Abnormal Vaginal Discharge Syndrome
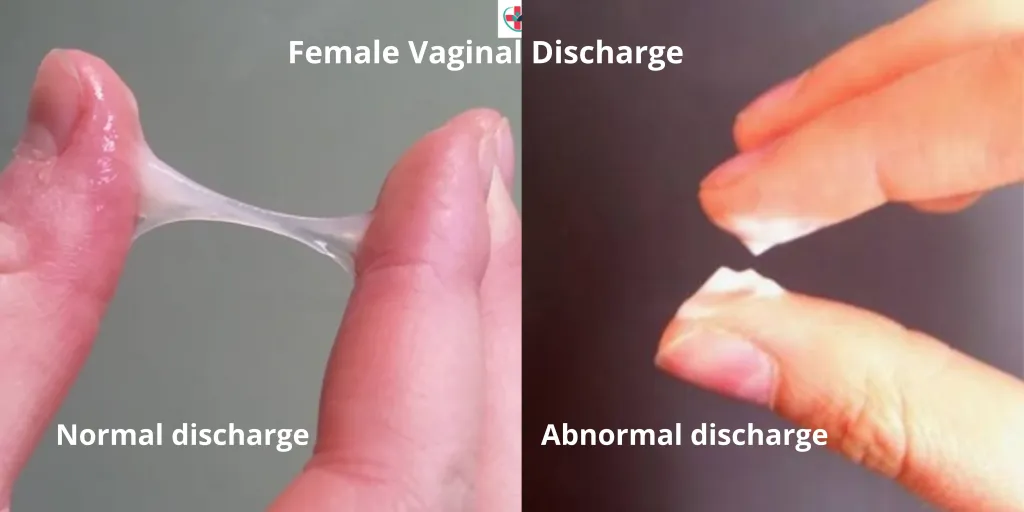
Abnormal vaginal discharge is defined as discharge that is different from usual with respect to colour/odour/consistency (e.g. discoloured or purulent or malodorous).
While all women experience physiological vaginal discharge, concerns arise when it is perceived as abnormal. This syndrome is primarily attributed to endogenous vaginal infections, such as bacterial vaginosis and vaginal candidiasis, which are not exclusively sexually transmitted.
Candida vaginitis and bacterial vaginosis are NOT sexually transmitted diseases, even though sexual activity is a risk factor.
Case Definition:
Abnormal vaginal discharge (indicated by amount, colour, and odour) with or without lower abdominal pain or specific risk factors.
Aetiology:
- Vaginitis and Vaginosis: Commonly caused by bacterial vaginosis(by Gardnerella vaginalis, Mycoplasma hominis), vulvovaginal candidiasis, and trichomoniasis.
- Cervicitis: Gonococcal and chlamydial infections contribute to cervicitis, which is often asymptomatic, and rarely a cause of abnormal vaginal discharge.
Clinical Presentation:
All women with vaginal discharge are treated for trichomoniasis, bacterial vaginosis, and candidiasis.
Increased Quantity of Discharge, Abnormal Color, and Odor:
- Lower abdominal pain, itching, and discomfort during sexual intercourse may be reported.
- Candida Albicans Vaginitis: Characterized by a very itchy, thick, or lumpy white discharge and red, inflamed vulva.
- Trichomonas Vaginalis: Presents with an itchy, greenish-yellow, frothy discharge accompanied by an offensive smell.
- Bacterial Vaginosis: Manifests as a thin discharge with a distinct fishy odour.
Specific Discharge Characteristics for Different Infections:
- Gonorrhoea-Induced Cervicitis: Rarely causes vaginitis. Presents with purulent, thin, mucoid, slightly yellow pus discharge devoid of smell and non-itchy.
- Chlamydia-Induced Cervicitis: May present with a non-itchy, thin, colourless discharge.
Note: Microscopy and speculum examination are recommended to rule out early lesions of cervical carcinoma.
Management:
Women with vaginal discharge should be managed according to the flow chart. The flow chart differentiates between candidiasis and other vaginal discharges.

However, all women with abnormal vaginal discharge are treated for bacterial vaginosis and trichomoniasis and candidiasis. At the moment, it is not possible in this country to identify women with cervicitis, and all women with a non- curd like discharge should be treated for cervicitis.
Management Protocol for Abnormal Vaginal Discharge Syndrome:
Initial Assessment:
- Conduct a thorough history and examine for genital ulcers and abdominal tenderness.
- Perform speculum examination to check for cervical lesions.
- Assess the risk for sexually transmitted diseases.
Lower Abdominal Tenderness with Sexual Activity:
- If lower abdominal tenderness is present and the individual is sexually active, treat as per Pelvic Inflammatory Disease (PID) guidelines.
Thick, Lumpy Discharge with Itching and Erythema/Excoriations (Likely Candida):
- Administer Clotrimazole pessaries 100 mg: Insert high in the vagina once daily before bedtime for 6 days or twice daily for 3 days.
- Alternatively, prescribe Fluconazole 200 mg tablets as a single oral dose.
- Consider Metronidazole 2 g stat dose if indicated.
Abundant/Smelly Discharge (Possible Trichomonas or Vaginosis):
- Prescribe Metronidazole 2 g stat dose.
Purulent Discharge, High STD Risk, or Previous Ineffective Treatment:
Treat for Gonorrhea, Chlamydia, and Trichomonas:
- Cefixime 400 mg stat or Ceftriaxone 1g IV stat.
- Doxycycline 100 mg 12 hourly for 7 days.
- Metronidazole 2 g stat dose.
- If pregnant, replace Doxycycline with Erythromycin 500 mg every 6 hours for 7 days or Azithromycin 1 g stat.
- Ensure partner treatment.
Persistent Discharge or Dysuria Despite Partner Treatment:
- Refer the individual for further management.
Key management points include:
Treatment for Vaginal Infections:
- All women are treated for bacterial vaginosis, trichomoniasis, and candidiasis.
- Identification of cervicitis is challenging; hence, all women with non-curd-like discharge are treated for cervicitis.
Promotion of Syndromic Management Package:
- Encourage adherence to comprehensive STI management, including partner treatment, preventive measures, and health education.
Communication:
- Explain the endogenous and recurrent nature of vaginitis to patients to prevent marital discord.
- Partners with urethral discharge should be treated for cervicitis.
Evaluation and Referral:
- Persistent abnormal vaginal discharge warrants evaluation to exclude cervical cancer.
- Speculum examination and referral for specialist management may be necessary.
Counsel and educate all clients on:
- Treatment compliance.
- Condom use and provide condoms.
- Partner management.
- Offer or refer for HIV VCT services if necessary.
- Schedule a return visit.
- Abstaining from sex till symptoms resolve.

well done thanks for the good notes