profoundly shaped by and, in turn, shapes social realities. Understanding the social aspects of diseases is critical for comprehensive care.
A. Differences Between Social Medicine and Curative Medicine
It's vital to distinguish between these two approaches to health, as both are necessary but focus on different dimensions of well-being.
- Focus: Primarily on treating existing diseases and symptoms. It identifies pathogens, physiological dysfunctions, and aims to restore health through medical interventions (drugs, surgery, therapies).
- Approach: Individualistic and reductionist. It often views the patient as a biological entity and disease as a deviation from normal biological functioning.
- Role of Patient: Often passive recipient of treatment.
- Interventions: Clinical diagnosis, pharmacological treatments, surgical procedures, and other direct medical interventions.
- Example: Prescribing antibiotics for a bacterial infection, performing surgery to remove a tumor, administering insulin for diabetes.
- Focus: Examines the social, economic, cultural, environmental, and political factors that cause or influence health and disease. It looks at the "causes of the causes" of illness.
- Approach: Holistic, population-based, and considers the broader determinants of health. It recognizes that illness is shaped by living and working conditions, social inequalities, and access to resources.
- Role of Patient/Community: Active participant in health promotion, disease prevention, and addressing social determinants.
- Interventions: Public health policies, community-based interventions, advocacy for social justice, addressing poverty, education, housing, and access to healthcare services.
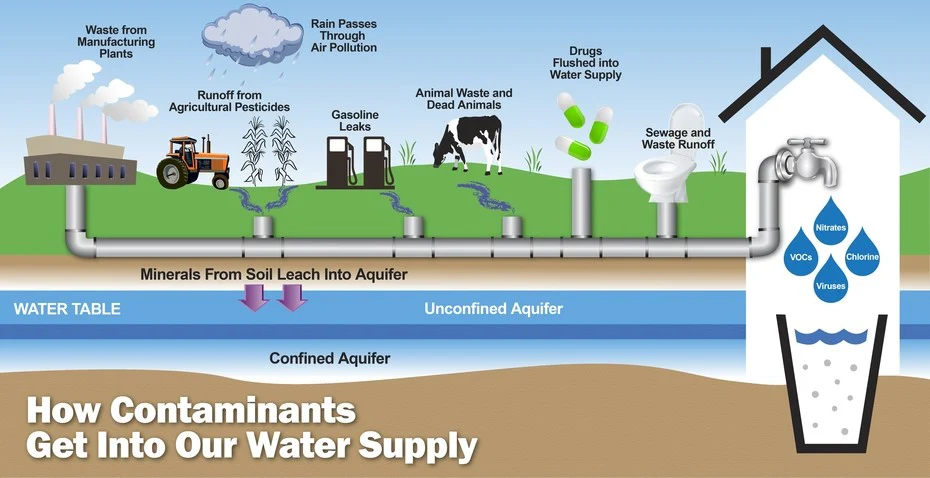
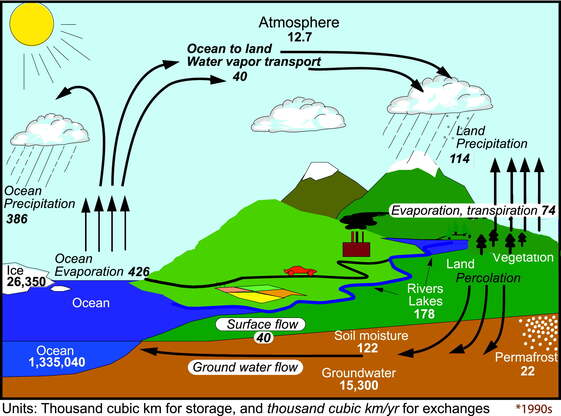
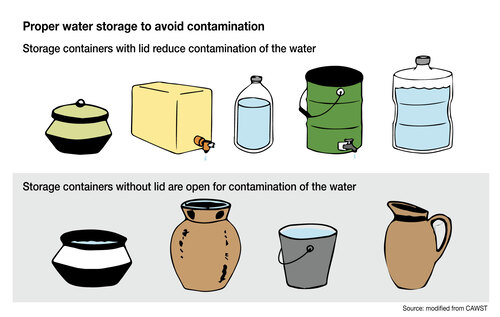
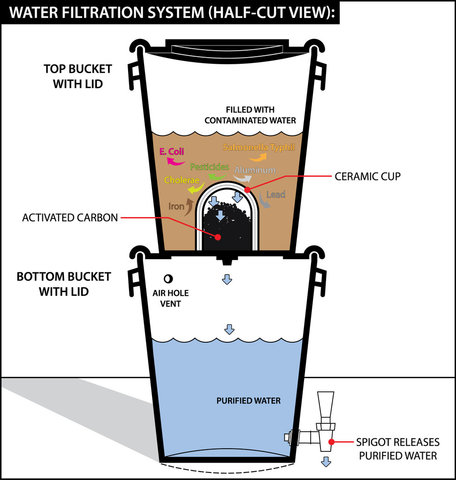
- Example: Campaigning for clean water access to prevent cholera, implementing nutrition programs to combat malnutrition, advocating for better housing to reduce respiratory illnesses, understanding how unemployment contributes to mental health issues.
Synergy: While distinct, these two approaches are complementary. Effective healthcare requires both excellent curative medicine to treat the sick and robust social medicine to prevent illness and promote health across populations.
B. Importance of Social Medicine
Social medicine is paramount for several reasons, especially in nursing:
- Holistic Patient Care: It allows nurses to view patients not just as a collection of symptoms but as individuals embedded in social contexts. Understanding these contexts helps in planning more effective and compassionate care.
- Disease Prevention: By identifying and addressing the social roots of disease (e.g., poverty, poor sanitation, lack of education), social medicine contributes significantly to primary prevention, reducing the incidence of illness in the first place.
- Health Equity and Social Justice: It highlights health disparities and inequalities, advocating for policies and interventions that promote fairness and equal opportunities for health for all members of society.
- Community Health Improvement: Social medicine shifts focus from individual treatment to community-wide health promotion, leading to healthier populations and stronger social structures.
- Sustainable Health Outcomes: Addressing social determinants leads to more lasting health improvements compared to solely treating symptoms, which often recur if underlying social issues persist.
- Relevance in Nursing: Nurses are often at the frontline, witnessing the impact of social determinants daily. Social medicine provides a framework for nurses to advocate for patients, participate in public health initiatives, and understand the broader factors influencing their patients' health trajectories. It fosters a desired attitude of empathy, advocacy, and a commitment to addressing the root causes of illness.
Social Aspects of Hospitalization
Hospitalization is a significant social experience that can profoundly impact an individual's well-being beyond their immediate physical illness. Understanding these impacts is crucial for patient-centered care and effective patient management.
A. Discussion of the Social Effects of Hospitalization and Appropriate Management
- Effect: Patients often feel stripped of their personal identity, roles (e.g., parent, worker), and control over their daily lives. They become "the patient in bed 3" rather than a unique individual. Routines are dictated, privacy is limited, and personal choices diminish.
- Management: Address patients by their preferred name. Encourage personal belongings. Involve them in decision-making about their care as much as possible. Respect privacy during procedures and discussions. Maintain communication with their family/social support.
- Effect: Patients may struggle to fulfill their normal social roles (e.g., provider, caregiver). Family members might have to take on new, unfamiliar roles, leading to stress and disruption within the family unit.
- Management: Acknowledge and validate the patient's concerns about their roles. Facilitate communication with family about temporary role adjustments. Connect patients with social workers or support groups if role strain is severe.
- Effect: Being away from family, friends, and familiar social environments can lead to feelings of loneliness, boredom, and isolation, particularly for long-term patients.
- Management: Encourage regular visiting hours. Facilitate virtual connections (video calls) if possible. Engage patients in therapeutic activities. Promote interaction with other compatible patients if appropriate. Provide emotional support and opportunities for conversation.
- Effect: Some conditions (e.g., mental illness, infectious diseases like HIV, certain chronic conditions) can carry social stigma, leading to patients feeling judged, isolated, or discriminated against within the hospital setting or upon discharge.
- Management: Provide empathetic and non-judgmental care. Educate staff to avoid stigmatizing language or behavior. Advocate for patient rights and confidentiality. Connect patients with support groups for their specific condition.
- Effect: In a hospital, intimate bodily functions are often exposed, and personal information is discussed openly, leading to feelings of embarrassment, loss of dignity, and vulnerability.
- Management: Always ensure patient privacy during examinations, personal care, and discussions. Use screens or draw curtains. Knock before entering. Explain procedures before performing them. Maintain confidentiality of patient information.
- Effect: Patients may become overly dependent on staff for basic needs, leading to a sense of helplessness or being treated like a child, especially if they are elderly or have cognitive impairments.
- Management: Promote independence where safe and possible. Encourage patients to participate in their own care. Offer choices. Use age-appropriate language and communication. Empower patients to make decisions.
- Effect: Hospitalization can disrupt established social support systems. Family and friends might face challenges in visiting or providing support due to distance, work, or lack of resources.
- Management: Facilitate communication with family. Provide information and support to caregivers. Connect families with hospital resources (e.g., social work, counseling).
B. Description of Specific Effects of Hospitalization
Hospitalization impacts individuals in interconnected social, economic, and physical ways.
- Loss of identity, autonomy, privacy.
- Social isolation and loneliness.
- Role strain and disruption of family dynamics.
- Potential for stigma and discrimination.
- Dependence and changes in self-perception.
- Disruption of usual social routines and activities.
- Direct Costs: Hospital bills, medication costs, specialist fees, transportation to and from the hospital.
- Indirect Costs (Loss of Income): Loss of wages for the patient due to inability to work. Loss of wages for family members who take time off work for caregiving or visiting.
- Burden on Family Resources: Families may need to spend money on food, accommodation near the hospital, and other necessities. This can lead to significant financial strain, especially for low-income families.
- Long-term Financial Impact: For chronic illnesses or prolonged hospital stays, there can be long-term financial consequences, including medical debt, depletion of savings, and even poverty.
- Deconditioning/Muscle Atrophy: Prolonged bed rest can lead to muscle weakness, loss of endurance, and physical deconditioning.
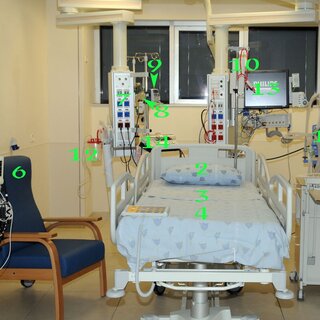
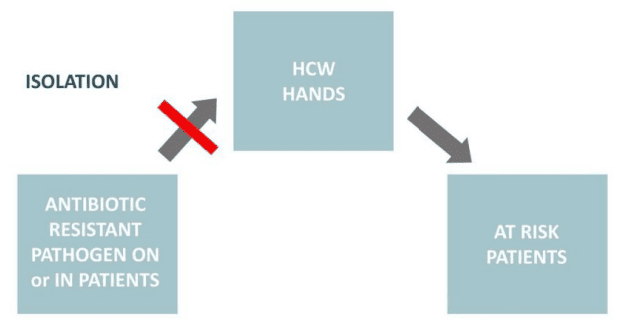
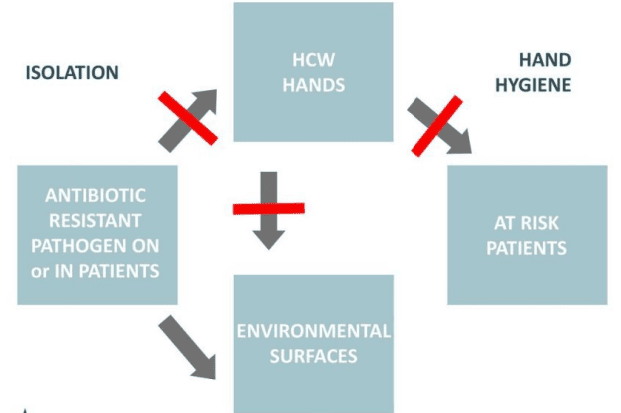
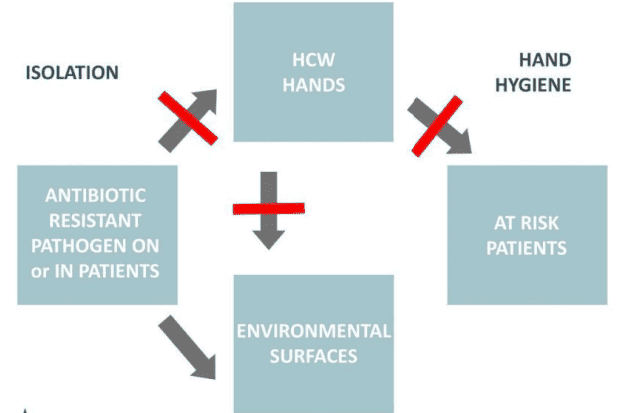
- Increased Risk of Infections: Hospital-acquired infections (HAIs) like C. difficile, MRSA, UTIs, and pneumonia are significant risks due to exposure to various pathogens.
- Sleep Disturbances: The hospital environment (noise, light, frequent interruptions for vital signs/meds) often disrupts normal sleep patterns, leading to fatigue and delayed recovery.
- Pain and Discomfort: Patients often experience pain related to their condition, procedures, or recovery, which can impact their physical and mental state.
- Nutritional Deficiencies: Poor appetite, specific dietary restrictions, or difficulty eating can lead to malnutrition, slowing recovery.
- Skin Breakdown: Immobility increases the risk of pressure ulcers (bedsores).
- Delirium/Cognitive Changes: Especially in older adults, the unfamiliar hospital environment, medication effects, and illness can lead to acute confusion or delirium.
- Complications from Procedures/Medications: Risks associated with medical interventions, including side effects from drugs, adverse reactions, or complications from surgery.
C. The Role of Social Aspects During Patient Management
Integrating social aspects into patient management is fundamental for holistic, patient-centered, and effective care. This requires nurses and healthcare teams to:
- Conduct a Thorough Social Assessment: Beyond medical history, inquire about living situation, family support, employment, financial concerns, cultural beliefs, social activities, and community connections.
- Involve Family and Social Support: Recognize the family as part of the care unit. Facilitate their involvement in care planning, education, and decision-making (with patient consent).
- Provide Culturally Competent Care: Understand and respect the patient's cultural background, beliefs, and practices regarding health, illness, and treatment. Adapt care to align with cultural values where appropriate.
- Address Communication Barriers: Use plain language, interpreters if needed, and assess health literacy. Ensure patients understand their condition, treatment plan, and discharge instructions.
- Facilitate Continuity of Care and Discharge Planning: Plan early for discharge, considering the patient's home environment, social support, and access to post-hospital care (e.g., home health, rehabilitation, community resources). This prevents readmissions.
- Connect Patients with Resources: Refer patients to social workers, financial counselors, spiritual care, support groups, and community services that can address their social and economic needs.
- Promote Patient Autonomy and Dignity: Empower patients to participate in their care, make informed decisions, and maintain their sense of self-worth despite illness or disability.
- Advocate for Patients: Speak up for patients' rights, needs, and preferences, especially when they are vulnerable or unable to advocate for themselves.
- Educate About Lifestyle and Social Determinants: Help patients understand how their social environment and lifestyle choices impact their health, and guide them towards healthier behaviors within their social context.
- Consider Psychological and Emotional Well-being: Recognize and address the emotional toll of illness and hospitalization (anxiety, depression, fear), which are often intertwined with social factors.
By actively considering and managing the social aspects, healthcare professionals can significantly improve patient outcomes, reduce suffering, and contribute to overall well-being.
Urbanization and Delivery of Health Services
Urbanization, the process by which populations shift from rural to urban areas, is a global phenomenon with profound implications for all aspects of society, including the provision and access to health services. Sociologists view urbanization as a dynamic product of human endeavor and societal development.
Understanding Urbanization
- Definition: Urbanization is the process of becoming urban, characterized by the movement of people into cities and towns, and a shift from agricultural livelihoods to industrial, commercial, and service-based economies. It is an area where a maximum number of people are engaged in non-agricultural activities.
- Dual Nature of Urban Life: While often seen as a symbol of progress and civilization ("man built the city and the city in turn made man civilized"), urban areas simultaneously present both immense opportunities (hope) and significant challenges (despair).
- Complexity of Urban Life: Urban areas are characterized by increased social interaction and extraordinary complexities in social life and relationships. The concept of constant change is a defining feature of urban environments.
Dimensions of Urbanization, Technology, Economic, and Socio Development in Health Service Delivery
Urbanization, alongside advancements in technology, economic growth, and broader socio-development, profoundly influences the structure, accessibility, and quality of health service delivery.
A. Urbanization's Influence on Health Service Delivery:
- Concentration of Resources: Urban areas typically attract and concentrate healthcare infrastructure, specialized personnel, advanced technology, and pharmaceutical industries, leading to more diverse and high-level medical services.
- Increased Demand: High population density leads to increased demand for health services, necessitating robust and scalable healthcare systems.
- Emergence of Specialized Services: The critical mass of patients and professionals in urban centers allows for the development of highly specialized medical fields and tertiary care hospitals.
- Accessibility Challenges: Despite concentration, access can be uneven due to traffic congestion, cost of transport, and geographical distribution of facilities, especially for residents in slums or peripheral areas.
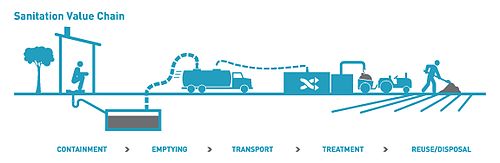
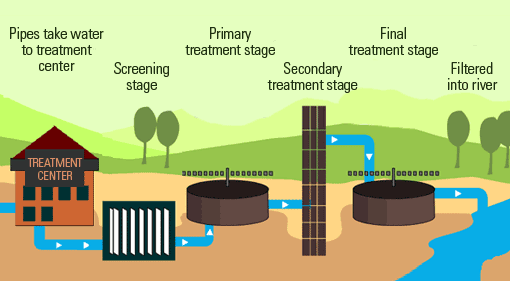
- Public Health Challenges: Urbanization brings unique public health challenges like sanitation, waste management, pollution, and the rapid spread of infectious diseases, requiring specialized public health interventions within the health service delivery framework.
B. Technology's Role in Health Service Delivery:
- Diagnostic and Treatment Advancements: Technology drives the development of advanced diagnostic tools (e.g., MRI, CT scans) and sophisticated treatment modalities (e.g., robotic surgery, targeted therapies), largely concentrated in urban centers.
- Information Technology (IT) in Healthcare: Electronic Health Records (EHRs), telemedicine, and health information systems streamline operations, improve data management, and facilitate remote consultations, expanding reach even to underserved urban populations.
- Medical Devices and Equipment: Urban health facilities typically have access to cutting-edge medical equipment, improving the precision and effectiveness of care.
- Challenges: High cost of technology, the need for skilled personnel to operate and maintain it, and the digital divide (unequal access to technology) can create disparities.
C. Economic Development's Impact on Health Service Delivery:
- Funding for Healthcare: Economic growth typically leads to increased government revenue and private wealth, allowing for greater investment in healthcare infrastructure, research, and workforce development.
- Insurance and Affordability: Developed economies often have more comprehensive health insurance systems, making healthcare services more affordable and accessible to a larger segment of the population.
- Private Sector Growth: Economic development encourages the growth of private healthcare providers, offering more choices but potentially exacerbating inequalities if not properly regulated.
- Income Disparities: Despite overall economic growth, income inequalities within urban areas can lead to significant disparities in access to quality health services, with the poor often relying on overburdened public facilities.
D. Socio-Development's Influence on Health Service Delivery:
- Education and Health Literacy: Higher levels of education and health literacy associated with socio-development enable populations to better understand health information, engage in preventative care, and navigate complex health systems.
- Social Capital and Networks: Strong social networks within communities can facilitate health promotion and support adherence to treatment. However, urban anonymity can sometimes weaken these networks.
- Lifestyle Changes: Socio-development often brings changes in lifestyle (e.g., diet, physical activity, stress levels) which in turn affect disease patterns (e.g., increase in non-communicable diseases) and demand different types of health interventions.
- Demand for Quality: As societies develop, there is an increased demand for higher quality, patient-centered, and ethically responsible healthcare services.
Relevance of Urbanization in Providing Healthcare to Patients
Urbanization is highly relevant to healthcare provision, presenting both significant advantages and complex challenges that healthcare systems must address:
- Centralized Access: Easier access for many to a wide range of medical specialists, hospitals, and diagnostic centers due to their concentration in urban areas.
- Advanced Facilities: Urban centers are hubs for advanced medical technology and cutting-edge research, offering state-of-the-art treatment options.
- Specialized Expertise: A greater pool of medical professionals, including highly specialized doctors and nurses, is available.
- Emergency Services: Better-equipped and faster emergency response systems are typically found in urban settings.
- Public Health Interventions: Easier to implement mass vaccination campaigns, health education programs, and surveillance systems in densely populated areas.
- Health Disparities: Significant health inequalities exist within urban areas, often correlating with socio-economic status. Slum dwellers and the urban poor often face severely limited access to quality care.
- Overburdened Services: Rapid urbanization can overwhelm existing healthcare infrastructure, leading to long waiting times, overcrowded facilities, and compromised quality of care.
- Specific Health Risks: Urban environments contribute to health issues like air pollution-related respiratory diseases, stress-related mental health disorders, road traffic accidents, and the rapid spread of infectious diseases.
- Lifestyle Diseases: Urban lifestyles often contribute to non-communicable diseases such as diabetes, hypertension, and heart disease due to sedentary habits and dietary changes.
- Social Problems Impacting Health: Homelessness, poverty, substance abuse, and crime are more prevalent in urban areas and directly impact health outcomes and access to care.
- "Urban Penalty": In some developing contexts, rapid, unplanned urbanization can lead to a "health penalty" where urban dwellers may experience worse health outcomes than their rural counterparts due to poor living conditions, lack of sanitation, and limited access to basic services.
Effects of Urbanization (Broader Implications)
Beyond health service delivery, urbanization has wide-ranging health, social, and psychological effects:
Health Problems Associated with Urbanization:
- Disease Outbreaks: High population density and inadequate sanitation can lead to rapid spread of infectious diseases (e.g., cholera, tuberculosis).
- Alcoholism and Drug Abuse: Stress, anonymity, and easy access can contribute to substance abuse issues.
- STIs and HIV/AIDS: Increased mobility and varied social interactions can contribute to higher rates.
- Accidents: Higher traffic density and industrial activities increase the risk of road and occupational accidents.
- Suicide and Mental Health Issues: Stress, social isolation despite density, competition, and anonymity can contribute to mental health problems.
- Prostitution: Often associated with poverty and social dislocation in urban areas, leading to further health and social risks.
- Water-washed Diseases: Inadequate water supply and sanitation in informal settlements can lead to diseases spread by lack of hygiene.
- Non-communicable Diseases (NCDs): Rise in NCDs due to changes in diet (processed foods), reduced physical activity, and increased stress.
Social Problems Associated with Urbanization:
- Homelessness and Slum Formation: Rapid influx of people can outpace housing development, leading to informal settlements and homelessness, particularly among lower-income groups.
- Class Extremes and Poverty: Urbanization often highlights and exacerbates social inequalities, with visible contrasts between extreme wealth and deep poverty.
- Social Distance and Anonymity: Despite physical proximity, individuals may experience social distance and a lack of close-knit community ties, leading to feelings of alienation.
- Social Heterogeneity: Presence of diverse ethnic, tribal, and cultural groups ("many tribes") can lead to both cultural enrichment and potential social tensions.
- Formal Social Control: Individual behavior is often controlled by formal institutions like the police and courts, rather than informal community norms.
- Social Mobility: Increased opportunities for movement between social classes (upward or downward) and geographical mobility (moving between towns or jobs).
- Voluntary Associations: People have more choice in forming social groups (e.g., social drinking groups, clubs, sports teams) based on shared interests rather than kinship or locality.
- Individuality/Egocentricity: A focus on individual achievement and self-interest ("one for myself or for myself") can emerge due to heterogeneity and competition, sometimes leading to selfishness.
- Lack of Togetherness: Weakening of traditional community bonds and a sense of collective responsibility.
- Moral Laxity: Perceived decline in traditional moral values, sometimes seen in issues like prostitution and adultery, though this is a complex and debated point.
- Dynamism: People are often driven by ambition and readily explore new opportunities that arise.
- Overcrowding and Poor Housing: Leads to various health and social issues, including increased stress, privacy issues, and spread of disease.
- Family Disharmony: Urban dwellers may prioritize jobs over family, and geographical distances can lead to strained relationships.
- Depersonalization: A "don't care" attitude can emerge due to the vastness and anonymity of urban life.
- Deviant Behavior: Overcrowding and social disorganization can contribute to increased rates of deviant behavior.
- Crime and Delinquency: Weakening of social norms and values, coupled with economic disparities and anonymity, can lead to higher crime rates.
Solutions to Urbanization-Related Challenges (Toward Sustainable Urban Health)
Addressing the challenges of urbanization requires comprehensive and multi-sectoral approaches:
- Systematic Development of Urban Centers: Implement planned, integrated urban development strategies to ensure orderly growth, adequate infrastructure, and equitable resource distribution.
- Proper Urban Planning: Develop master plans that include zoning for residential, commercial, and industrial areas, and allocate space for green areas, public services, and healthcare facilities.
- Fighting Poverty: Implement economic policies that create jobs, promote equitable income distribution, and provide social safety nets to reduce urban poverty, which is a root cause of many health and social problems.
- Equal Development for Other Towns (Decentralization): Invest in rural and secondary towns to create opportunities and reduce the pressure of migration to mega-cities, promoting balanced regional development.
- Seek Economical and Social Development Support: Collaborate with government agencies, non-governmental organizations (NGOs), and international development partners to secure funding and expertise for urban development and health initiatives.
- Improving on Housing (Satellite Cities/Affordable Housing): Develop affordable, quality housing options, including the creation of well-planned satellite cities, to alleviate overcrowding and improve living conditions in existing urban centers.
- Encourage Families to Live Together/Strengthen Social Bonds: Implement policies and community programs that support family cohesion and foster strong social networks and community engagement to combat isolation and depersonalization.
- Promote Human Rights: Ensure that urban development and healthcare policies are grounded in human rights principles, guaranteeing equitable access to housing, healthcare, education, and social services for all urban residents, especially vulnerable populations.
- Strengthen Public Health Infrastructure: Invest in sanitation, waste management, clean water supply, and disease surveillance systems to prevent and control urban health threats.
- Sustainable Transportation: Develop efficient and accessible public transportation systems to reduce pollution and improve access to services.
Social Aspects of Diseases and Hospitalization Read More »