Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Table of Contents
ToggleINTEGRATED DISEASE SURVEILLANCE AND RESPONSE-IDSR
IDSR – Is a strategy for a multi-disease surveillance of selected priority diseases or conditions which links the community, health facility, district and national levels allowing the rational use of resources for disease control and prevention.
Integrated Disease Surveillance is a comprehensive approach used by public health systems to monitor, detect, and respond to various diseases and health events in a coordinated manner.
Surveillance – Is the ongoing systematic collection, analysis and interpretation of health data. It includes the timely dissemination and use of information for public health actions.
Surveillance is also used for planning, implementation and evaluation of public health practices at any level
Disease surveillance refers to monitoring of diseases and factors affecting their distribution/trends in order that action may be taken of the health system.
Disease Outbreak: A sudden increase in the number of cases of a particular disease in a defined geographic area and time period that is greater than what is normally expected.
Communicable Diseases: Also known as infectious diseases, these are illnesses caused by microorganisms such as bacteria, viruses, fungi, or parasites that can be transmitted from one person to another, directly or indirectly.
Case Definition: A set of standardized criteria that define what constitutes a confirmed case of a particular disease. It helps health workers accurately identify and classify cases during disease surveillance.
Priority Diseases: Diseases that are given special attention due to their significant impact on public health and the potential for rapid spread and serious consequences. Priority diseases vary by region and context.
Supervision, Monitoring, and Evaluation: These are components of disease surveillance that involve overseeing and assessing the implementation of surveillance systems, tracking data quality and completeness, and evaluating the effectiveness of response strategies.
IDRS works in collaboration with bodies under Center for Disease Control (CDC) in order to achieve the goal of disease surveillance and response.
The outstanding bodies are:
- Division of emergency infectious and surveillance services (DEISS). It provides expertise to design, develop, implement, monitor and evaluate strategies for IDSR. They organize tools for the program like laboratory equipment.
- Division of epidemiology and surveillance capacity building: provides experts for strengthening target countries by giving information on disease outbreaks.
- Global Immunization Division (GID) that provides experts in surveillance for vaccines for preventable disease and integrated data management for an expanded program for immunization related surveillance, routine immunization.
In 1996, there was a big problem with a disease called Ebola. Because of that, Uganda decided to join the IDSR program. They made a CDC to look out for disease outbreaks. Other African countries, like Ethiopia, Ghana, and Burkina Faso, also use IDSR to handle outbreaks.
Objectives of Integrated Disease Surveillance and Response
- To strengthen national capacity for early detection, complete recording, timely reporting, use of electronic tools, regular analysis and prompt feedback of IDSR priority diseases, events and conditions at all levels.
- To strengthen national and subnational laboratory capacity to confirm IDSR priority diseases, events and conditions.
- To strengthen capacity for public health emergency preparedness and response at all levels.
- To strengthen the supervision, monitoring and evaluation system for IDSR.
- To integrate multiple surveillance systems so that tools, personnel and resources are used more efficiently.
- Emphasize community participation in detection, reporting and response to public health events including case-based and event-based surveillance and response and risk communication in line with International Health Regulations (IHR).
According to WHO AFRO 1998, the objectives for IDSR include:
- To strengthen district level surveillance.
- To integrate the laboratory with laboratory reports.
- To reduce duplication of reporting on the outbreak.
- To share resources among disease control programs.
- To translate surveillance and laboratory data into specific and timely public health actions.
Basic Ingredient for IDSR
The IDSR also identified basic ingredients for it to achieve the goals as follows: To make IDSR work well, we need a few important things:
- Clear case definition and reporting mechanism.
- Efficient communication systems.
- Basic but sound epidemiological framework.
- Good laboratory report.
- Good feedback and rapid response.
- Nurses/Midwives attached to health centres to document the surveillance reports.
Core functions of IDSR
Step 1 – Identify and record cases, conditions and events: Use of standard case definitions for health service delivery points (human, animal and environment), simplified case definitions for community level, to identify priority diseases, conditions, and alerts that can signal emerging public health
Step 2 – Report suspected cases or conditions or events to the next level for action: If this is an epidemic prone disease or a potential Public Health Emergency of International Concern (PHEIC), or a disease targeted for elimination or eradication, report immediately to the next level
Step 3 – Analyze (person, place and time) data and interpret findings: Surveillance data should be compiled, analyzed for trends, compared with data from previous periods and interpreted for public health actions at all levels
Step 4 – Investigate and confirm suspected cases, outbreaks or events: Take action to ensure that the cases, outbreaks or events are investigated and confirmed by laboratory
Step 5 – Prepare: ensure the availability of public health emergency preparedness and response plans, as well as a mechanism for coordination of response measures. Take steps in advance of occurrence of outbreaks or public health events, to prepare teams that may respond quickly and set aside essential supplies and equipment which will be available for immediate action
Step 6 – Respond: On confirmation of the outbreak, coordinate and mobilize resources (human, financial etc.) to implement the appropriate public health response
Step 7 – Risk communication: Risk communication is the real-time exchange of information, advice and opinions between experts, community leaders, or officials and the people who are at risk. It encourages communicating with all levels and across sectors including communities that provide data, report outbreaks, cases and events
Step 8 – Monitor, evaluate, supervise and provide feedback to improve the surveillance system: Assess the effectiveness of the surveillance and response systems, in terms of timeliness, quality of information, preparedness, and overall performance. Provide feedback to reinforce health workers’ efforts to participate in the surveillance system. Take action to correct problems and make improvements
Detecting and Planning for Disease Outbreak
From the previous section where we introduced Integrated Disease Surveillance and Response (IDSR), you learned that the main group responsible for controlling diseases is the people who work in the Center for Disease Control (CDC), which is usually located in a hospital setting.
You also learned about the important members of the team needed to make the work effective, including midwives like yourself who are stationed at the outskirts of the district. With the help of clear case definitions, you can accurately detect diseases and provide detailed reports to the CDC.
In the earlier part of our community health discussions, you learned how to carry out health assessments to identify health issues within the community and diagnose priority diseases. You also understood that in order to reach a diagnosis for a community health problem, you have to perform surveillance. This involves screening through laboratory tests and actively searching for cases.
Similarly, when you’re dealing with infectious diseases, you will follow similar guidelines. You’ll select and conduct surveillance activities to gather information, analyze it, interpret the findings, and create a report for the CDC to take action.
To carry out these activities effectively, you need to organize your team, which will consist of:
- District Health Officer: This is an important leader who oversees health activities in the district.
- Community Health Workers: These are the frontline workers who engage directly with the community and gather information.
- Laboratory Technician: This person handles lab tests and analysis, which is crucial for confirming diseases.
- Subordinate Nurses: You’ll work with at least one nurse who assists you in carrying out various tasks.
Together, this team will collaborate and follow the outlined guidelines until the final step of report writing. This coordinated effort ensures timely and accurate response to disease outbreaks and contributes to safeguarding public health.
Approaches to public health surveillance
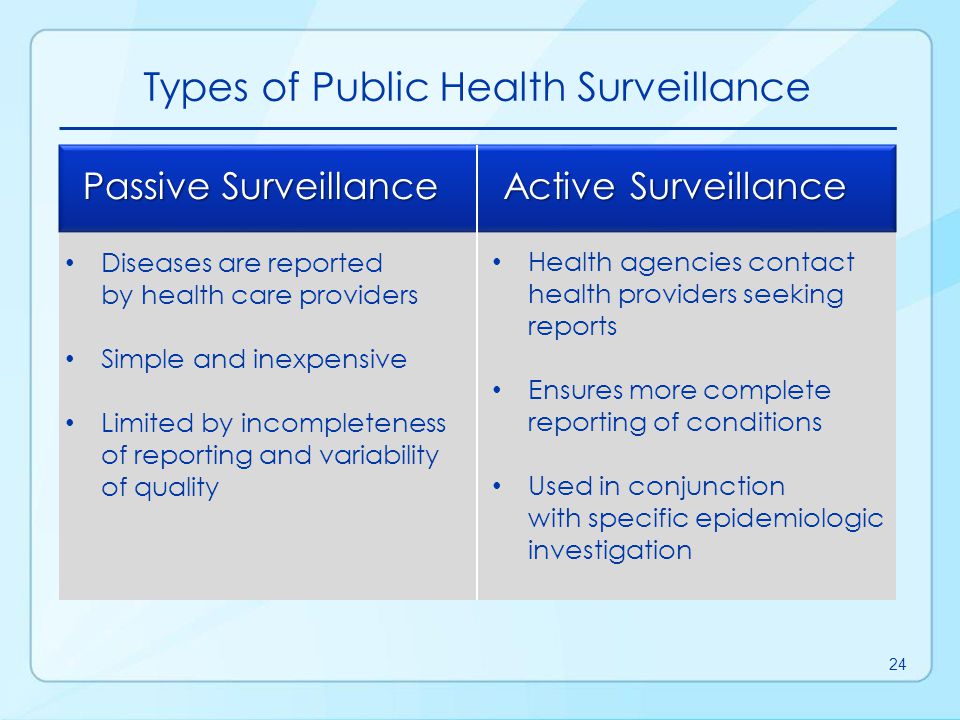
A. Passive surveillance: a system by which a health institution receives routine reports submitted from health facilities and the community. This is the most common, and it includes the surveillance of diseases and other public health events through the Health Management Information System (HMIS)
B. Active surveillance: It involves actively looking for the cases in the community or health facilities through;
- Records review by health workers at health facility level
- Screening for specific health conditions e.g., at points of entry, health facilities etc.
- Regular communication and keeping in touch with key reporting sources. This may take various forms such as telephone calls to health care workers at a facility or laboratory or physically moving to the site.
- Finding additional cases and contacts during outbreaks.
- Finding diseases targeted for elimination and eradication e.g., Polio (through Acute Flaccid Paralysis (AFP) surveillance), Guinea Worm etc.
C. Integrated Disease Surveillance: This approach aims at collecting health data for multiple diseases using standardized tools, and supports Early Warning Alert and Response (EWAR) systems. To ensure robust early warning and prompt response, the IDSR data collection and analysis system relies on two main channels of information or signal generation, namely:
- Indicator Based Surveillance (IBS)
- Event-Based Surveillance (EBS).
Indicator-based surveillance (IBS)
Indicator-based surveillance is the regular, systematic, identification, collection, monitoring, analysis and interpretation of structured data, such as indicators produced by a number of well identified, mostly health-based formal sources. Methods of indicator-based surveillance include; facility-based surveillance, case-based surveillance, sentinel surveillance, syndromic surveillance, laboratory-based surveillance, disease-specific surveillance and community based surveillance
Event- based surveillance (EBS)
Event-based surveillance is rapid capture of information about events that are of potential risk to public health. Information is initially captured as a rumor or signal with the potential of becoming an alert after verification. All alerts may not necessarily become real events, as such they all need to be triaged and verified before a response is initiated.
Detecting and Planning for Disease Outbreak
From the previous section where we introduced Integrated Disease Surveillance and Response (IDSR), you learned that the main group responsible for controlling diseases is the people who work in the Center for Disease Control (CDC), which is usually located in a hospital setting.
You also learned about the important members of the team needed to make the work effective, including midwives like yourself who are stationed at the outskirts of the district. With the help of clear case definitions, you can accurately detect diseases and provide detailed reports to the CDC.
In the earlier part of our community health discussions, you learned how to carry out health assessments to identify health issues within the community and diagnose priority diseases. You also understood that in order to reach a diagnosis for a community health problem, you have to perform surveillance. This involves screening through laboratory tests and actively searching for cases.
Similarly, when you’re dealing with infectious diseases, you will follow similar guidelines. You’ll select and conduct surveillance activities to gather information, analyze it, interpret the findings, and create a report for the CDC to take action.
To carry out these activities effectively, you need to organize your team, which will consist of:
- District Health Officer: This is an important leader who oversees health activities in the district.
- Community Health Workers: These are the frontline workers who engage directly with the community and gather information.
- Laboratory Technician: This person handles lab tests and analysis, which is crucial for confirming diseases.
- Subordinate Nurses: You’ll work with at least one nurse who assists you in carrying out various tasks.
Together, this team will collaborate and follow the outlined guidelines until the final step of report writing. This coordinated effort ensures timely and accurate response to disease outbreaks and contributes to safeguarding public health.
Priority diseases, conditions or events
Epidemic prone disease, conditions or events | Diseases targeted for eradication or elimination | Other major disease, events or conditions of public health importance |
─ Acute hemorrhagic fever syndrome* ─ Anthrax ─ Chikungunya ─ Cholera ─ Dengue ─ Diarrhea with blood (Shigella) ─ Listeriosis ─ Malaria ─ Meningococcal meningitis ─ Monkeypox ─ Plague ─ SARI** ─ Typhoid fever ─ Yellow fever ─ Zika ─ Also; ─ A cluster of deaths in the community (animal or human deaths) ─ A cluster of unwell people or animals with similar signs or symptoms ─ *Ebola, Marburg, Rift Valley, Lassa, Crimean Congo, West Nile Fever, Dengue. | ─ Trachoma ─ Yaws and endemic syphilis or bejel ─ Poliomyelitis
Diseases or events of international concern ─ Human influenza due to a new subtype1 ─ SARS1 ─ Smallpox1 ─ Zika ─ Yellow fever ─ Any public health event of international or national concern (infectious, zoonotic, food borne, chemical, radio nuclear, or due to unknown conditions. | ─ Acute viral hepatitis ─ Adverse events following Immunization (AEFI) ─ Diabetes mellitus (new cases) ─ Diarrhea with dehydration less than 5 years of age ─ HIV (new cases) ─ Hypertension (new cases) ─ Injuries (Road traffic Accidents) ─ Malaria ─ Malnutrition in children under 5 years of age ─ Maternal deaths ─ Perinatal deaths ─ Epilepsy ─ Human Rabies ─ Severe pneumonia less than 5 years of age ─ STIs ─ Schistosomiasis ─ Soil transmitted helminths ─ Trachoma |
DETECTING AND REPORTING OF PRIORITY DISEASES, CONDITIONS/EVENTS
An essential component of a public health surveillance system is its ability to detect priority diseases which fall within the mandate of public health officials at all levels. Early detection, reporting and response of public health events help to reduce the burden of mortality and morbidity.
Detection of suspected cases of outbreak prone diseases always be vigilant in your health facility and community for the following;
- Targeted outbreak prone diseases, conditions and events.
- Conditions that are reported more frequently than expected in the community.
- Cluster (group) of diseases or sudden deaths following public gatherings.
- Any unusual events that may cause health risks.
Health staff (human, animals and environmental) conduct surveillance activities at all levels of the health system (public and private) so that they can detect public health problems of concerns in their community.
In Community.
- Community Case definition for all priority diseases plays important roles in surveillance by facilitating early detection and action to priority diseases, conditions and events.
- Community members should be oriented in surveillance so that they actively participate in detecting, reporting, responding to and monitoring health events related to humans or animals in their catchment areas.
- Encourage vigilance in ensuring that these events are identified and reported on time to facilitate early and quick response.
Ways of detecting priority diseases, conditions and events.
- A person falls ill and seeks treatment from a facility.
- High rate of hospital admission for the same disease or symptoms.
- Community members report unusual events or occurrences at local level such as clusters of deaths or unusual disease patterns to the health facility or perhaps school.
- Health workers who conducted routine record reviews to find cases for a specific disease observe that cases of another priority disease have not been reported e.g. AFP, cholera, measles.
- During conducting routine record reviews of lab register and observe recorded continued cases of priority diseases e.g. yellow fever, cholera.
- Radio/T.V, newspapers or social media report a rumor of rare or unexplained events in the area with potential exposure for humans.
- Vital events records show an increase in maternal deaths.
- Unusual reports of illness among health care workers.
- An unusual death or number of deaths among animals, such as livestock, birds or rodent species, or an unusually high number of sick animals presenting with the same signs.
- Environmental officers observed during assessment of water bodies contamination which might be due to chemicals like lead or due to other related chemicals due to mining activities.
A STANDARD CASE DEFINITION
Case definition is an agreed-upon set of criteria used to decide if a person has a particular suspected disease or condition. The definition specifies clinical criteria, laboratory diagnosis and specifications on time, place and person.
A case definition of a disease is a standardized set of criteria that outlines the specific characteristics and symptoms that an individual must meet in order to be classified as having that particular disease.
It serves as a clear guideline for healthcare professionals and public health authorities to accurately identify and classify cases of the disease.
In simpler terms, a case definition is like a checklist that helps healthcare workers determine whether a person’s symptoms and characteristics match those of a specific disease. If they meet the criteria in the checklist, they can be considered a “case” of that disease. This is important for accurate disease tracking, monitoring, and response.
Disease | Clinical Presentation |
Measles | – High fever that gets serious quickly- Rash appears 3 to 5 days after fever, followed by Koplik’s rash around the mouth and forehead 2 to 4 days after infection. |
Tetanus | – Symptoms show up around 5 to 10 days after infection,- Common symptoms include jaw stiffness, restlessness, difficulty swallowing, headache, fever,- Other symptoms: sore throat, neck stiffness, abdominal rigidity, raised eyebrow. |
Poliomyelitis | – Symptoms start 3 to 5 days after infection,- Early symptoms: slight headache, sore throat, vomiting in younger children,- Older children: symptoms appear 7 to 14 days,- Major symptoms: fever, severe headache, stiff neck and back, deep muscle pain, brain damage leading to paralysis of certain muscles. |
Tuberculosis | – Patient may appear well or have a cough,- Cough might produce green or yellow sputum in the morning,- Night sweats and shortness of breath,- Pneumothorax (air in pleural space) in young adults,- Weight loss. |
Cholera | – Symptoms begin 1 to 3 days after infection,- Range from mild, uncomplicated diarrhea to severe,- Common symptoms: sudden, painless watery diarrhea and vomiting,- Severe cases: loss of more than 1/4 of fluid an hour, eye sickness, intense thirst, muscle cramps, weakness, minimal urine. |
Hepatitis | – Acute viral form: sudden onset with poor appetite, feeling ill, nausea, vomiting, and often fever,- Person develops joint pains with itchy red hives on the skin,- Dark urine, jaundice (yellowing of skin and eyes) with general itching, liver enlargement. |
Why do we need case definitions?
- To help decide if a person has a presumed disease or condition or event, or to exclude other potential disease diagnoses.
- To ensure that every case is diagnosed in the same way, regardless of where or when it occurred, or who identified it.
- To initiate action for reporting and investigation quickly if the clinical diagnosis takes longer to confirm.
- To compare the number of cases of the diseases, conditions or events that occurred in one time or place with the number occurring in another time or place
Standard Case Definitions, for health facility level.
Three-tiered classification system is normally used – Suspect, Probable, Confirmed:
A Suspected case: indicative clinical picture i.e., patient will have fewer or atypical clinical features without being a confirmed or a probable case
Probable case: Clear clinical picture (meets the clinical case definition) i.e., patient will have typical clinical features of the illness or linked epidemiologically to a confirmed case but a laboratory sample cannot be taken because the case is lost or dead or a sample has been taken but not available for laboratory testing or was not viable for sufficient laboratory testing
Confirmed case: A suspected or confirmed case verified by laboratory analysis.
Priority Diseases in Uganda and their Case Definition
Activity:
1. Write down the most common priority diseases that you have ever participated in managing.
- Measles
- Tuberculosis
- Poliomyelitis
- Tetanus
- Cholera
- Hepatitis B
2. Outline the case definition of the diseases.
- Measles: A fever accompanied by a rash, cough, and red, watery eyes.
- Tuberculosis: Persistent cough for more than two weeks, chest pain, and weight loss.
- Poliomyelitis: Muscle weakness or paralysis, often affecting the legs.
- Tetanus: Muscle stiffness and spasms, usually starting with the jaw muscles.
- Cholera: Profuse watery diarrhea and vomiting, leading to dehydration.
- Hepatitis B: Jaundice, fatigue, abdominal pain, and dark urine.
As a quick reminder, priority diseases are communicable diseases caused by biological agents or their products.
They spread from one person to another and are called priority diseases because of their serious impact on humans. Many of these diseases can lead to disasters, increase illness and death, and even cause economic problems for a country.
In Uganda, there have been several outbreaks of diseases that have resulted in loss of lives. Some of these diseases include:
- Measles: Common among children aged 1 to 3 years. Symptoms include rash, cough, and red, watery eyes.
- Tuberculosis: Affects people of all age groups and is characterized by a persistent cough, chest pain, and weight loss.
- Poliomyelitis: Recent research shows an increasing trend in this disease, which causes muscle weakness or paralysis, often in the legs.
- Tetanus: Affects people of all ages, usually starting with stiffness and spasms in the jaw muscles.
- Cholera: Common during rainy seasons and can become a disaster. Symptoms include severe watery diarrhea and vomiting, leading to dehydration.
- Hepatitis B: Rampant throughout the country, presenting symptoms like jaundice, fatigue, abdominal pain, and dark urine.
REPORTING SUSPECTED CASES OF PRIORITY DISEASE/EVENTS.
Rationale for Reporting Include;
- To identify emerging problems or conditions and plan appropriate responses including informing relevant staff or levels.
- Take action in a timely way.
- Monitor disease trends in the area.
- Evaluate the effectiveness of the response
In IDSR, data collection and data reporting follow different timelines for different purposes.
i. Immediate reportable diseases, conditions and events
- Report case based information to next level
- Notifying a potential public health emergency of international concern under IHR 2005
- Reporting events from the community sources
ii. Summarize immediate and Weekly reportable diseases.
- Weekly reporting of immediate notifiable diseases
- Zero reporting
iii. Monthly /quarterly reporting.
- Report monthly and quarterly routine summary information for other diseases of public health importance
iv. Improve routine reporting practices
- Review the flow of information at the reporting site
- Keeping records and procedures for managing reporting forms
- Perform periodic checks on data quality
- Enhance linkages to strengthen community based surveillance
- Strengthen linkages between laboratory and surveillance information
- Promote a Multisectoral one health approach with effective involvement from human, animal and environmental health sectors as well as other relevant sectors to strengthen reporting.
v. Data protection and security to protect patient’s confidentiality and privacy by using unique numbers instead of names and this will prevent identities
1) Record details of the sick person including;
- The name of the sick person.
- Sex, age and job of the sick person.
- Address and location of the household.
- The signs of the disease.
- The date of the onset.
- How many people are affected in the household?
- The action taken.
- Any previous contacts as necessary.
2) Report immediately to the local area leaders, nearest health facility in the community and the health sub district, DHO or surveillance team and MOH using phone calls, SMS, Android and web.
3) Create a line list for the cases seen in the facility.
ANALYZING/INTERPRETATION OF DATA IN PRIORITY DISEASES
- Data is a set of values of subjects with respect to qualitative or quantitative variables. OR;
- Data is information that has been translated into a form that is efficient for movement or processing.
- Analysis refers to breaking a whole into its separate component for individual examination of raw data and converting it into information useful for decision-making by users.
- Data analysis is the process of inspecting, cleansing, transforming and modeling data with the goal of discovering useful information, informing conclusions and supporting decision making.
Analyzing data provides the information that is used to take relevant, timely and appropriate public health action.
Analyzing a surveillance data allows for;
- Observing trends over time and alerting health staff about emergent events or unusual patterns.
- Identifying geographic areas of higher risk.
- Characterizing personal variables such as age, gender or occupation that a person is at higher risk for the disease or event.
- Monitoring and evaluation of public health interventions
1. RECEIVE, HANDLE AND STORE DATA FROM REPORTING SITES
a) Receive data
- Make a careful record of all data received from the reporting site.
- The surveillance team at each level or reporting site where data are received should;
- Acknowledge the recipient of the data/report
- Log into an appropriate logbook any data set or surveillance report received for any reporting site.
- Record with log the data, they were received, what is the report about and who is the sender.
- Verify whether the data send arrived timely or was late
- Check the completeness of the data set or reports
- Review the data quantity:
- Verify whether the information (hard copy or electronic file) is filled out accurately
- Ensure that the form is filled out completely
- Check to be sure that there are no discrepancies on the form
- Merge the data then store in database
- For electronic surveillance refer to eIDSR guide
b) Enter and clear the data
- Extract the priority IDSR diseases from the register and enter correctly into aggregated IDSR reporting forms while listing data from all the reporting sites through liaison with health information assistants (HIAs).
- Ensure that health facility personnel know the algorithm for reporting including reporting levels.
Use the following practices regardless of the method
2. Analyze data by time, place and person
Objective | Method | Data display tools | |
Time | To detect abrupt or long-term changes in disease or unusual event occurrence, how many occurred, the seasonality and the period of time from exposure to onset of symptoms | Compare the number of case reports received for the current period with the number of cases received in a previous period (days, weeks, months, quarters, seasons or years | Record summary total in a; ∙ Table ∙ Line graph ∙ Histogram ∙ Sequential maps |
Place | To identify where cases are occurring | Plot cases on a map and look for clusters or relationships between the location of the cases and the health events being investigated, e.g cases near a river, near a market or near a slum | Plot cases on a spot map of the district or area affected during an outbreak Dot density analysis can also be used to depict the number of cases by geographical location |
Person | To describe reasons for changes in disease occurrence, how it occurred, who is at greatest risk for disease and potential risk factors | Depending on the disease, characterize cases according to the data reported for case based surveillance such as age, sex, place of work, immunization status, school attendance and other known risk factors for the diseases | Extract specific data about the population affected and summarize in a ∙ Table or ∙ Bar chart |
- Analyze data by time
- Analyze data by place
- Analyze data by person
- Make a table for person analysis
- Calculate the percentage of cases occurring with a given age group
- Calculate the attack rates
- Calculate a case fatality rate
3. Compare analysis results with thresholds for public health action
- An alert threshold– Is the critical number of cases (or indicator, proportion, rate etc) that is used to sound an investigation at the start of an epidemic and prepare to respond to the epidemic.
- Action( Epidemic) threshold– Is the critical number or density of susceptible hosts required for an epidemic to occur.
4. Draw conclusions from the findings to generate information through;
- Routinely gather or present the graphs, maps and tables and meet with district health teams or relevant stakeholders to review analysis results and discuss the findings.
- Systematically review the findings following the district’s analysis plan if one has been prepared.
- Make sure you also correlate the analysis you have done with other data sources like from animals, or the environment to assist in correct interpretation of the findings.
- Consider quality of the data when interpreting results.
- At minimum, review the findings to;
∙ Assess
∙ Compare
∙ Consider possible explanation for increase in cases
∙ Changes in reporting of cases
∙ Changes in reporting procedures
∙ Changes in case definition that is being used to report
- Summarize and use the analysis to improve public health action.
- Prepare and share with all the stakeholders including the affected communities
INVESTIGATION AND CONFIRMATION OF SUSPECTED CASES, OUTBREAKS/EVENTS:
Purposes
- Verify the outbreak or confirm the public health event and risk.
- Identify and treat additional cases that have not been reported or recognised
- Collect information and laboratory specimens for confirming the diagnosis ∙ Identify the source of infection or cause of the outbreak.
- Helps to describe the epidemiological situation in time, place and person.
- Describes how the disease is transmitted and the population at higher risk ∙ Select appropriate response activities to control the outbreak or the public health event.
- Strengthen prevention activities to avoid future reoccurrence of the outbreak
Steps of outbreak investigation
1. Prepare to conduct an investigation. Mobilize Public health emergency rapid response team (PHERRT)
- Specify tasks of the people in the PHERRT what they are expected to perform
- Define supervision and communication lines
- Decide where the investigation will take place
- Obtain the required authorizations
- Finalize forms and methods for collecting information and specimens
- Arrange transportation and other logistics
- Gather supplies for collecting laboratory specimens
2. Verify and confirm the outbreak/event
- Review the clinical history and epidemiology
- Collect laboratory specimens and
- Obtain laboratory results to confirm the diagnosis
3. Define and search for additional cases;
- Develop a case definition to be used
- Isolate and treat cases as necessary
- Search for additional cases through; Search for suspected cases and deaths in the health facility records and Search for contact persons and suspected deaths in the community (contact tracing)
4. Develop a line list and record information about the additional cases
5. Analyze data about the outbreak; Interpret analysis results;
- Interpret the time analysis results
- Interpret the person analysis results
- Interpret the place analysis results
- Analyze data and generate hypothesis
- Test and refine hypothesis with analytic study
6. Report writing and dissemination of findings.
7. Implement prevention and control measures.
8. Conduct an assessment to determine if the event is a potential public health emergency of international concern (PHEIC).
9. Maintain and intensify surveillance.
10. Conducting regular risk assessment after the outbreak has been confirmed.
RESPONDING TO OUTBREAKS AND OTHER PUBLIC HEALTH EVENTS
Preparation: Preparations for public health events involves the following;
1. Establish a permanent PHEOC (command and control Centre) for overseeing public health emergency preparedness and response activities. The PHEOC will need to develop the following essential elements so as to be fully functional to support the preparation and response to emergencies.
- Plans and procedures for operations
- Telecommunication technology and infrastructure to enable timely communication
- Information system to support informed decision making (Hms/DHI3).
- Trained human resources
2. Establish a district or regional public health emergency management committee (PHEMC)
- Identify members of the PHEMC
- Identify functions of the PHEMC
- Regular PHEMC meetings.
3. Establish public health emergency management committee at all level These includes;
Coordination/management subcommittees.
Roles: Coordinate all aspects of the operations response, planning and management including:
- Selecting participating organizations and assigning responsibilities
- Designing, implementing and evaluating control interventions
- Coordination of technical EPR subcommittees and overall liaison with partners
- Daily communication through situation report about the evolution of the outbreak
- Managing information for public and news media
- Operational support including mobilization of resources
- Responsible for staff wellbeing, security
Finance and administration
- Tracks expenditure, makes payments, and provides administrative services
- Ensures appropriate cash flow management, tracking material and human resources, looking at cost, budget preparation, monitoring, and maintenance of administrative records.
Logistics committee
- Provide budgetary support/ funding for epidemic preparedness & response.
- Procurement of equipment and supplies.
- Maintain adequate stocks of supplies and equipment.
- Arrange for transport and communication systems.
- Liaison with other agencies for logistic support.
- Provide accountability for all the resources used during epidemic preparedness & response.
Planning committee
- Evaluate the situation (information gathering and analysis), assessment of the options for dealing with it, and keeping track of resources.
Case management and infection prevention and control committee
- Ensure or make available guidelines and SOPs for case management and infection prevention and control in all health facilities.
- Strengthen isolation facilities and reinforce infection prevention and control measures.
- Conduct risk assessment of health care workers.
- Ensure appropriate medical care is being provided to patients.
- Provide ambulance services – collection of suspected cases from the community using the defined referral system.
- Collect data from all treatment facilities (if available) and submit to the surveillance sub committee.
- Ensure appropriate disinfection of homes and environments with suspected/ probable/ confirmed cases/ deaths of an infectious disease.
- Conduct safe burial of dead bodies from isolation facilities and community deaths.
- Training and refreshers training of health workers in the isolation facility and other health facilities in the affected district
Surveillance and laboratory
- Ensure or make available all surveillance guidelines and tools in the health facilities.
- Ensure the use of the outbreak case definition.
- Conduct active case finding, case investigation, contact tracing and follow-up.
- Verification of suspected cases/ alerts/ rumors in the community.
- Ensure proper filing of case investigation, contact tracing and follow-up forms.
- Ensure proper collection, packaging, transport, and testing of specimens from suspect/ probable cases/ deaths.
- Communicate test results to clinical services.
- Conduct data management and provide regular epidemiological analysis and reports.
- Training of health personnel in disease surveillance.
- Close linkage with burial, infection control and social mobilization groups
Risk communication and social mobilization
- Ensure or make available risk communications materials and plans
- Conduct rapid assessment to establish community knowledge, attitudes, practices & behavior on prevailing public health risks/events
- Organize sensitization and mobilization of the communities
- Serve as focal point for information to be released to the press and public
- Liaise with the different subcommittees, local leadership and NGOs involved in activities on mobilizing communities
Psychosocial support committee
- Provide psychological and social support to suspected/probable/confirmed cases; affected families and communities
- Provide wellness care and psychological support to the response team
- Prepare bereaved families/ communities for burials
- Prepare communities for reintegration of convalescent cases/ patients who have recovered
Water sanitation and hygiene- WASH committee
- Conduct environmental health risk assessment for the outbreak
- Ensure provision of clean water
- Improved water management at household and community level.
- Plan for sanitation improvement campaign
- Plan for improved hygiene practices including hand-washing, food hygiene and sanitation.
Vaccination campaign committee/EPI team
- Identify high risk groups during the outbreak that should be targeted for vaccination
- Compute the targeted population for the vaccination campaign
- Conduct micro-planning for all vaccination logistics including cold chain facilities, vaccine delivery and distribution, human resource needs, waste handling, social mob.
- Conduct the vaccination campaign and post vaccination campaign validation exercise
Establish public health emergency rapid response team (PHERRT)
Roles of PHERRT includes;
- Investigate rumors and reported outbreaks, verify diagnosis and other public health emergencies including laboratory testing
- Collect additional samples from new patients and old ones if necessary (human, animals, food, and water
- Make a follow up by visiting and interviewing exposed individuals, establish a case definition and work with community to find additional cases
- Assist in laying out mechanisms for implementation of Infection Preventive Control Measures
- Assist in generating a line list of the cases, and perform descriptive analysis of data (Person, Place and Time) to generate hypothesis including planning for a further analytical study
- Propose appropriate strategies and control measures including risk communications activities
- Establish appropriate and coordinated risk communication system through a trained spokesperson
- Coordinate rapid response actions with national and local authorities, partners and other agencies.
- Initiate the implementation of the proposed control measures including capacity building
- Conduct ongoing monitoring and evaluation of effectiveness of control measures through continuous epidemiological analysis of the event
- Conduct Risk Assessments to determine if the outbreak is a potential PHEIC
- Prepare detailed investigation reports to share with PHEMC committee
- Contribute to ongoing preparedness assessments and the final evaluation of any outbreak response.
- Meet daily during outbreaks, and quarterly when there is no outbreak
- Participate in simulation exercises
4. Risk mapping for outbreaks and other public health events.
- Risk assessment and mapping is used as an aid to preparedness to identify at-risk areas or populations, rank preparedness activities, and also to engage key policy and operational partners.
5. Resource mapping to identify the available resources in every geographical area to ensure prompt mobilization and distribution of such resources including materials, human and funds in an outbreak situation
6. Prepare an emergency preparedness and response plan to strengthen the ability of the national to subnational levels to respond promptly when an outbreak/event is detected. This plan should; Response to outbreaks/events
- Declaring an outbreak and activating the response structures- once an epidemic threshold is reached at district level the head of DHMT should notify the region and MOH will assess whether the event is potential public health event of international concerns.
- Mobile PHERRT for immediate action which includes;- convene the district public health management once an outbreak/event is confirmed, DHMT will work with the district authority to convene PHEMC to assess and implement the response.
- Select and implement appropriate public health response activities. These includes;
- Strengthen case management and infection prevent and control measures (IPC)
- Build the capacity for response staff
- Enhance surveillance during the response
- Enhance surveillance with neighboring boarder districts
- Engage community during response
- Inform and educate the community
- Conduct a mass vaccination campaign if indicated
- Improve access to clean and safe water
- Ensure safe disposal of infectious waste
- Improve food handling practices
- Reduce exposure to infectious or environmental hazards
- Ensure safe and dignified burial and handling of dead bodies
- Ensure appropriate and adequate logistics and supplies
7. Provide regular situation reports on the outbreak and events
8. Document the response including minutes of meeting, activity, process, epidemic report, evaluation reports and other relevant document
9. Treatment of cases during an outbreak with appropriate medicine and procedures. These may include;
- Antibiotics
- Rehydration with fluids orally or intravenously
- Assessment of pain and management
- Ensure appropriate infection control
- Observation- vitals and specific observation
- Other routine nursing care
The Different Levels Where Surveillance Activities Are Performed
- Community: Represented by basic community-level services such as VHTs, village leaders (religious, political, traditional), school teachers, extension workers, veterinarians, chemical and drug sellers, and traditional healers.
- Health facility: For surveillance purposes, all institutions (public and private health services providers) with outpatient and/or in-patient facilities are defined as a “health facility.”
- Health Sub-district (HSD): The HSD is the basic level for delivery of the Uganda National Minimum Health Care Package. It is mandated with planning, organization, budgeting, supervision, and management of health services at this and lower-level health centres. It carries an oversight function of health care services within the HSD with a referral facility at the level of a general hospital or HC IV. For surveillance purposes, the HSD receives and reviews reports from lower-level health facilities in its catchment area and submits aggregated reports to the district.
- District: The District Health Services have the responsibility of planning and directing implementation, supervision, and monitoring of integrated service delivery in the context of the One Health approach.
- Regional Level: It consists of regional referral hospitals (RRH), which provide referral services, support supervision, and response to public health threats to the districts within their respective regions.
- National level: The national health system consists of the Ministry of Health and other national-level institutions, including national referral hospitals, national reference laboratories, and national medical stores. It is where policies, guidelines, and standard operating procedures are developed and resources allocated. In relation to surveillance, this level reports on priority diseases and uses the IHR decision instrument.
Roles and Responsibilities of Various Actors in IDSR
Community-Based Surveillance Focal Person (Community Health Worker)
- Using lay simplified case definitions to identify priority diseases, events, conditions, or other hazards in the community.
- Conducting household visits on a regular basis.
- Meeting with key informants on a regular basis.
- Attending local ceremonies and events and following up on anything unusual, e.g., someone you were expecting to be there doesn’t show up.
- Recording priority diseases, conditions, or unusual health events in the reporting forms and tools (tally sheets) and reporting immediately within 24 hours.
- Participating in verbal autopsies by performing interview questions prepared by the supervisor at the health facility.
- Sending rapid notification to the nearest health facility and other relevant sectors of the occurrence of unexpected or unusual cases of disease or death in humans and animals for immediate verification and investigation according to the International Health Regulations (IHR) and in line with the IDSR strategy (within 24 hours).
- Involving local leaders in describing disease events and trends in the community.
- Sensitizing the community to report and seek care for priority diseases, conditions, and unusual events.
- Supporting health workers during case or outbreak investigation and contact tracing.
- Mobilizing local authorities and community members to support response activities.
- Participating in risk mapping of potential hazards and in training, including simulation exercises.
- Participating in containment and response activities in coordination with the district level.
- Participating in response activities, which could include home-based care, social or behaviour change of traditional practices, and logistics for distribution of drugs, vaccines, or other supplies. Providing trusted health education in a crisis is a useful contribution.
- Giving feedback to community members about reported cases, events, and prevention activities.
- Verifying if public health interventions took place as planned with the involvement of the community.
- Participating in meetings organized by sub-district, district, and higher-level authorities.
Health Facility Staff and Point of Entry
- Identifying cases of priority diseases using the standard case definitions.
- Recording case-based information and reporting for immediately notifiable diseases, conditions, and events to the next level.
- Liaising with the district on how to conduct immediate laboratory investigation of suspected cases.
- Case treatment/ referral.
- Preparing for and participating in outbreak investigation and response and case treatment.
- Reporting summary data and case-based (weekly report) to the next level timely.
- Conducting simple data analysis (graphs, tables, charts) at the point of collection.
- Communicating diagnosis for outbreak-prone diseases to the district/ community.
- Convening the district rapid response team.
- Identifying resources (human, financial, commodities, phone cards) and timeline for deployment.
District Surveillance Officer at District Level:
- Investigate and verify possible outbreaks, collect diagnostic samples, and advise on treatment/prevention protocols.
- Prepare and analyze weekly surveillance reports and submit them to higher authorities in a timely manner.
- Ensure that surveillance sites maintain surveillance reports and ledgers/logbooks appropriately.
- Maintain a list of all reporting sites.
- Establish and maintain a database of all trained and registered healthcare workers who can serve as surveillance focal persons at the reporting sites as well as other CBS FPs.
- Ensure there is an adequate supply of data collection and reporting tools available at the surveillance reporting sites.
- Ensure that the IDSR standard case definitions for all the priority diseases are understood and used by healthcare workers at the site, and provide on-the-spot training if needed.
- Monitor the performance indicators (such as timeliness and completeness) of the IDSR as stipulated in the IDSR guideline.
- Periodically update graphs, tables, charts, etc. and compare current data with previous months, quarters, weeks, or years (important for seasonal events) and make recommendations for response.
- Provide in-person feedback to surveillance reporting sites on a weekly or monthly basis regarding the implementation of the IDSR.
- Closely follow up (through calling) with the reporting sites to ensure they report data on time.
- Conduct regular supportive supervision visits to surveillance sites, including health facilities, border entries, and communities, and build their capacity to analyze and interpret their data to guide decisions. Sign and date the inpatient and outpatient record books, registries, or phone entries to document the visit and write recommendations for improvement.
- Support healthcare facilities to verify alerts from the community.
- Arrange and lead the investigation of verified cases or outbreaks.
- Maintain an updated line list of suspected cases.
- Assist healthcare facilities in the safe collection, packaging, storage, and transport of laboratory specimens for confirmatory testing.
- Receive laboratory results from the Province/Region and provide them to the healthcare facility.
- Conduct/coordinate on-the-job trainings for the surveillance sites with new staff.
- Review the quality of surveillance data from time to time by conducting data quality audits and develop appropriate measures to improve data quality in the district.
- Maintain a rumor logbook to record events for the surveillance site.
- Ensure cross-border (district-district) coordination and collaboration on surveillance issues and provide notification of any outbreaks in the neighboring district. International or cross-border notification should also be done if needed.
- Document the value added of IDSR and advocate to the health management team to support IDSR activities.
- Participate in outbreak investigations and ensure there is an updated register/line list.
The District Health Management Team:
- Through the District Medical Officer, liaise with the District Executive Director/District Commissioner/Regional Medical Officer on overall surveillance activities and plans.
- Support the Surveillance Officer at the district level to implement planned activities.
- Ensure surveillance activities are included in the District Health Planning of overall activities.
- Liaise with the District officials to mobilize funds (at the district level) for surveillance activities.
- Ensure timely release of funds for surveillance activities.
- Monitor IDSR performance and outputs of data analysis and monitoring tools.
- Participate in risk mapping of the district and in the development of a plan of action based on the findings.
- During outbreaks, assist the Emergency Preparedness and Response (EPR) committee in organizing the rapid response teams and ensure functionality (see section 5 for details).
- Report findings of the initial investigation to the Province/Region.
- Participate in risk mapping and community assessment.
- Participate in the establishment and ensure the functionality of the emergency preparedness and response committees.
- Design, train, and set up the implementation of community health education programs.
- Participate in and support response training for healthcare facilities and the community.
- Together with the Province/Region, select and implement appropriate public health responses.
- Plan timely community information and education activities.
- Document response activities.
- In case of outbreaks, send daily district situation reports.
Other Political Leaders at the District Level:
Political leaders like Village//Ward//District Officers are very important people and they assist in fostering behavioral change on disease surveillance. They can play the following roles:
- Support any declarations of a public health emergency.
- Develop an inventory and identify local human/financial/logistics support that can be provided locally. A quick response will often prevent spread.
- Ensure principles of hygiene and sanitation are followed (environmental cleanliness, availability of latrines and their utilization, advocate for people to drink clean and safe water, advocate personal hygiene and sanitation measures including handwashing).
- Report clusters of illness/death to a nearby health facility.
- Implement the bylaws to enhance principles of hygiene and sanitation.
- Take an active role in sensitizing community members on how to promote, maintain, and sustain good health.
- Facilitate community-based planning, implementation, and evaluation of health programs within the Ward (IDSR is among the programs).
- Make follow-up on any outbreak in collaboration with healthcare providers and other extension workers at the Ward level.
- Provide administrative backup to healthcare providers at the Ward and Village levels.
- Support the enforcement of relevant legislations to prevent/control the outbreak of infectious diseases.
- Supervise subordinates in ensuring principles of hygiene and sanitation are followed.
- Ensure the convening of regular Public Health Care Committee (or institute a Public Health Committee) when an outbreak occurs.
- Discuss disease patterns and their implications for action, as part of regular meetings with the District Medical Officer.
- Ensure that various committees are established and facilitated to perform activities.
- Solicit resources from various sources to respond to disasters, including epidemics.
- Conduct advocacy on health matters in different campaigns carried out in the district.
Regional or Provincial Health Management Team:
- Liaise with the Regional/Provisional Commissioner and national-level Chief Medical Officer/Director General of Health on surveillance activities and plans.
- Support the Regional Surveillance Officer and district surveillance officers to implement planned activities.
- Ensure surveillance activities are included in regional/provincial and district health plans.
- Mobilize funds and ensure timely release for surveillance and response activities.
- Monitor district IDSR performance and data analysis.
- Assist districts in risk mapping, developing action plans, and community assessments.
- Support districts in emergency preparedness, response training, and public health response.
Ministry of Health/National Level:
- Set up a Public Health Emergency Operation Center and incident management system.
- Identify a spokesperson and develop risk communication plans.
- Set standards, policies, and guidelines for IDSR and update emergency preparedness and response plans.
- Assess and rectify national-level capacity, including surge capacity.
- Mobilize and coordinate domestic and external support for IDSR implementation.
- Conduct overall supervision, monitoring, and evaluation of IDSR activities.
- Produce and disseminate epidemiological bulletins.
- Support investigation of suspected epidemics.
- Provide national-level data management and analytical support.
WHO and Other Partners:(UN Agencies, CDC, USAID, PATH MSF, REDCROSS, UNICEF)
- Contribute to setting standards and developing guidelines.
- Provide technical assistance, expertise, and material support to strengthen surveillance, laboratory, and health information systems.
- Support resource mobilization for surveillance and response activities.
- Assist in supervision, monitoring, and evaluation of IDSR.
- Provide management support, such as writing funding proposals.
- Support capacity building through training and equipment provision.
- During public health emergencies, provide technical experts, surge staff, portable laboratories, and other equipment and vaccines.
Roles of a Nurse in IDSR
Before we proceed with outlining the roles, let’s engage in the activity:
Activity:
Why is it important to involve a nurse in IDSR programs?
Answer: Nurses are vital in IDSR programs as they assume significant roles in healthcare delivery. Their involvement is crucial due to their extensive patient interactions and responsibilities in various healthcare settings. Nurses often serve as the frontline healthcare providers, offering care, education, and support to patients. Their presence in IDSR ensures early detection, prompt response, and effective management of disease outbreaks, leading to improved community health outcomes.
Roles
- Assessment and Reporting: Evaluate and report priority disease cases from lower levels to higher levels of authority.
- Coordination of Activities: Facilitate the smooth coordination of IDSR activities among stakeholders, including community members and technical personnel at the CDC.
- Planning and Preparation: Strategize and prepare for effectively managing disease outbreaks within the community.
- Assistance in Monitoring and Evaluation: Actively participate in monitoring and evaluating disease outbreak programs.
- Assessment, Analysis, and Reporting: Analyze, interpret, and compile straightforward reports for priority disease outbreaks using your knowledge in epidemiology.
- Engagement in Immunization Programs: Participate in immunization initiatives aimed at protecting the community against vaccine-preventable diseases. The Center for Disease Control and Prevention (CDC) advocates for early childhood vaccination against preventable diseases, a role that nurses fulfill.
Advantages of IDSR:
- It is cost-effective as it utilizes the same health personnel and reporting formats for routine health data.
- It enables the computerization of available data at the central level.
- It provides training and capacity building opportunities for health personnel to develop new skills.
- It encourages community participation in detecting and responding to disease outbreaks.
- It facilitates effective resource utilization and allocation.
- It enables quick response to public health events.
Challenges in IDSR implementation:
- Non-sustainable financial resources for IDSR activities.
- Lack of coordination among different stakeholders.
- Inadequate training and high turnover of peripheral/frontline health staff.
- Unreliable feedback mechanisms from higher to lower levels.
- Inadequate supervision and support from higher levels.
- Weak laboratory capacities and lack of job aids (case definitions, reporting formats).
- Poor availability of communication and transport systems, particularly at the peripheral level.
- Inadequate data management and analysis capabilities at various levels.
- Resistance to change from routine disease surveillance practices to the integrated approach.
- Lack of community engagement and ownership of the IDSR system.
- Weak linkages between animal and human health surveillance systems.
- Insufficient political commitment and leadership to sustain IDSR implementation.
- Fragmented health information systems that hinder data integration and analysis.
- Inadequate use of digital technologies and innovations to enhance IDSR.
- Challenges in adapting IDSR to changing epidemiological patterns and emerging threats.
- Limited capacity for timely outbreak detection, investigation, and response.
Let’s summarize what you’ve learned.
What Have We Learned?
Throughout this section, we delved into Integrated Disease Surveillance and Response (IDSR) in comprehensive detail. We covered its aims, objectives, and foundational requirements for effective implementation.
Major priority diseases were identified, with detailed case definitions provided for each. We explored the crucial aspects of supervisory monitoring and evaluation within IDSR and highlighted key individuals involved in these activities. Lastly, we delved into the roles a nurse plays in IDSR, emphasizing the importance of their involvement.
Now, it’s time to evaluate your understanding through a self-test. Attempt to answer the questions and consider discussing the information with your colleagues as you review your notes.
Self-Test:
- Which organization is directly involved in the implementation of IDSR in Uganda?
- Outline the measures you would take when planning for an epidemic disease outbreak.
- Utilizing a table, explain the case definition for the following diseases:
- Tetanus
- Tuberculosis
- Cholera
- Hepatitis “B”
- State one activity you would perform when monitoring and evaluating disease outbreaks in your workplace.
- Enumerate two major roles you would play in the IDSR program as a nurse.


Can we please get some revision questions.
Some of us wanted to join the WhatsApp group but all in Vine