Table of Contents
ToggleOrthopedic Care
Orthopedic care is concerned with preventing, recognizing, and treating injuries, diseases, and ailments that afflict the musculoskeletal system of the body.
This system consists
of muscles, tendons, ligaments, and other connective tissues that enable a human being to perform physical activity.
Orthopedic care involves treating common problems such as;
- Musculoskeletal trauma
- Sports injuries
- Degenerative diseases
- Infections
- Tumors
- Congenital disorder
Some of the techniques used to treat musculoskeletal ailments through orthopedic care include but are not limited to the following:
- Bandaging
- Traction
- Splints
- Non-surgical procedures
- Surgical procedures (such as ligament repair)
Bandaging
Purpose of Bandages
- To cover retain dressings and splints in place,
- To protect a wound,
- To support as in sprain,
- To compress,
- To secure dressing,
- To immobilize in fracture plaster of Paris cast,
- To Control bleeding from wounds,
- To restrict movement.
Types of Bandage
- Triangular Bandages: This type of Bandages is used in emergency treatment and first aid,
> Head bandage,
> Sling - Roller Bandage: >Circular
> Spiral, Recurrent. - Plaster : It is made from plaster of Paris, it immobilizes fractures of bones.
- Adhesive: It used for fracture at Clavicle bone.
- Gauze Bandages
- Crepe Bandages: These bandages are elastic and a degree to which they are stretched when applied
determines the amount of pressure they exert. They are widely used.
General rules of bandaging
- Use a tightly rolled bandage of suitable width and material.
- Face the patient when bandaging limbs.
- Hold the head of the bandage uppermost.
- Bandage the limb well aligned in an anatomical position.
- Hold the bandage in the right hand when bandaging a left limb and vice versa
- Bandage the limb from inside outwards and from below upwards, keeping the bandage even
throughout. - Ensure that the bandage is neither too tight nor too loose.
- Finish off the bandage with a straight turn, fold in the end and secure avoiding joints and the site of injury.
- Fasten with safety pins or with the provided fastener.
- Apply tape in psychiatric, mentally handicapped or paediatric patients instead of pins or other
sharp appliances.
Bandaging patterns
Figure of eight
- Observe general rules of all nursing procedures.
- Put patient to comfortable position exposing the affected part.
- Hold bandage with the drum facing upwards.
- Wrap bandage around the limb twice below the joint.
- Use alternating ascending and descending turns to form figure of eight; overlap each turn of the
bandage by one half to two-thirds the width of the strip. - Wrap bandage around the limb twice, above the joint to anchor it and secure end with a clip or
safety pin. - Elevate the bandaged extremity for 15 to 30 minutes after application of bandage.
- Assess the skin for color, integrity pain and temperature.
- Leave patient comfortable and clear away.
Spiral bandaging (e.g. bandaging the ear)
- Make a fixing turn around the head
- Bring the bandage under the ear and straight over the head and down the back, leaving the other
ear un-bandaged. - Repeat these turn three or four times until the affected ear is gradually covered.
- Finish with a fixing turn and secure the bandage at the centre of the forehead using a safety pin
clip or tape. - Divergent Spica (pattern used to cover a dressing wound at a fixed joint e.g. Knee, heel or elbow).
- Make two turns over the centre of the joint.
- Now make alternate turns above and below these turns forming a pattern at each side of the
joint
Triangular Bandaging Arm sling
- Place the injured arm across the patient’s chest so that the fingers almost touch the opposite
shoulder. - Place one corner of the bandage over the uninjured part with the right angled corner just above
the level of the elbow of the injured side. - Tuck the other upper half of the base of the bandage well beneath the forearm and elbow.
- Carry the corner ends across the back and tie the ends with a reef knot, which lies in the hollow
above the clavicle on the un-injured side. - The right angle is folded and pinned to enclose the elbow.
- Place a pad under the knot if it seems likely to cause pressure.
Bandaging the Eye
- Facing the patient; hold the eye pad in position until the bandage covers it.
- Begin from the affected side to the normal across the forehead and round the head in a fixing
turn, then from the back of the head the bandage comes under the ear, across the eye covering
the nasal side of the pad and straight over the head and down the back. - The next turn comes under the ear, overlaps the eye turn, crosses the fixing turn at the same
point as the other, then overlaps it crosses the head and comes round to the front. - Fix a pin should be in the centre of the forehead.
Capeline Bandage (Use a double headed roller bandage) Position patient in sitting up position and stand behind the patient)
- Place the centre of the outer surface of the of the bandage in the centre of the fore head
- Bring the head of the bandage around over the temples and above the ears to the nape of the
neck when the ends are crossed - Bring the upper bandage around the head and the other head of the bandage over the centre of
the top of the scalp and then to the root and nose - Bring the bandage which circles the victims head over the fore head covering and fixing the
bandage which crosses the scalp. - The bandage is then brought back over the scalp.
- Ensure that each turn of the bandage covers 2/3 of the previous turn
- Cross it again at the back and fix it using encircling bandage and turn back over the scalp to the
opposite side at the central line now covering the other margin of its original turn - Repeat the back word and forward turns to alternate side of the centre, each one begin in turn
fixed by the encircling bandage until the whole scalp is covered - Take two circular turns around the head, secure bandage with safety pin
Recurrent bandaging
- Overlap each layer of bandage by half to two thirds the width of the strip; wrap firmly but not
tightly as you work ask the patient if it feels comfortable. Loosen the bandage if there is tingling,
itching, numbness or pain. - Stand facing the patient and take a fixing turn.
- Carry the bandage upward across the front of the limb at 450 rounds behind it at the same level
and downwards over the front to cross the first turn at a right angle. - Repeat these turns until the limb has been sufficiently covered.
Splints
Injuries that result in instability require immobilization, decreasing the likelihood of further damage, protecting soft tissues, alleviating pain, and accelerating healing. Instability may result from direct injury to the bones (fracture), joints (dislocation), or the soft tissues such as the muscles (strain) or ligaments (sprain).
Following the diagnosis of an unstable injury, a splint may be the best treatment option and is defined as an external device used to immobilize an injury or joint and is most often made out of plaster.
A splint must be differentiated from a cast, to determine the best form of immobilization based on the clinical scenario. Contrary to a splint, a cast is a circumferential application of plaster that rigidly immobilizes a particular joint or fracture. Because of their circumferential restrictive nature, casts are not placed in the acute post-injury setting as they do not accommodate for soft tissue swelling.
Indications
Splints are placed to immobilize musculoskeletal injuries, support healing, and to prevent further
damage. The indications for splinting are broad, but commonly include:
- Temporary stabilization of acute fractures, sprains, or strains before further evaluation or definitive operative management
- Immobilization of a suspected occult fracture (such as a scaphoid fracture)
- Severe soft tissue injuries requiring immobilization and protection from further injury
- Definitive management of specific stable fracture patterns
- Peripheral neuropathy requiring extremity protection
- Partial immobilization for minor soft tissue injuries
- Treatment of joint instability, including dislocation.
Equipment
Obtain and organize all equipment before splint application. The necessary equipment for a plaster or
fiberglass splint includes:
- Sheet or towel to protect patient clothing
- Stockinette (a soft, loosely knitted stretch fabric) or fabric under padding
- Under cast padding, which is typically made out of cotton.
- Plaster (8-10 sheets thick) or padded fiberglass. In general, forearm splints require smaller width,
and upper arm and leg splints require larger width rolls of material. - Water bucket filled with cool water.
- Elastic bandage
- Sling for upper extremity injuries
- If fracture reduction is attempted, a C-arm X-ray should be used for the evaluation of the fracture
reduction.
General steps may be applied when placing a splint
- Ensure adequate analgesia before splint application. This will ensure muscle relaxation and facilitate fracture reduction, if necessary.
- Ensure that any soft-tissue injuries are addressed before splint placement.
- Apply a stockinette circumferentially to the injured area. This should span both proximally and distal to the injured area, protecting the skin from irritation by the plaster or fiberglass.
- Pad bony prominences such as the elbow, knee, or calcaneus with at least 1 cm to 2 cm of soft cast padding. Soft tissue protection is essential to prevent future skin irritation or necrosis. The thickness of this padding will depend on body habit.
- Apply 2-3 layers of cast padding (0.25 cm to 0.5 cm) circumferentially to the remaining area of
immobilization. - Reduce any fracture by restoring the bone length, rotation, and alignment. This may require radiographic confirmation before support material application.
- Activate the supportive plaster or fiberglass layers by saturating them in the water bucket. Laminate the sheets by pressing them together before application, as this increases the strength and adhesion between the layers.
- Mold the supportive material around the area of injury. The specific molding approach will depend on the type of injury; however, as a general rule, the splint should be molded to resist any deforming angulation.
- Ensure the supportive material does not circumferentially encase the injured area to accommodate any soft-tissue swelling. If there is circumferential overlap, this should be addressed by cutting the splint once the supportive material has set.
- Fold the stockinette over the plaster or fiberglass to protect the patient’s skin from its sharp edges.
- Circumferentially apply an elastic bandage around the splint. This aids in the molding of the splint material to the injured area and holds the support material in place until it has hardened. Direct placement on the skin should be avoided and is a commonly observed mistake.
- Repeat the physical exam to ensure that there is no significant change in the patient’s neurovascular status. Any change in the physical exam should prompt the rapid removal of the splint and reassessment.
- Counsel the patient on proper splint care and follow-up instructions.
Common upper extremity splints include:
1. Coaptation splint
2. Sugar tong splint
3. Posterior long arm elbow splint
4. Ulnar gutter splint
5. Radial gutter splint
6. Volar or dorsal short arm splint,
7. Thumb spica splint
Common lower extremity splints include:
1. Posterior long leg splint, posterior short leg splint
2. Posterior short leg splint with stirrups
Complications of Splints
- Loss of fracture reduction
- Skin irritation or breakdown
- Joint stiffness.
- Thermal injury
- Neurovascular compromise – acute carpal turnel syndrome
- Compartment syndrome – Excessive compression may occur through splint placement, mainly if a splint is circumferential, becoming a cast.
Traction
This is a system in fracture management in which a continuous pull is applied and maintained on a limb or other parts of the body by the use of cords and weights.
Indications
➢ To correct joint deformities
➢ To separate joint surfaces and so prevent further spread of infection e.g TB of the joints like hips, knees.
➢ To prevent muscle spasms
➢ To prevent and overriding of bones since it keeps/maintains bones in the right position during the healing process.
Types of traction
- Skeletal traction
- Skin traction
a) Hamilton Russel traction
b) Gallows traction - Pulp traction
- Halo traction
- Skull tongs traction
- Fixators
a) Internal
b) External
SKELETAL TRACTION
This is the type of traction in which a pin, nail or wire is passed through a bone.
This type of traction is mainly used for the treatment of fractures and works better for well-built strong persons.
Common sites for introducing the pins include;
1. The condyles of the femur
2. The tubercles of the tibia
3. Calcaneus at the heels of the foot.
Metallic equipment used in skeletal traction
- Steinmann’s pins: This is a rigid steel pin passed through a bone and attached to a special stirrup. Because of the presence of the stirrup, the surgeon is able alter the line of the pull without moving the pin.
- Kirschner wire: This is a narrow steel wire which is not rigid unless pulled on by a stirrup when the stirrup is rotated. It can move the wire and so possibility for infection is high hence this is not commonly used compared to the Steinmann’s pin.
Preparation of the patient for skeletal traction
➢ Explain the procedure to the patient and provide reassurance to allay anxiety
➢ Do shaving if the patient is hairy.
➢ Do premedication if prescribed.
➢ Institute an intravenous line.
After the preparation, the patient s taken to the theater with the leg in Thomas splint with skin traction
applied, then an operation is done under general anesthesia in order to insert the Steinmann’s pin
through the bone. A stirrup is then attached to the pin and the patient returned to the ward.
Requirements for making a skeletal traction.
Trolley:
Top shelf:
➢ Extension cord
➢ 6-8 metal pulleys
➢ Cotton wool in a gallipot
➢ Receiver of forceps and scissors
➢ Gallipot of gauze
➢ Antiseptic lotion e.g. iodine in gallipot
Bottom shelf:
➢ Thomas splint
➢ Knee piece
➢ Foot piece for Thomas splint
➢ Strong slings, safety pins
➢ Weights e.g. sandbags of required weight by the doctor
➢ Bed elevators e.g. bed blocks
➢ Strapping.
At the bed side.
➢ Balkan bean
➢ Fracture boards.
Specific care for a patient on skeletal traction.
1. Pin:
Report any sign of inflammation, discharge or movement of the pin.
2. Traction.
➢ Cords and pulleys must be free and smooth running
➢ Cords must be long enough and must not touch the toes.
➢ The cord must not be knotted or kinked
➢ Weights should be secure and hanging freely
SKIN TRACTION
It involves applying splints, bandages, or adhesive tapes to the skin directly below the fracture. Once the material has been applied, weights are fastened to it. The affected body part is then pulled into the right position using a pulley system attached to the hospital bed.

Preparation of the patient for a skin traction
- Relevant explanation is given to the patient to ensure cooperation. Explanation should also be given to the relatives who may consider that apparatus cruel.
- Ensure firm base on the bed and comfortable mattress.
- Ensure privacy, wash the leg and dry thoroughly observing any abrasions, which should be
reported immediately. - Shave the leg if necessary taking particular care not to cause any skin damage.
- Paint the skin with tincture of benzoin compound, which eliminates allergic reaction to strapping
and assists adhesive properties. - Protect the bony prominences with adhesive felt or latex foam or orthopaedic wool.
Bed: - This should have a firm base, use fracture boards if necessary
- Soft mattress
- The bedclothes should be arranged in separate packs for the trunk and limb not in traction.
- The patient must be kept warm and bed tidy at all times (this is important for patients morale.)
- Bed cradle should be used if both legs are in traction to ensure that the bedclothes do not hamper the efficiency of the traction.
- If there is an overhead beam, a trapeze should be applied to enable the patient lift himself up, thus help prevent formation of pressure sores and hypostatic pneumonia.
- Bedclothes are necessary if the patients own weight is a counter traction.
Management of a patient with skin tractions
Acute management
1. Ensure Order for Skin traction is documented by the Orthopaedic Team-(including weight to be applied in kgs)
2. Preparation of equipment
Top Shelf
- Shaving tray
- Receiver containing: A
pair of dressing forceps, 21
dissecting forceps - Bowl containing swabs
- Extension plaster
- A pair of Scissors
- Crepe bandages
- Tape measure
- Skin pencil
Bottom Shelf
- Receiver for used swabs
Spreader - Cordiallv, Brown wool or
sorbo pads - Tincture of benzoin co.
- Dressing mackintosh and
towel - A small blanket to cover the limb
- Balkan Beam
- Bed blocks
Bed Side
- Hand washing equipment
- Screens
- Bucket for used
equipment - Weights in various
kilograms
On the bed - Pulleys
- Fracture board
3. Pain relief: A femoral nerve block is the preferred pain management strategy and should be administered in the emergency department prior to being admitted to the ward.
– Diazepam and Oxycodone should always be charted and used in conjunction with the femoral nerve block.
4. Distraction and education: Explain the procedure to the parents and patient before commencing.
– Plan appropriate distraction from play therapy, parents or other nursing staff.
5. Application of traction: Ensure the correct amount of water has been added to the traction weight bag as per medical orders.
– Fold foam stirrup around the heel, ankle and lower leg of affected limb. Apply bandage, starting at the ankle, up the lower leg using a figure 8 technique, secure with sleek tape.
– Place rope over the pulley and attach traction weight bag. If necessary trim rope to ensure traction weigh bag is suspended in air and does not sit on the floor.
Ongoing management
6. Maintain skin integrity: Patient’s legs, heels, elbows and buttocks may develop pressure areas due to remaining in the
same position and the bandages.
– Position a rolled up towel/pillow under the heel to relieve potential pressure.
– Encourage the patient to reposition themselves or complete pressure area care four hourly.
– Remove the foam stirrup and bandage once per shift, to relieve potential pressure and observe condition patients skin.
– Keep the sheets dry.
– Document the condition of skin throughout care in the progress notes and care plan
– Ensure that the pressure injury prevention score and plan is assessed and documented.
7. Traction care: Ensure that the traction weight bag is hanging freely, the bag must not rest on the bed or thenfloor
– If the rope becomes frayed replace them
– The rope must be in the pulley tracks
– Ensure the bandages are free from wrinkles
– Tilt the bed to maintain counter traction
8. Observations: Check the patient’s neurovascular observations hourly and record in the medical record.
– If the bandage is too tight it can cause blood circulation to be slowed.
– Monitoring of swelling of the femur should also occur to monitor for compartment syndrome.
– If neurovascular compromise is detected remove the bandage and reapply bandage not as tight. If circulation does not improve notify the orthopaedic team.
9. Pain Assessment and Management: Assessment of pain is essential to ensure that the correct analgesic is administered for the desired effect
– Paracetamol, Diazepam and Oxycodone should all be charted and administered as necessary.
– Pre-emptive analgesia ensures that the patient’s pain is sufficiently managed and should be considered prior to pressure area care.
– Assess and document outcomes of pain management strategies employed.
10. Activity: The patient is able to sit up in bed and participate in quiet activities such as craft, board games and watching TV. Play therapy will be beneficial for patients in traction long term.
– Non-pharmacological distraction and activity will improve patient comfort.
– The patient is able to move in bed as tolerated for hygiene to be completed.
– Patients who are in traction for a number of weeks may require a referral to the education
department.
11. Theatre time
The patient should be transported to theatre in traction to reduce pain and maintain alignment.
Special considerations
The foam stirrup, bandage and rope are single patient use only.
Potential complications
- Skin breakdown/pressure areas
- Neurovascular impairment (assessment of circulation, oxygenation and nerve function of limbs within the body)
- Compartment syndrome (Increased pressure within one of the bodies compartments which contain muscles and nerves. )
- Joint contractures
- Constipation from immobility and analgesics
PULP TRACTION
This is the type of traction used for management of displaced phalanges, metacarpals and metatarsal fractures. A structure is put through the pulp of the fingers and fastened to an extension wire which is incorporated in the plaster.
SKULL TONGS TRACTION.
This kind of traction is used to immobilize the cervical spine in the treatment of unstable fractures or dislocation of a cervical spine.
Types of skull tongs traction.
➢ Crutchfield tongs
➢ Gardner wells tongs
NB: Gardner wells tongs is widely used by most experts because it is believed that its less likely to pull out compared to the Crutch field tongs.
Procedure.
In either type of tongs, the patient is prepared psychologically, physically and made to consent. This process may be done in theater under anesthesia. The tongs are surgically inserted into the bony cranium and a connector half halo brace is attached to a hook from which traction can be applied.
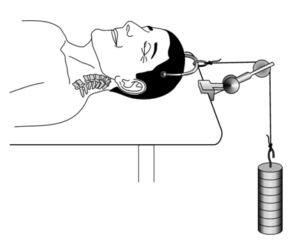
After procedure:
➢ After the procedure the patient is put on a special bed with a special mattress and therapeutic frames.
➢ The position used is complete supine with a small pillow under the head.
➢ Since patients remain in this type of traction for long, the same precautions taken in other types of skeletal traction must also be observed.
➢ The head of the bed is elevated to provide counter traction.
➢ Castors are placed on this bed to allow easy wheeling in case of any movement to the x-ray etc.
Points to remember
➢ Perform activities of daily living for the patient because this patient has difficulties doing it for himself.
➢ Prevent infection at the tong sites by regular cleaning
➢ Suggest recreational or occupational activities since restlessness and boredom are common concerns.
➢ Teach the patient range of motion exercises.
➢ Provide good nutrition.
HALO TRACTION
This is quite similar to the skull tongs traction. It serves the purpose of providing stabilization and support for fractured cervical vertebrae.
The pin is inserted into the skull, but the difference is that its got a vertical frame piece that extends to the rest of the patient and allows movement out of bed without intervening its function.
This frame cannot be removed because any movement of the vertebrae could injure the spinal cord.
FIXATORS
These are metallic rods passed through a bone to ensure stability.
Types;
- External fixation devices
This is a frame of metal rods that connect skeletal pins. These rods extend and provide tractions between the pin sites. They can be simple with two to three connecting rods but can also be complexed with many rods arranged at different angles to maintain the position of fractured bone fragments.
Advantages
➢ Can be used when many bone fragments are to be immobilized.
➢ Used when open wounds are present externally to prevent the possible risk for infection especially
seen in casts. - Internal fixator Metallic devices used either to replace certain bones or treat certain fractures. Can be temporal or permanent especially if it were put for the purpose of replacing a dead bone like missing head of the femur.
GENERAL NURSING CARE OF A PATIENT ON TRACTION
- Traction should be put at day time preferably
- The patient is nursed with fracture boards on the bed so as to keep firm
- The foot or head of the bed is kept elevated at all times depending on the site of traction(skull or limbs).
- Do not lift, move or remove weights unless asked to do so by the doctor. Make sure the cords are always pulling and the weights not resting on the bed. The beds are elevated using bed blocks and the traction is maintained throughout the 24 hours per day because sudden cessation irritates diseased joints, causes displacement in a fracture and its very painful for the patient.
- The cords must run freely over the pulleys oiled regularly.
- Watch the color of the toes to ensure circulation is satisfactory.
In case of skeletal traction: –
➢ The puncture site must be kept clean and dry.
➢ Use tincture benzoin-co. to seal the wound.
➢ Observe the screws on either side of the pin to ensure free movement, lubricate the screw of oil if necessary.
➢ Keep a cork on the sharp point of the pin to prevent injury and pulling off.
➢ Provide the patients bed with an overhead lifting pole and chain to help the patient lift himself.
➢ When giving a bed pan ask the patient to lift himself or ask for assistance and do it if the patient is unable.
➢ Change bottom sheet from head to toe. - Assist patient with bathing where he or she cannot wash for himself eg the back, legs. bathing is done daily. Keep care full attention to pressure areas especially around the ring of the Thomas splint.
- Patient is kept on full diet. Encourage foods with extra vitamins, minerals eg iron, milk, liver.
- Teach patients muscle exercises to be done daily and to move the joints eg knee and ankles.
- Give psychological care by regular re assurance.
- Provide indoor games to occupy patient.
Care of P.O.P
- Elevate the limb on a pillow
- Elevate the foot of the bed.
- Wash the plaster powder off the toes
- Expose the P.O.P to room temperature
- Observe the toes for good blood supply.
- Ask the patient to move with toes from time to time
- Half hourly pressure check for pressure on the nerves
- Check the color of the toes
- Check the temperature of the toes by the back of your hands
- Observe any swelling of the toes
- Check the pain which shows pressure
- Check for loss of sensation or movement of the toes
- Check for numbness or tingling due to nerve pressure.
- Check for any blood stains on P.O.P meaning there is bleeding.
- Physiotherapy;
- Ensure deep breathing exercise
- Ensure limb movement of an affected site.


Very fine