Estrogen Receptor Modulators
Estrogen Receptor Modulators
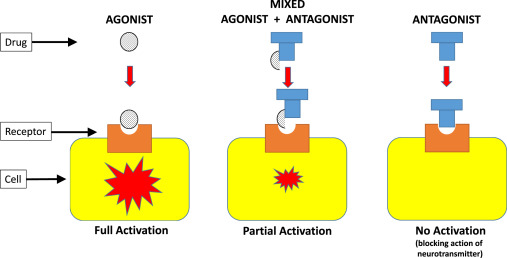
Estrogen Receptor Modulators are agents that either stimulate or block specific estrogen receptor sites.
They are used to stimulate specific estrogen receptors to achieve therapeutic effects of increased bone mass without stimulating the endometrium and causing other less desirable effects i.e. these drugs stimulate the estrogen receptors in the body so as to produce estrogen as needed by the body.
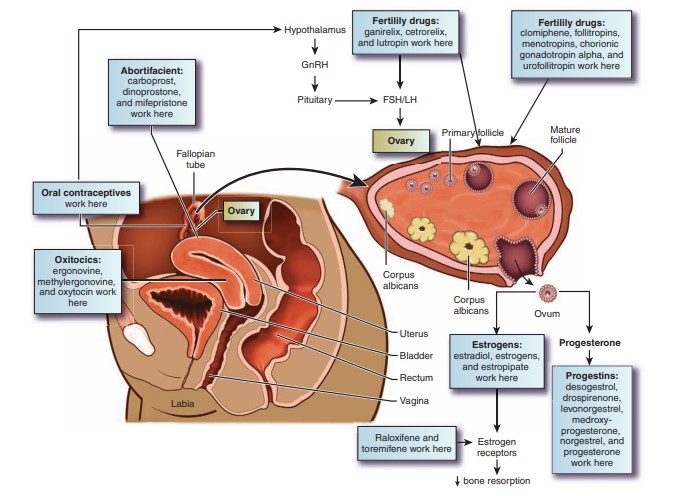
Raloxifene
Dose : 60 mg/day Orally.
Indications : –Used therapeutically to stimulate specific estrogen receptor sites, which results in an increase in bone mineral density without stimulating the endometrium in women; – reduces risk of invasive breast cancer in postmenopausal women with osteoporosis who are at
high risk for invasive breast cancer
Toremifene
Dose : 60 mg/day orally until disease progression occurs.
Indications: Used as an antineoplastic agent because of its effects on estrogen receptor sites for treatment of advanced breast cancer in postmenopausal women with estrogen receptor–positive and estrogen
receptor–unknown tumors
Contraindications of Estrogen Receptor Modulators
- Allergy to estrogen receptor modulators.
- Contraindicated in pregnancy and lactation because of potential effects on the fetus or neonate.
- History of venous thrombosis or smoking. Increased risk of blood clot formation if smoking and estrogen are combined.
Adverse Effects of Estrogen Receptor Modulators
- Raloxifene has been associated with GI upset, nausea, and vomiting.
- Changes in fluid balance may cause headache, dizziness, visual changes, and mental changes.
- Specific estrogen receptor stimulation may cause hot flashes, skin rash, edema, and vaginal bleeding.
Clinically Important Drug–Drug Interactions
- Cholestyramine: reduced raloxifene absorption
- Highly protein-bound drugs (e.g. diazepam, ibuprofen, indomethacin, naproxen): interference on binding sites
- Warfarin: decreased prothrombin time if taken with raloxifene
Nursing Considerations
- Assess for the mentioned cautions and contraindications (e.g. drug allergies, cardiovascular diseases, metabolic bone disease, history of thromboembolism, etc.) to prevent any complications.
- Perform a thorough physical assessment (e.g. bowel sounds, skin assessment, vital signs, mental status, etc.) to establish baseline data before drug therapy begins, to determine effectiveness of
therapy, and to evaluate for occurrence of any adverse effects associated with drug therapy. - Assist with pelvic and breast examinations. Ensure specimen collection for Pap smear and obtain a history of patient’s menstrual cycle to provide baseline data and to monitor for any adverse
effects that could occur. - Arrange for ophthalmic examination especially for patients who are wearing contact lenses because hormonal changes can alter the fluid in the eye and curvature of the cornea, which can
change the fit of contact lenses and alter visual acuity. - Monitor laboratory test results (e.g. urinalysis, renal and hepatic function tests, etc.) to determine possible need for a reduction in dose and evaluate for toxicity.
Nursing Diagnoses
- Ineffective tissue perfusion related to changes in the blood vessels brought about by drug therapy and risk of thromboemboli
- Excess fluid volume related to fluid retention
- Acute pain related to systemic side effects of gastrointestinal (GI) pain and headache
Implementation with Rationale
These are vital nursing interventions done in patients who are taking female sex hormones and estrogen receptor modulators:
- Administer drug with food to prevent GI upset.
- Provide analgesic for relief of headache as appropriate.
- Provide small, frequent meals to assist with nausea and vomiting.
- Monitor for swelling and changes in vision or fit of contact lenses to monitor for fluid retention and fluid changes.
- Provide comfort measures to help patient tolerate drug effects.
- Provide safety measures (e.g. adequate lighting, raised side rails, etc.) to prevent injuries.
- Educate client on drug therapy to promote understanding and compliance.
Evaluation
Here are aspects of care that should be evaluated to determine effectiveness of drug therapy:
- Monitor patient response to therapy (palliation of signs and symptoms of menopause, prevention of pregnancy, decreased risk factors for coronary artery disease, and palliation of certain cancers).
- Monitor for adverse effects (e.g. GI upset, edema, changes in secondary sex characteristics, headaches, thromboembolic episodes, and breakthrough bleeding).
- Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to watch for.
- Monitor patient compliance to drug therapy
Estrogen Receptor Modulators Read More »