Table of Contents
TogglePneumonia
Pneumonia is an inflammation of the lung parenchyma characterized by cough, tachypnea and dyspnea.
The causative agent usually various microorganisms, including bacteria, mycobacteria, fungi, and viruses are introduced into the lungs through inhalation or from the blood stream.

Causes of Pneumonia
- Bacterial ; streptococcus pneumoniae, haemophilus influenzae ,mycoplasma pneumoniae, staphylococcus aureus, pseudomonas aeruginosa, klebsiella pneumoniae, Moraxella catarrhalis and legionella spp.
- Viral; respiratory syncytial viruses, Influenza A and B, adeno viruses, parainfluenza virus etc.
- Fungal; Histoplasma capsulatum, coccidioides immitis, pneumocystis jirovecii or cryptococcus neoformans.
Classifications of Pneumonia.
Classification is according to;
- Etiology
- Anatomical
- Duration
- Clinical grounds
1. Etiologic classification
- Infective pneumonia:
–Viral pneumonia e.g Influenza A virus –Bacterial pneumonia e.g S. Pneumonia –Fungal pneumonia -Tuberculous pneumonia e.g M.TB
- Non Infective pneumonia: causes; –Toxins –Chemicals e.g. paraffin and vomitus –Radiotherapy –Allergic mechanisms
2. Anatomical
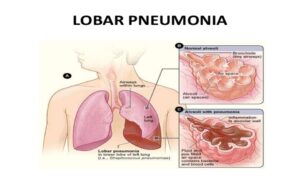
- Lobar pneumonia – Inflammation is localized on one or more lung lobes
- Bronchopneumonia – Pneumonia with inflammation of bronchi and bronchioles –Inflammation is diffuse and primarily affects lobules of the lung.
- Interstitial pneumonia – Pneumonia with inflammation of the lung interstitial tissue.
3. Duration
- Acute pneumonia: Type of pneumonia that lasts only for a few days to and not more than two weeks.
- Chronic Pneumonia: –Lasts for more than two weeks. –Common in Immune Suppressed patients – TB is most common.
4. Clinical Grounds
Pneumonia is classified as:
1. Community-acquired pneumonia (CAP):
- CAP occurs either in the community setting or within the first 48 hours after hospitalization. The causative agents include streptococcus pneumoniae, H. influenza, Legionella, and Pseudomonas aeruginosa.
- Pneumonia is the most common cause of CAP in people younger than 60 years of age.
- Viruses are the most common cause of pneumonia in infants and children.
2. Hospital acquired (Nosocomial pneumonia):
- Hospital Acquired Pneumonia is also called nosocomial pneumonia and is defined as the onset of pneumonia symptoms more than 48 hours after admission in patients with no evidence of infection at the time of admission.
- HAP is the most harmful nosocomial infection and the leading cause of death in patients with such infections.
- Common microorganisms that are responsible for HAP include Enterobacter species, Escherichia coli, influenza, Klebsiella species, Proteus, Serratia marcescens, S. aureus, and S. pneumonia.
3. Aspiration pneumonia:
- Aspiration pneumonia refers to the pulmonary consequences resulting from entry of endogenous or exogenous substances into the lower airway.
- The most common form of aspiration pneumonia is a bacterial infection from aspiration of bacteria that normally reside in the upper airways.
- Aspiration pneumonia may occur in the community or hospital setting.
- Common pathogens are S. pneumonia, H.influenza, andS. aureus.
4. Pneumonia in immunocompromised patients
- Pneumonia in immunocompromised patients includes Pneumocystis pneumonia, fungal pneumonias and Mycobacterium tuberculosis.
- Patients who are immunocompromised commonly develop pneumonia from organisms of low virulence.
- Pneumonia in immunocompromised patients may be caused by the organisms also observed in HAP and CAP.
5. Primary or secondary pneumonia
- Primary pneumonia: Type that occurs in a previously healthy persons living in community. Its usually lobar pneumonia due to strep pneumoniae.
- Secondary pneumonia
- Develops in after;
- History of prior respiratory disease
- Immunocompromised e.g. AIDs patients
- Surgical operation thus in post-operative patientts
Pathophysiology of Pneumonia
- When the infective agents reach the alveoli , they adhere to the walls of bronchi and bronchioles
- They multiply extracellularly , trigger inflammation and pouring of exudates into the air spaces.
- WBCs migrates to alveoli, the alveoli become more thick due to filling with exudates (consolidation).
- Due to inflammation, involved areas are not adequately ventilated, due to increased secretions and edema.
- This will lead to partial occlusion of alveoli and bronchi causing a decrease in alveolar oxygen content.
- Venous blood from the affected areas thus returns to the heart without being oxygenated.
- This will lead to arterial hypoxemia and even death due to interference with gas exchange.
Clinical Features of Pneumonia
- Fever with chills (Temperature 38-39◦c)
- Cough (may be absent in neonates and infants) with sputum production in older children
- Fast breathing (Tachypnea)
- Nasal flaring (with inspiration, the side of the nostrils flares outwards)
- Chest indrawing ( it is inward movement of the lower chest wall when the child is breathes in)
- Altered consciousness
- Irritability
- Shortness of breath
- Grunting respirations
- Chest in-drawing
- Stridor
- Wheezing
- Crackles
- Decreased breath sounds
Diagnosis and Investigations
- History taking. The diagnosis of pneumonia is made through history taking, particularly a recent respiratory tract infection.
- Physical examination. Mainly, the number of breaths per minute and breath sounds is assessed during physical examination.
- Chest x-ray. Identifies structural distribution (e.g., lobar, bronchial); may also reveal multiple abscesses/infiltrates, empyema (staphylococcus); scattered or localized infiltration (bacterial); or diffuse/extensive nodular infiltrates (more often viral). In mycoplasma pneumonia, chest x-ray may be clear.

- Arterial Blood Gas/pulse oximetry. Abnormalities may be present, depending on extent of lung involvement and underlying lung disease.
- Gram stain/cultures. Sputum collection; needle aspiration of empyema, pleural, and transtracheal or transthoracic fluids; lung biopsies and blood cultures may be done to recover causative organism. More than one type of organism may be present; common bacteria include Diplococcus pneumoniae, Staphylococcus aureus, a-hemolytic streptococcus, Haemophilus influenzae; cytomegalovirus (CMV). Note: Sputum cultures may not identify all offending organisms. Blood cultures may show transient bacteremia.
- CBC. Leukocytosis usually present, although a low white blood cell (WBC) count may be present in viral infection, immunosuppressed conditions such as AIDS, and overwhelming bacterial pneumonia. Erythrocyte sedimentation rate (ESR) is elevated.
- Serologic studies, e.g., viral or Legionella titers, cold agglutinins. Assist in differential diagnosis of specific organism.
- Pulmonary function studies. Volumes may be decreased (congestion and alveolar collapse); airway pressure may be increased and compliance decreased. Shunting is present (hypoxemia).
- Electrolytes. Sodium and chloride levels may be low.
- Bilirubin. May be increased.
Management of Pneumonia
- Although viruses are major causes of pneumonia in infants and young children, pneumonia should always be considered potentially bacterial and patient treated with antibiotics.
- Prompt treatment with appropriate antibiotics e.g.
- Amoxicillin is the antibiotic of first choice in children with no serious pneumonia. In infants under 2 months with severe pneumonia, the first line treatment is a combination of ampicillin (150-200mg/kg/day in divided doses) plus gentamycin (5-6 mg/kg/day) intravenously for 10 days. If penicillin is not available, alternative may be cefotaxime. If child condition does not improve, add cloxacillin.
- For older children 2 months to 5 years, ceftriaxone is first line treatment or ampicillin plus gentamycin.
- Fever is treated with paracetamol. Tepid sponging when necessary.
- Nurse patient in semi-sitting up position of head elevated to aid breathing.
- In neonates, clear the airway or nasal irrigation with sodium chloride 0.9%
- Monitoring for increased respiratory distress
- Assist the patient to cough if unable clear the airway by suction
- Administer broncho-dilators
- Oxygen therapy where cyanosis has occurred.
- Fluid- Promote adequate rehydration. In children with severe respiratory difficulty, place and i.v. line and give 70% of normal maintenance fluids. Resume oral fluids as soon as possible.
- Well balanced nutrition, may be via NGT. In the absence of severe respiratory difficulty breastfeed on demand.
- Observations of respiratory rate, temperature, and pulse rate.
- Hygiene: This should be maintained.
- Keep the patient warm and dry. Change position of the patient where indicated.
- Physiotherapy: Chest exercises may be done.
Complications of Pneumonia
- Bacteria in blood stream( bacteremia)/ sepsis
- Lung abscesses
- Empyema
- Pleural effusion
- Obstructive airway secretion
- Shock and respiratory failure
- Necrotizing pneumonia
- Chronic lung disease
Nursing Diagnosis
- Impaired tissue oxygenation related to inflammatory process in airway passages evidenced by cyanosis
- Extreme anxiety related to the frequent life threatening asthmatic attacks evidenced by patient asking many questions
- Impaired breathing patterns related to inflammatory process in the lungs evidenced by use of accessory muscles/wheezing.
- Altered body temperature related to inflammatory process in the lungs evidenced by a high thermometer reading.
- Ineffective airway clearance related to copious tracheobronchial secretions.
- Risk for deficient fluid volume related to fever and a rapid respiratory rate.


Very precise thanks
Thanks
I love it