Table of Contents
ToggleGenital Ulcer Syndrome
Genital ulcer disease is a common syndrome affecting both men and women, characterized by single or multiple ulcers with different clinical manifestations.
Genital ulcer disease refers to breaks in the skin or mucosa and may present as ulcers, sores or vesicles.
Case Definition:
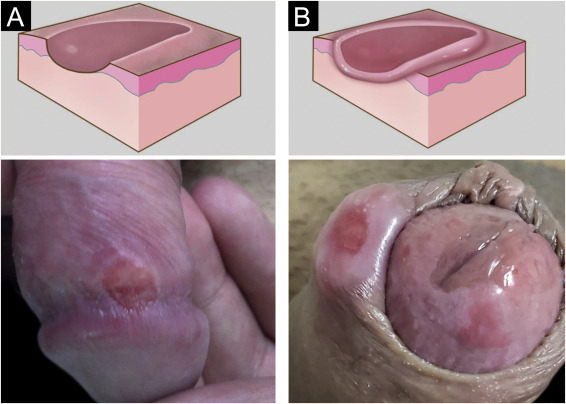
Non-vesicular Genital Ulcer: Ulcer on the penis, scrotum, or rectum in men, and on the labia, vagina, or rectum in women, with or without inguinal adenopathy. Vesicular ulcers involve the presence or history of vesicles.
Causes:
The aetiology of this syndrome varies across geographical regions and can evolve over time, often presenting challenges due to mixed infections and the influence of HIV.
- Non-vesicular Ulcers: Commonly caused by syphilis, chancroid, lymphogranuloma venereum, granuloma inguinale, or atypical cases of genital herpes (HSV infection).
- Vesicular Ulcers: Primarily caused by Herpes genitalis, syphilis, and Chancroid in Uganda.
Multiple organisms can cause genital sores, commonly:
- Treponema pallidum bacteria: syphilis
- Herpes simplex virus: genital herpes
- Haemophilus ducreyi: Chancroid
- Donovania granulomatis: Granuloma inguinale
- Chlamydia strains: lymphogranuloma venereum (LGV)
Clinical Presentation:
In men, genital ulcer disease occurring under the prepuce may present with a discharge in uncircumcised male patients, therefore, prepuce should be retracted and examined for ulcer lesions.
Female patients should have the labia separated and inspected, with speculum examination if necessary.
Mixed infections are common
- Primary syphilis: the ulcer is at first painless and may be between or on the labia or on the penis.
- Secondary syphilis: multiple, painless ulcers on the penis or vulva.
- Genital Herpes: small, multiple, usually painful blisters, vesicles, or ulcers. Often recurrent.
- Granuloma inguinale: an irregular ulcer which increases in size and may cover a large area.
- Chancroid: multiple, large, irregular ulcers with enlarged painful suppurating lymph nodes.
Management:
Prompt treatment is important due to the increased risk of HIV transmission associated with genital ulcers.
Treatment strategies for both genders should align with the local epidemiology. In Uganda, the following approach is recommended:
- Non-vesicular Ulcers: Treatment according to the provided flow chart, distinguishing between specific etiologies.
- Vesicular Ulcers: Given the increased risk of HIV transmission, treatment for genital herpes is strongly recommended.

Management Protocol for Genital Ulcer Syndrome:
Multiple Painful Blisters or Vesicles (Likely Herpes):
- Administer Aciclovir 400 mg every 6 hours for 7 days.
- If RPR (Rapid Plasma Reagin) positive, add Benzathine penicillin 2.4 MU IM single dose (half in each buttock).
- In case of persistent lesions, repeat Acyclovir for an additional 7 days.
All Other Cases:
- Prescribe Ciprofloxacin 500 mg every 12 hours for 3 days.
- Add Benzathine penicillin 2.4 MU IM single dose (half in each buttock).
- For individuals with penicillin allergy, substitute with Erythromycin 500 mg every 6 hours for 14 days.
If Ulcer Persists Beyond 10 Days and Partner Was Treated:
- Add Erythromycin 500 mg every 6 hours for 7 days.
If Ulcer Still Persists:
- Refer the individual for specialist management.
Important Notes:
- A negative RPR does not exclude early syphilis.
- Genital ulcers may appear with enlarged and
- fluctuating inguinal lymph nodes (buboes). Do not incise buboes.
Other Components of STI Case Management:
In addition to antimicrobial therapy, comprehensive STI case management includes:
- Partner Notification and Treatment: Partners should be notified and treated, irrespective of symptoms.
- Preventive Measures: Emphasize preventive measures, including safe sexual practices and condom use.
- Health Education: Counsel and educate all clients on:
- The importance of treatment compliance and regular follow-ups.
- Condom use and provide condoms.
- Partner management.
- Offer or refer for HIV VCT services if necessary.
- Schedule a return visit if feasible.
- Abstaining from sex symptoms resolve.