Syndromic Approach
Syndromic approach to STI management is a method of diagnosing and treating sexually transmitted infections (STIs) based on the patient’s clinical signs and symptoms, rather than laboratory confirmation.
Instead of targeting a specific pathogen, healthcare providers address the symptoms and syndromes associated with various STIs.
It is very useful in settings where laboratory testing is limited or unavailable.
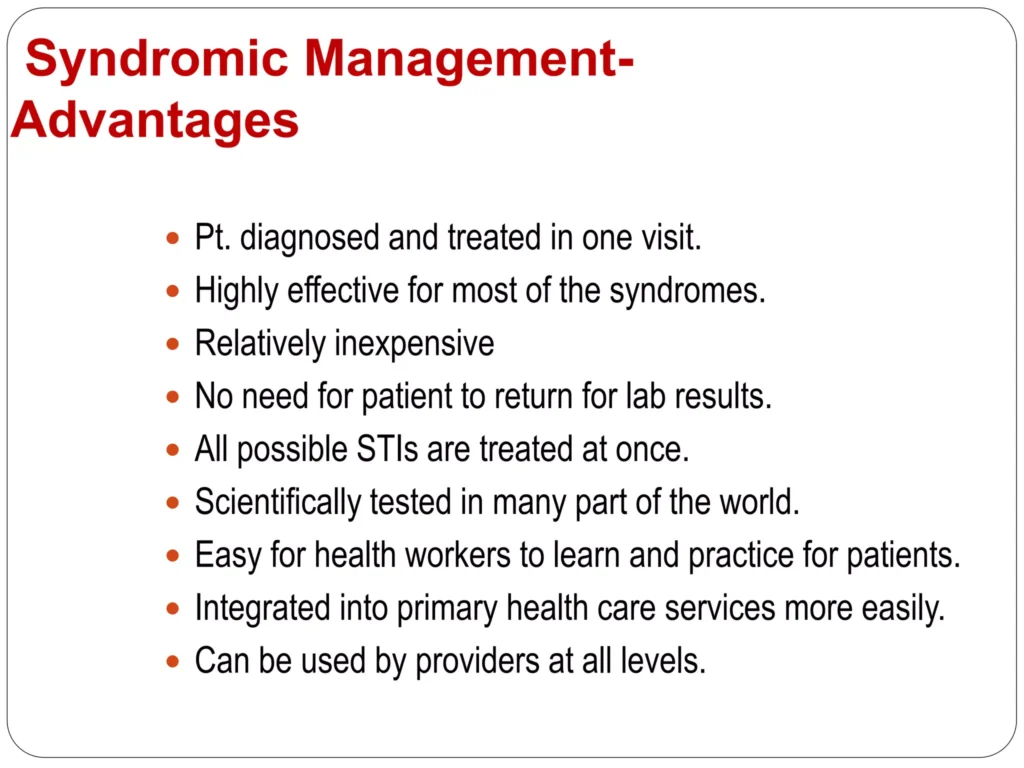
Advantages of using Syndromic Approach.
Improved Clinical Diagnosis:
- The syndromic approach can help to improve clinical diagnosis of STIs, as it allows healthcare providers to identify and treat STIs based on the patient’s symptoms and signs, even if laboratory testing is not available. This can help to reduce the number of misdiagnoses and ineffective treatments.
Ease of Learning for Primary Health Care Workers:
- The syndromic approach is easy for primary healthcare workers to learn, as it does not require specialized equipment or training. This makes it a feasible approach for use in resource-limited settings where laboratory testing may not be available.
Rapid diagnosis and treatment:
- The syndromic approach allows for rapid diagnosis and treatment of STIs, as it does not require waiting for laboratory results. This can help to prevent complications and reduce transmission of STIs.
Same-Visit Treatment for Symptomatic Patients:
- Symptomatic patients can receive immediate treatment during a single visit, eliminating the need for multiple visits for laboratory tests. This accelerates care and minimizes patient inconvenience.
Cost-effectiveness:
- The syndromic approach is more cost-effective than laboratory-based testing, as it does not require expensive equipment or reagents. This makes it a more sustainable approach for use in resource-limited settings.
Accessibility at Lower Health Units:
- Treatment is available at the initial point of contact with the healthcare system, extending STI management even to lower health units. Referrals are reserved for complex cases.
Preventive Partner Treatment:
- The syndromic approach includes the treatment of sexual partners, contributing to preventing reinfection and interrupting the transmission cycle.
Resource Efficiency:
- Resource utilization is optimized as the approach minimizes the demand for laboratory testing, making it suitable for resource-limited settings.
Increased access to treatment:
- The syndromic approach can help to increase access to treatment for STIs, as it allows healthcare providers to treat patients without having to wait for laboratory results. This is particularly important in settings where patients may have difficulty accessing laboratory services.
Disadvantages of using Syndromic Approach
Inadequate Care for Asymptomatic Individuals:
- The syndromic approach may overlook individuals with STDs who exhibit no symptoms, particularly asymptomatic women. This limitation hinders the identification and treatment of silent infections.
Overuse/Wastage of Medications:
- The syndromic approach can lead to wasting of drugs, as patients may be treated for STIs that they do not actually have. This can be a particular problem in settings where resources are limited.
Poor Predictive Value for Some Infections:
- Symptoms and signs, especially in women, may have limited predictive value for certain STIs, such as gonococcal and chlamydial infections. This can result in missed diagnoses and delayed appropriate treatment.
Risk of Antibiotic Resistance:
- Over reliance on syndromic treatment may contribute to antibiotic resistance, as broad-spectrum antibiotics are often used without targeting the specific pathogens causing the infection.
Challenges in Addressing Co-Infections:
- Co-infections with multiple pathogens may pose challenges as the syndromic approach focuses on a single syndrome, potentially missing the concurrent presence of different STIs such as Chlamydia or Gonorrhea, in individuals with genital ulcers who are also infected with genital herpes or syphilis. This can lead to inadequate treatment and potential complications.
Inefficacy for Viral Infections:
- The approach may be less effective for viral STIs, as antiviral medications may require specific identification of the viral agent, which the syndromic approach does not provide.
Potential for misdiagnosis:
- The syndromic approach may lead to misdiagnosis of STIs, as it is not always possible to accurately identify the specific STI causing the symptoms based on clinical signs and symptoms alone. This can lead to incorrect treatment and potential complications.
Inadequate care for asymptomatic patients:
- The syndromic approach does not adequately care for people with STIs who have no symptoms, especially women with STIs, as they are often asymptomatic. This can lead to untreated infections and potential complications.
NOTE:
There are different approaches to STI diagnosis and management.
SO, In our current circumstances, the advantages of syndromic approach outweigh the disadvantages. A theoretical comparison of the cost effectiveness of the three approaches to diagnose 500 patients with genital ulcer, 500 patients with urethral discharge, and 500 with vaginal discharge found that the clinical and laboratory approach to diagnosis and management, each cost 2 -3 times as much as syndromic diagnosis. The cost of personnel and consequences of incorrect diagnosis accounted for most of the difference. By treating all STDs that cause a syndrome, syndromic diagnosis avoids many complications. Even in developed countries, many health care providers prefer to use the syndromic approach to avoid delay in treating their patients while waiting for laboratory results. |
RATIONALE OF SYNDROMIC APPROACH
Limited laboratory facilities:
- In many healthcare settings, particularly in resource-limited areas, laboratory facilities for STI testing may be limited or unavailable.
- The syndromic approach allows for the diagnosis and treatment of STIs based on clinical symptoms and signs, without the need for laboratory confirmation.
Multiple organisms causing STI syndromes:
- Most STI syndromes can be caused by more than one organism.
- For example, urethral discharge in men can be caused by Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis.
- The syndromic approach uses broad-spectrum antibiotics that are effective against a wide range of organisms, ensuring effective treatment even when the specific causative agent is unknown.
Delayed laboratory results:
- Even where laboratory facilities exist, test results may not be immediately available.
- Patients may be unlikely to return for their results and treatment, leading to delays in diagnosis and treatment and increased risk of transmission.
- The syndromic approach allows for immediate treatment, reducing the risk of complications and transmission.
Common occurrence of mixed infections:
- Mixed infections, where a patient is infected with more than one STI, are common.
- The syndromic approach uses broad-spectrum antibiotics that are effective against a range of organisms, increasing the likelihood of treating all infections.
Influence of self-medication and immunity on clinical picture:
- Self-medication and immunity can alter the clinical presentation of STIs, making it difficult to make a specific diagnosis based on symptoms alone.
- The syndromic approach provides a standardized treatment approach that is effective regardless of the specific causative organism or the influence of self-medication and immunity.
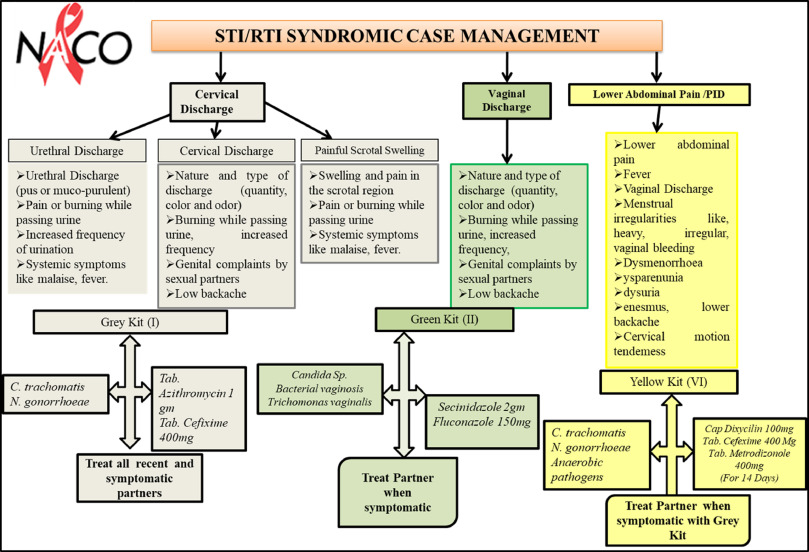
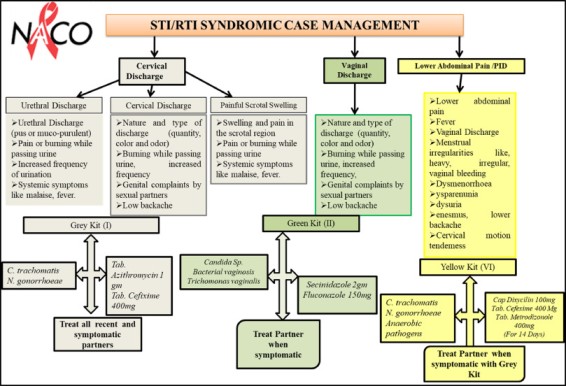
STD Syndromic Treatment Flow Charts (Algorithms)
Diagnosis and treatment flow charts formalizing the Syndromic approach have been developed. They provide health workers with step by step instructions to diagnose and treat STDs with recommended drugs.
STD syndromic treatment flow charts, also known as algorithms, offer several advantages in the diagnosis and management of sexually transmitted infections (STIs):
- Problem-oriented and improved clinical diagnosis: Algorithms are designed to focus on the specific symptoms and signs of STIs, guiding healthcare providers in making accurate diagnoses.
- Training tool for primary care providers: Algorithms serve as valuable training tools for primary care providers, including those with limited experience in STI management.
- Standardization of treatment: Algorithms promote the standardization of STI treatment across different healthcare settings and providers. This consistency ensures that patients receive appropriate and evidence-based treatment, reducing variations in care.
- Disease surveillance: Algorithms facilitate the collection of standard data on STI diagnoses and treatments. This information is important for disease surveillance, monitoring trends, and evaluating the effectiveness of STI control programs.
- Evaluation of training: Algorithms can be used to assess the effectiveness of STI training programs for healthcare providers. By comparing the diagnostic and treatment practices of providers before and after training, the impact of training interventions can be evaluated.
- Treatment in one visit: Algorithms enable the diagnosis and treatment of STIs in a single visit, improving patient convenience and reducing the risk of transmission. This is particularly important in settings where patients may have limited access to healthcare services or may be reluctant to return for multiple visits.
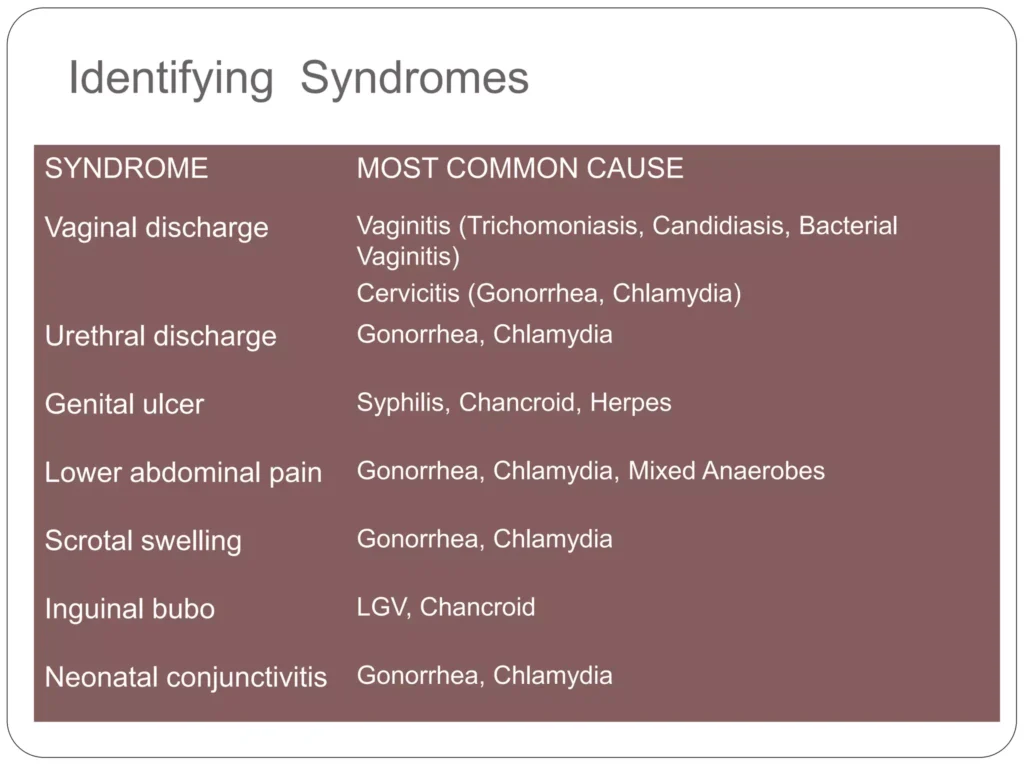
STI SYNDROMES
Commonest:
- Urethral discharge
- Abnormal vaginal/cervical discharge
- Genital ulcers
- Lower abdominal pain
- Enlarged groin lymph nodes (Bubo)
Others:
- Painful scrotal swelling
- Bartholin’s abscess
- Conjunctivitis with pus in newborn (ophthalmia neonatorum)
- Genital growth
- Inflammation of glans penis and prepuce (Balanitis)
- Acquired immunodeficiency syndrome