ATYPICAL ANTIPSYCHOTIC
Atypical or second generation or novel
Atypical or ‘2nd generation’. These medications have been used since the 1990s. These are newer types of antipsychotics.
- These are sometimes referred to as ‘atypicals’
These are newer antipsychotic drugs on the Ugandan market and are less commonly used because they are expensive. They are however the best antipsychotics because they control both negative and positive symptoms of schizophrenia. These drugs are also associated with fewer side effects compared to the typical antipsychotics. Are also called new antipsychotic drugs.
- Some are also less likely to cause sexual side effects compared to first generation antipsychotics.
But second generation antipsychotics may be more likely to cause serious metabolic side effects. This may include rapid weight gain and changes to blood sugar levels, diabetes mellitus, hypercholesterolemia.
Mechanism of Action
- They block 5-HT2A-receptors with lesser degree of antagonism of D2-receptor.
- Have efficacy against negative effects especially clozapine
- As a result, they have fewer extrapyramidal adverse effects than the older traditional agents.
- Atypical agents are serotonin-dopamine 2 antagonists (SDAS)
- They are considered atypical in the way they affect dopamine and serotonin neurotransmission in the four key dopamine path way in the brain.
Classes of Atypical Antipsychotics
- Benzoxazoles- Risperidone
- Dibenzodiazepines – Clozapine
- Thienobenzodiazepine- Olanzapine
- Dibenzothiazepine- Quetiapine
- Imidazolidinone – Sertindole
Risperidone (Risperdal)
- Available in regular tabs, I.M depot form and rapidly dissolving tablet.
- Functions more like atypical antipsychotic at doses greater than 6 mg.
- Increased extra pyramidal side effects (dose dependent)
- Most likely atypical to induce hyperprolactinemia.
- Weight gain and sedation (dose dependent)
- Hypotension, fatigue, abdominal pain, nausea.
Olanzapine (Zyprexa)
- Available in regular tabs, immediate release I.M, rapidly dissolving tab, depot form. Dose 5mg-20mg/ day-OD /nocte.
Side effects
- Sedation, weight gain, hypotension, anti cholinergic effects, changes in liver function tests.
Quetiapine (Seroquel)
- Available in a regular tablet form only.
- Dose: 100-400mg bid or DDD
Side effects
- Weight gain,
- Most likely to cause orthostatic hypotension
- Increase blood sugar-diabetes
Clozapine (Clozaril)
Available in one form-a regular tablet
- Dose: 100-900mg bid or in DDD
Side effects
- Sedation , weight gain
- Hyper salivation
SIDE EFFECTS OF ANTI-PSYCHOTICS:
Extra pyramidal side effects:
Most of the anti-psychotic drugs may cause the imbalance of the neurotransmitters (excitatory and inhibitory) resulting into side effects known as extra pyramidal.
- Acute dystonia– uncontrolled muscular spasm. Muscle from spasm many part of the body, for example:
- Oculogyric: crisis-eyes rolling upwards.
- Torticollis: head and neck twisted to the side
The patient may be unable to swallow or speak clearly. in extreme cases , the back may arch or the jaw dislocate.
Management:
- Give artane tablets or anticholinergic drugs given orally, I.M or I.V depending on the severity of symptoms.
- Benzodiazepines like diazepam.
- Some times change in medication, or lowering dose.
- Parkinsonian symptoms (pseudo-parkinsonism)
- Tremor
- Rigidity
- Bradykinesia: decreased facial expression, flat monotone voice, slow body movements, inability to initiate movement.
- Mask like face
- Bradyphrenia
- Slowed thinking
- Salivation
- Drooping posture.
Management
- Reduce the antipsychotic dose.
- Change to atypical drug (as antipsychotic monotherapy)
- Prescribe an anticholinergic like Artane.
- Akathisia (restlessness); A subjectively unpleasant state of inner restlessness where there is a strong desire or compulsion to move.
- Foot stamping when seated.
- Constantly crossing or uncrossing legs.
- Rocking from foot to foot.
- Constantly pacing up and down.
Management
- Reduce or lower the antipsychotic dose.
- Give benzodiazepines like diazepam
- Give beta blockers like propranolol
- Give an anti cholinergic like artane.
- Tardive dyskinesia (abnormal movement): It is an irreversible extrapyramidal syndrome usually common in patients who have been on anti-psychotics for long. It is characterized by persistent involuntary movement of all oral facial muscles.
- Rabbit syndrome: lip smacking or chewing type movement as of a rabbit.
- Tongue protrusion: fly catching.
- Choreiform hand movements (pill rolling or piano playing)
Severe orofacial movement can lead to difficulty, speaking, eating, or breathing. Movements are worse when under stress.
Management:
- Stop anti-cholinergic if prescribed
- Reduce dose of anti psychotic.
- Change to a typical drug.
- Neuroleptic malignant syndrome: It is rare but fatal (life threatening), occurs as a result of prolonged intake of anti psychotic drugs it is characterized by:
- Severe mental, motor and autonomic disturbance.
- Hyper tonicity increased muscle tone. There is an increased reflex to stimuli.
- Generalized stiffness of the muscles affecting i.e. patient may find it unable to swallow.
- Hyperpyrexia increased body temperature, because of that, they get profuse sweating, this leads to fast dehydration
- There is increased blood pressure leading to tachycardia.
The mortality rate is 20 % as per global population. They need intensive medical and nursing.
For the above extra-pyramidal side effects, we use the following drugs to counter act them.
- Benzhexol (artane)
We can use 2mg-4mg o.d /bid 4-5 days and then go back to PRN when acute. But otherwise, they are supposed to be given when necessary. It is under the group of anti-cholinergic drugs under the classification of drugs.
- Benztropine mosylate (congetin)
It also falls under the group of anti-cholinergic.
Dose: 0.5-1mg to 4mg maximum o.d / PRN (orally)
Injection: 1mg-2mg to I.m-PRN.
N.B: Children below 5yrs should not be given chlorpromazine (Largactil). Use haloperidol.
Other side effects as per systems.
Gastro intestinal tract(GIT)
- Dry mouth: Management: Rinsing of mouth with water (avoid candy ‘’sweetie’’ as carriers may result).
- Excessive salvation (sialorrhea): management give antiparkinsonian like artane or stop drug.
- Constipation: management: give high fibred diet, laxatives like bisacodyl
- Sedation: management: give smaller dose in the morning some patients can only cope with single night-time dosing. Reduce dose if necessary.
Cardio vascular system:
- Postural hypotension (orthostatic hypotension): Management: advise patient to take time when standing up or change posture gradually. Reduce dose or slow down rate of increase
- Cardiac arrhythmias (ECG changes): Management: ECG monitoring, change drug.
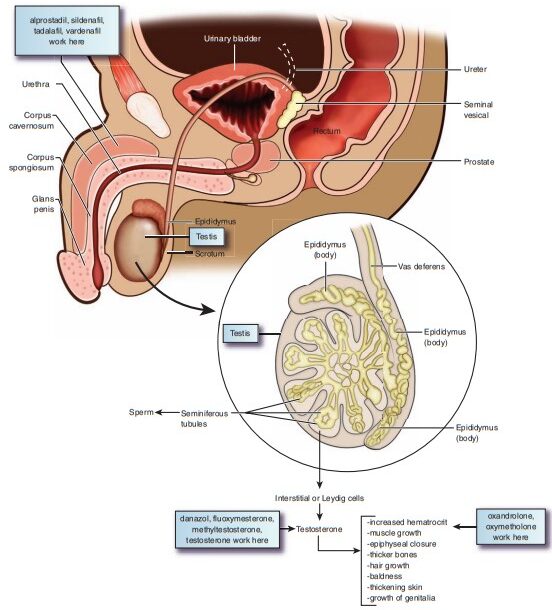
Endocrine and metabolic system:
- Weight gain: Management: dietary control, exercise, change drug.
- Galactorrhea (increased lactation): Management: change the drug
- Amenorrhea: Management: change the drug.
- Decreased libido: Management: reduce dose or change drug.
Haemotological.
- Bone marrow depression.
- Obstructive jaundice.
Ocular
- Blurred vision
- Glaucoma- increased intraocular pressure
- Retina pigmentation (may lead to blindness)
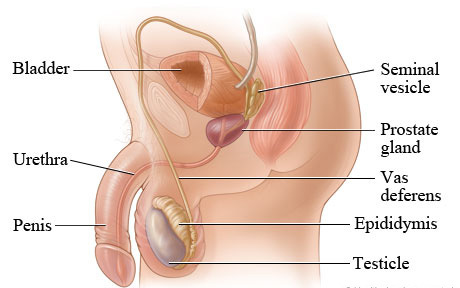
Genital and urinary systems.
- Retention of urine-people can retain or pass urine
- Polyuria- excessive passage of urine of low specific gravity.
- Impotence.
Allergic.
- Photo sensitivity.
- Skin pigmentation.
- Nasal congestion (thioridazine)
NURSE’S RESPONSIBILITY FOR A PATIENT RECEIVING ANTIPSYCHOTICS
- Instruct patients the patient to take sips of water frequently to relieve dryness of mouth. Frequent mouth washes, use of chewing gum, applying glycerine on the lips are also helpful.
- A higher fiber diet, increased fluid intake and laxatives if needed, help to reduce constipation.
- Advise the patient to get up from the bed or chair slowly. Patient should sit on the edge of the bed for one full minute dangling his feet before standing up. Check BP before and after medication is given. This is an important measure to measure to prevent falls and other complications resulting from orthostatic hypotension.
- Differentiate between akathisia and agitation and inform the physician. A change of drug may be necessary if side effects are severe. Administer antiparkinsonian drugs as prescribed
- Observe the patient regularly for abnormal movements
- Take all seizure precautions.
- Patient should be warned about driving a car or operating machinery when first treated with antipsychotics. Giving the entire dose at bedtime usually eliminates any problem from sedation.
- Advise the patient to use sunscreen measures (use of full sleeves, dark glasses etc) for photosensitive reactions.
- Teach the importance of drug compliance, side-effects of drugs and reporting if too severe, and regular follow ups. Give reassurance and reduce unfounded fears and anxieties.
- Seizure precautions should also be taken as clozapine reduces seizure threshold. The dose should be regulated carefully and the patient may also be put on anticonvulsants such as carbamazepine.
ATYPICAL ANTIPSYCHOTIC Read More »