HAEMORRHAGE: Nursing Lecture Notes
HAEMORRHAGE: Nursing Lecture Notes
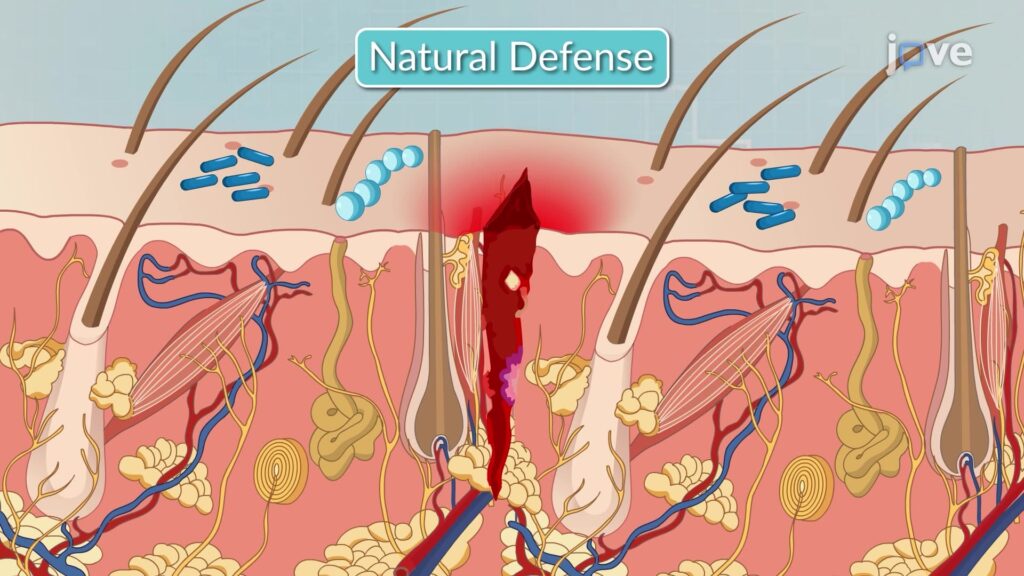
Haemorrhage, commonly known as bleeding, is the loss of blood from the circulatory system, specifically from blood vessels. It is a critical medical condition that, if uncontrolled, can lead to severe physiological compromise and death. The body possesses intrinsic defence mechanisms, primarily through the process of clotting (hemostasis), to prevent excessive blood leakage. However, these mechanisms can be deficient due to underlying diseases, absence of essential clotting factors, or the use of anticoagulant medications.
Types of Haemorrhage
Haemorrhage is classified based on several key characteristics to aid in diagnosis, prognosis, and management. These classifications include:
- The type of blood vessel involved.
- The location or situation of the haemorrhage.
- The time of occurrence or duration of the haemorrhage.
Classification by Blood Vessels Involved
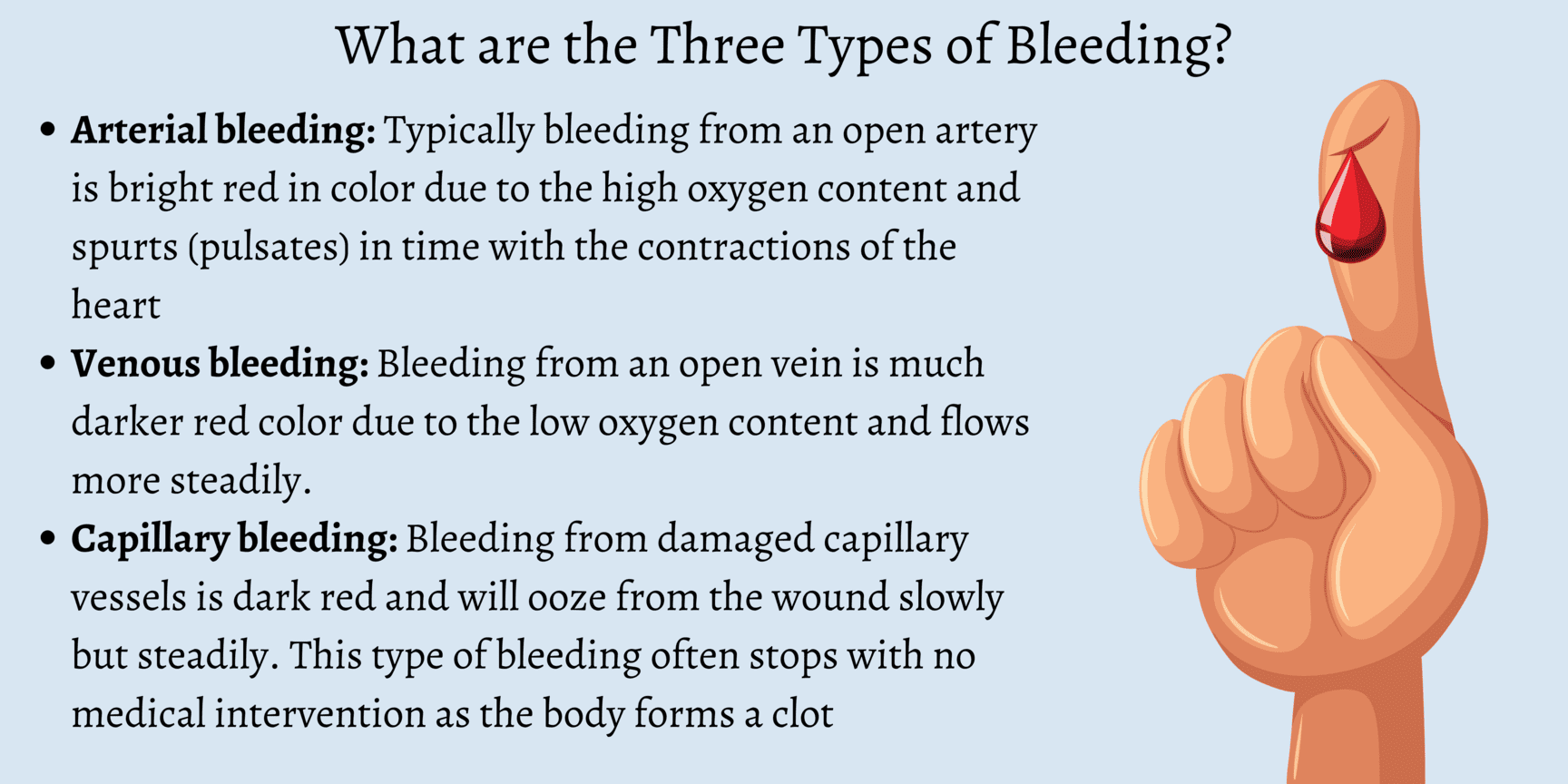
The characteristics of bleeding often provide clues as to which type of blood vessel has been compromised:
1. Arterial Haemorrhage:Classification by Time or Duration of Haemorrhage
The timing of haemorrhage relative to an injury or surgical procedure provides important diagnostic and prognostic information:
1. Primary Haemorrhage:- Increased intravascular pressure due to actions such as coughing or vomiting.
- Increased venous pressure.
- Physical excitement or administration of stimulant drugs.
- Sepsis: Bacterial infection leading to inflammation and enzymatic destruction of vessel walls.
- Enzymatic Action: For example, the action of pepsin on a bleeding peptic ulcer, eroding the vessel.
- Mechanical Pressure: Persistent pressure from a drainage tube or foreign body (e.g., bone fragment) eroding a vessel.
- Presence of Carcinoma: Malignant tumors can erode blood vessels, leading to chronic or acute bleeding.
Classification by Situation or Location of Haemorrhage
This classification distinguishes whether the blood loss is visible externally or contained within body cavities:
1. External or Revealed Haemorrhage:- Definition: This is bleeding that is directly visible, either from an open wound on the body surface or from a natural body orifice (e.g., epistaxis from the nose, hematemesis from vomiting blood, melena/hematochezia from the rectum).
- Visibility: Blood is immediately apparent and can be quantified relatively easily.
- Definition: This refers to bleeding that occurs into an internal body cavity or tissue space, where the blood loss is not immediately visible externally.
- Locations: Common sites include the peritoneal cavity (e.g., ruptured spleen), pleural cavity (e.g., hemothorax), retroperitoneal space, lumen of hollow organs (e.g., intestines, stomach, bladder), or within the tissues of a limb (e.g., large hematoma).
- Diagnosis: Since the bleeding is concealed, diagnosis relies heavily on the patient's symptoms and signs of hypovolemia and shock. It may be "revealed" later if the blood exits the body (e.g., vomited blood, blood passed per rectum) or by the formation of bruising and swelling on the surface of the body.
Clinical Picture: Signs and Symptoms of Haemorrhage
The clinical presentation of haemorrhage varies depending on the amount, rate, and duration of blood loss. Symptoms and signs reflect the body's compensatory mechanisms attempting to maintain vital organ perfusion, followed by the failure of these mechanisms as blood loss becomes severe. The progression is often categorized into stages of shock.
Early Symptoms and Signs (Compensatory Stage / Class I & II Haemorrhage)
These signs indicate the body's initial attempts to compensate for blood loss (up to 15-30% of blood volume). The sympathetic nervous system is activated.
Neurological/Mental Status:- Restlessness and Anxiety: Often one of the earliest signs, resulting from cerebral hypoperfusion and increased catecholamine release.
- Increased Thirst: Due to fluid shifts and activation of the renin-angiotensin-aldosterone system.
- Slightly Increased Pulse Rate (Mild Tachycardia): The heart beats faster to maintain cardiac output despite reduced blood volume.
- Blood Pressure (BP) Maintained or Slightly Lowered: Due to peripheral vasoconstriction attempting to shunt blood to vital organs. Orthostatic hypotension may be present.
- Pallor (Paleness): Due to vasoconstriction and reduced blood flow to the skin.
- Coldness: Skin feels cool to the touch (subnormal temperature, e.g., 36.9°C), also due to peripheral vasoconstriction.
- Slightly Clammy Skin: Due to increased sweating from sympathetic activation.
- Oliguria (Reduced Urine Output): The kidneys conserve fluid and blood flow is shunted away from them.
Symptoms and Signs of Severe Haemorrhage (Decompensatory & Irreversible Stages / Class III & IV Haemorrhage)
These signs manifest when compensatory mechanisms are overwhelmed, and blood loss exceeds 30-40% of total blood volume. This leads to profound organ hypoperfusion and cellular dysfunction.
Neurological/Mental Status:- Lethargy, Drowsiness, Confusion: Progressive worsening of cerebral hypoperfusion.
- Decreased Responsiveness: Leading to stupor and eventually coma.
- Blindness, Tinnitus (Buzzing in the Ears): Severe cerebral ischemia.
- Extreme Pallor: Face becomes ashen white, indicating severe cutaneous vasoconstriction and lack of circulating blood.
- Profound Coldness: Core body temperature may drop significantly (e.g., 36°C or lower), indicating severe hypothermia and circulatory collapse.
- Pulse: Very rapid in rate (severe tachycardia, >120 bpm), thready in volume (barely palpable), and often irregular in rhythm, indicating a severely compromised cardiac output.
- Blood Pressure: Extremely low (severe hypotension), indicating failed compensation and impending circulatory collapse.
- Low Venous Pressure: Due to severely depleted intravascular volume.
- Air Hunger: The patient gasps for breath, with respirations becoming rapid and sighing (Kussmaul-like breathing), as the body attempts to compensate for metabolic acidosis resulting from anaerobic metabolism.
- Dyspnea: Difficult or labored breathing.
- Diminished Urine Volume: Progressing to anuria (no urine production), which may result in acute renal failure due to prolonged renal ischemia.
- Extreme Thirst: Persists and worsens.
- Metabolic Acidosis: Due to widespread anaerobic metabolism and lactic acid accumulation.
- Eventual Multi-Organ Dysfunction Syndrome (MODS): Leading to irreversible organ damage and death.
Management of Haemorrhage: Principles of Care
Effective management of haemorrhage is time-sensitive and aims to stop the bleeding, restore circulating blood volume, optimize tissue perfusion, and treat any underlying coagulopathy.
Immediate Priorities (The "ABCDE" Approach):
- Airway: Ensure a patent airway. If the patient's consciousness is compromised, intubation may be necessary to protect the airway and facilitate ventilation.
- Breathing: Assess respiratory effort and oxygenation. Administer high-flow oxygen (e.g., via non-rebreather mask) to maximize oxygen delivery to tissues. Provide ventilatory support if needed.
- Circulation: This is paramount in haemorrhage.
- Direct Pressure: Apply direct pressure to any visible external bleeding site.
- Large-Bore IV Access: Establish at least two large-bore intravenous (IV) lines for rapid fluid and blood product administration.
- Fluid Resuscitation: Begin rapid infusion of crystalloid solutions (e.g., 0.9% Normal Saline, Lactated Ringer's) while awaiting blood products.
- Blood Transfusion: Initiate blood product transfusion (e.g., packed red blood cells, fresh frozen plasma, platelets) as soon as possible, especially for significant haemorrhage. Consider massive transfusion protocols if appropriate.
- Identify and Stop Bleeding: Promptly identify the source of bleeding and take definitive steps to control it (e.g., surgical intervention, endoscopic intervention, interventional radiology embolization, tourniquet for severe limb trauma).
- Disability (Neurological Status): Assess the patient's level of consciousness (e.g., AVPU scale, GCS) to monitor cerebral perfusion.
- Exposure and Environment: Fully expose the patient to identify all injuries and bleeding sites. Prevent hypothermia by covering the patient with warm blankets, as hypothermia exacerbates coagulopathy.
Ongoing Management and Monitoring:
- Continuous Monitoring: Continuously monitor vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation), ECG, and urine output. An arterial line may be used for continuous blood pressure monitoring.
- Laboratory Monitoring: Serial blood tests, including complete blood count (CBC), electrolytes, coagulation profile (PT, PTT, fibrinogen), blood type and cross-match, and lactate levels (to assess tissue perfusion and acidosis).
- Temperature Control: Maintain normothermia; hypothermia can worsen coagulopathy and acidosis.
- Correct Coagulopathy: Administer specific clotting factors, cryoprecipitate, or prothrombin complex concentrates (PCCs) as indicated, especially if the patient is on anticoagulants or has a pre-existing coagulopathy. Consider tranexamic acid (TXA) as an antifibrinolytic.
- Pain Management: Administer analgesia cautiously, considering its potential effects on blood pressure and mental status.
- Prevent Complications: Implement strategies to prevent acute kidney injury, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and multi-organ dysfunction syndrome (MODS).
- Definitive Treatment: Address the underlying cause of the haemorrhage once the patient is stabilized.
Management and Interventions
Effective management of haemorrhage is time-sensitive and requires a multi-faceted approach. The primary goals are to:
- Arrest the haemorrhage: Control and stop the bleeding at its source.
- Restore blood volume: Replenish lost blood and fluids to maintain adequate circulation.
- Manage the extravasated blood: Address the consequences of blood accumulating outside the vessels, and support the body's physiological responses.
I. Arrest of Haemorrhage: Controlling the Bleeding Source
The methods to control bleeding depend on whether the haemorrhage is revealed (external) or concealed (internal).
A. Arrest of Revealed (External) Haemorrhage
Most forms of external haemorrhage can be controlled by applying pressure directly or indirectly to the bleeding site. The choice of method depends on the severity and nature of the bleeding:
Direct Pressure (Pad & Bandage):- Method: This is the simplest, most effective, and often the first line of treatment. Apply a clean, sterile pad directly to the bleeding wound and secure it firmly with a bandage.
- Mechanism: Direct pressure compresses the bleeding vessels, allowing clots to form.
- Advantages: Highly effective, causes minimal damage, and can be performed quickly.
- Method: Fingers are used to apply firm pressure over the pressure point of an artery that supplies the wounded area, proximal to the injury.
- Mechanism: Temporarily occludes the main arterial blood supply to the limb or area.
- Application: Commonly used in areas where direct pressure might be difficult or less effective, such as on the neck (e.g., carotid artery pressure point in severe facial bleeding). It provides temporary control until definitive measures can be taken.
- Method: Raising the injured limb above the level of the heart.
- Mechanism: Reduces hydrostatic pressure in the veins, which can help control venous bleeding.
- Application: A classical method for controlling bleeding from ruptured varicose veins of the leg or other venous injuries.
- Method: A constricting band applied proximally to an injury on a limb. Tourniquets include devices like the Samway anchor, Esmarch’s Elastic bandage, or inflatable cuffs.
- Application: **Use ONLY for the control of heavy, life-threatening bleeding from a limb when other methods have failed or are not feasible.**
- Dangers: If left on for more than 30 minutes, it carries significant risks such as gangrene, nerve damage, and reperfusion injury upon removal. Requires careful application and monitoring.
- Method: Surgically tying off the bleeding vessel with sutures.
- Application: Necessary if bleeding continues despite less invasive measures or for larger vessels.
- Method: Application of heat (via electrical current) to the bleeding point to seal small vessels.
- Application: Commonly used in surgical settings for precise haemostasis.
- Method: Deliberate occlusion of bleeding blood vessels by introducing embolic materials (e.g., coils, particles, glues) through an angiographic catheter under imaging guidance.
- Application: Common in controlling bleeding from internal sources like oesophageal varices, gastric ulcers, or arterial bleeds in inaccessible locations. Examples of emboli include lyophilized human dura mater.
- Method: Insertion of sterile gauze or specialized hemostatic dressings into a wound or cavity to apply internal pressure.
- Application: A temporary measure for very severe bleeding, often used in theatre to control sudden haemorrhage or for diffuse bleeding that is difficult to ligate.
- Method: Substances capable of causing bleeding to stop when applied locally.
- Examples: Include topical thrombin, collagen, gelatin sponges, oxidized regenerated cellulose (Oxycel). Some natural substances like snake venom or adrenaline can also act as styptics.
- Application: Used locally in certain cases for low-pressure bleeding from capillaries and venules.
B. Arrest of Concealed (Internal) Haemorrhage
Controlling internal haemorrhage is more challenging as direct pressure is often not possible. Management focuses on internal pressure, addressing the underlying cause, and enhancing coagulation.
Surgical Ligation/Repair:- Method: Direct surgical intervention to identify and ligate or repair the bleeding vessel.
- Application: Often the definitive treatment for ruptured organs (e.g., ruptured spleen, liver laceration) or major vessel injuries.
- Method: Removing blood clots from a hollow organ can allow it to contract and seal bleeding vessels.
- Application: For severe bleeding from the bladder, passing a catheter and emptying it of clots can help the bladder contract and tamponade bleeding.
- Method: Administration of medications that promote vasoconstriction.
- Examples:
- Adrenaline (Epinephrine): Can be added to saline or sodium bicarbonate for washing out an organ to encourage vessel constriction (e.g., in some urological procedures, often done two-hourly).
- Ergometrine: Used post-partum to stimulate uterine contractions and reduce bleeding after the birth of the placenta.
- Vasopressin (Pitressin): Can be used effectively in the control of bleeding from oesophageal varices by causing splanchnic vasoconstriction.
- Method: Administering agents that correct clotting factor deficiencies.
- Application: Very valuable when the mechanism of clotting is deficient.
- Vitamin K (IM): Important in jaundiced patients or those with liver dysfunction who are bleeding due to impaired synthesis of Vitamin K-dependent clotting factors.
- Factor VIII Concentrate: Indicated in patients with Haemophilia A.
- Fresh Frozen Plasma (FFP), Platelets, Cryoprecipitate: Administered to provide clotting factors or platelets as needed.
- Method: Using specialized materials to provide internal pressure or promote clotting.
- Examples:
- Gauze soaked in adrenaline can be effective in certain sites (e.g., nasal packing for epistaxis).
- Oxycel (oxidized regenerated cellulose), Fibrin glue, or a piece of the patient’s own crushed muscle can be used to promote local haemostasis in surgical beds.
- Method: Systemic antibiotic administration.
- Application: Essential in secondary haemorrhage, especially when caused by infection, to control sepsis which contributes to vessel wall breakdown.
- Method: Applying pressure from within a lumen using an inflatable balloon.
- Application: Applied by the balloon of a triluminal tube (e.g., Sengstaken-Blakemore tube) in bleeding oesophageal varices or by the balloon of a Foley catheter in a post-prostatectomy cavity.
- Method: Use of medications that inhibit the breakdown of blood clots.
- Example: Achieved by the use of Tranexamic Acid (TXA), which stabilizes clots and reduces bleeding in various conditions.
II. Restoration of Blood Volume and Oxygen Carrying Capacity
Replacing lost fluid and blood is crucial to maintain adequate circulation and tissue perfusion.
- Airway: Ensure a patent airway. Intubation may be necessary if consciousness is compromised to protect the airway and facilitate ventilation.
- Breathing: Assess respiratory effort and oxygenation. Administer high-flow oxygen (e.g., via non-rebreather mask) to maximize oxygen delivery to tissues. Provide ventilatory support if needed.
- Circulation: This is paramount.
- Large-Bore IV Access: Establish at least two large-bore intravenous (IV) lines (e.g., 14-16 gauge) for rapid fluid and blood product administration. Central venous access may be needed in severe cases.
- Fluid Resuscitation: Begin rapid infusion of crystalloid solutions (e.g., 0.9% Normal Saline, Lactated Ringer's) as initial volume expanders while awaiting blood products. Monitor response.
- Blood Transfusion: Initiate blood product transfusion (e.g., packed red blood cells to increase oxygen-carrying capacity; fresh frozen plasma for clotting factors; platelets for thrombocytopenia) as soon as possible, especially for significant haemorrhage. Consider massive transfusion protocols (MTP) for severe, ongoing bleeding.
- Disability (Neurological Status): Assess the patient's level of consciousness (e.g., AVPU scale, GCS) to monitor cerebral perfusion and detect neurological changes.
- Exposure and Environment: Fully expose the patient to identify all injuries and bleeding sites. Prevent hypothermia by covering the patient with warm blankets, as hypothermia significantly exacerbates coagulopathy and metabolic acidosis.
- Continuous Monitoring: Continuously monitor vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation), ECG for cardiac rhythm, and hourly urine output via an indwelling urinary catheter (a sensitive indicator of renal perfusion). An arterial line provides continuous and accurate blood pressure monitoring.
- Laboratory Monitoring: Frequent serial blood tests are essential:
- Complete Blood Count (CBC): To monitor hemoglobin and hematocrit.
- Electrolytes and Renal Function Tests: To assess fluid and electrolyte balance and kidney function.
- Coagulation Profile: PT, PTT, fibrinogen to assess clotting status.
- Blood Type and Cross-match: For blood product compatibility.
- Lactate Levels: To assess tissue perfusion and severity of acidosis.
- Arterial Blood Gases (ABGs): For oxygenation, ventilation, and acid-base balance.
- Temperature Control: Actively maintain normothermia using warming blankets and warmed fluids.
- Correct Coagulopathy: Actively manage any identified clotting factor deficiencies by administering specific factor concentrates, cryoprecipitate, or prothrombin complex concentrates (PCCs), especially if the patient is on anticoagulants or has a pre-existing coagulopathy.
A. Nursing Diagnoses for Patients with Haemorrhage (Examples)
Nursing diagnoses are clinical judgments about individual, family, or community responses to actual or potential health problems/life processes. For haemorrhage, they often focus on perfusion, fluid balance, and anxiety.
- Deficient Fluid Volume related to active blood loss, as evidenced by hypotension, tachycardia, decreased urine output, cool/clammy skin, and altered mental status.
- Ineffective Tissue Perfusion (specify: Cerebral, Cardiopulmonary, Renal, Gastrointestinal, Peripheral) related to hypovolemia and decreased oxygen-carrying capacity, as evidenced by altered mental status, oliguria, delayed capillary refill, weak pulses, or abnormal ABGs.
- Decreased Cardiac Output related to reduced preload (due to blood loss), as evidenced by hypotension, tachycardia, and signs of hypoperfusion.
- Risk for Shock related to uncompensated blood loss.
- Anxiety/Fear related to threat to health status, perceived loss of control, and critical illness.
- Risk for Imbalanced Body Temperature (Hypothermia) related to hypovolemia, decreased metabolic rate, and rapid fluid resuscitation.
- Acute Pain related to injury or invasive procedures, as evidenced by patient report, guarding behavior, or vital sign changes.
B. Nursing Interventions for Haemorrhage
Nursing interventions are actions designed to achieve patient outcomes related to the nursing diagnoses. These are broad categories and require specific adaptation based on the individual patient's condition and the type of haemorrhage.
- Prioritize ABCs and Rapid Response:
- Immediately assess and maintain airway patency, breathing effectiveness, and circulation.
- Activate rapid response team/code team according to facility protocol for acute haemorrhage.
- Stay with the patient; do not leave an acutely bleeding patient unattended.
- Control Bleeding (Nursing Actions):
- Apply direct, firm pressure to any external bleeding site using sterile dressings. Elevate the affected limb if appropriate.
- Prepare and assist with tourniquet application if indicated for life-threatening limb haemorrhage (monitor time).
- Prepare for and assist with surgical or interventional radiology procedures for definitive bleeding control.
- Ensure all lines, drains, and tubes are securely in place to prevent accidental dislodgement.
- Fluid and Blood Volume Resuscitation:
- Establish and maintain multiple large-bore IV access sites.
- Administer prescribed IV fluids (crystalloids) and blood products (PRBCs, FFP, platelets) rapidly, using rapid infusers if available, and monitor patient response.
- Monitor for signs of fluid overload or transfusion reactions.
- Ensure warmed fluids and blood products are used to prevent hypothermia.
- Continuous Assessment and Monitoring:
- Monitor vital signs (BP, HR, RR, SpO2, Temp) continuously (e.g., every 5-15 minutes or more frequently in acute phase).
- Assess level of consciousness (LOC) and neurological status frequently for signs of cerebral hypoperfusion.
- Monitor hourly urine output via indwelling catheter; report output less than 0.5 mL/kg/hour.
- Assess skin color, temperature, and capillary refill for signs of peripheral perfusion.
- Monitor dressing for increasing saturation and measure blood loss (e.g., weigh pads, assess drainage in collection devices).
- Review and trend laboratory results (Hgb, Hct, lactate, coagulation studies, electrolytes).
- Assess for signs of internal bleeding if concealed haemorrhage is suspected (e.g., increasing abdominal girth, distension, pain, bruising, changes in bowel sounds, persistent hypotension despite fluid resuscitation).
- Oxygenation and Respiratory Support:
- Administer oxygen as prescribed to maintain SpO2 >94%.
- Monitor respiratory effort and patterns; prepare for ventilatory support if respiratory distress or failure occurs.
- Maintain Normothermia:
- Use warming blankets, warmed IV fluids, and control room temperature to prevent and treat hypothermia.
- Pain and Anxiety Management:
- Administer analgesics as prescribed, carefully monitoring for effects on vital signs.
- Provide emotional support, calm reassurance, and clear, concise explanations to the patient and family. Address their fears and anxiety.
- Create a calm environment as much as possible.
- Prevent Complications:
- Maintain strict asepsis for all invasive procedures (IV insertion, catheter care) to prevent infection.
- Implement measures to prevent pressure injuries due to immobility and hypoperfusion.
- Initiate DVT prophylaxis as soon as appropriate and ordered.
- Monitor for signs of acute kidney injury or multi-organ dysfunction.
- Documentation and Communication:
- Accurately and timely document all assessments, interventions, and patient responses.
- Communicate effectively and frequently with the interdisciplinary team (physicians, respiratory therapists, lab, blood bank) regarding patient status and changes.
- Handover critical information thoroughly.
Special Types and Terms of Haemorrhage
Haemorrhage can manifest in various specific ways depending on its anatomical location, and certain terms are used to describe these particular presentations.
Specific Types of Haemorrhage
These are haemorrhages that are identified by their site of external manifestation or unique characteristics:
Epistaxis (Nosebleed):- Description: Bleeding from the nose.
- Common Causes:
- Injury to the nose (trauma).
- Fracture base of the skull (indicating severe trauma).
- Ulceration of the mucus membrane of the nose (e.g., from dryness, digital manipulation).
- Bleeding disorders (e.g., leukemia, haemophilia).
- Local infections like rhinitis.
- Venous congestion associated with heart diseases (e.g., heart failure).
- Hypertension (high blood pressure).
- Management:
- Initial First Aid: The patient should sit upright, leaning slightly forward (not backward, to prevent blood from flowing down the throat), and firm pressure should be applied to the soft cartilaginous part of the nostrils for 10-15 minutes.
- Sponge the face with cold water or apply a cold compress to the bridge of the nose.
- If bleeding persists, medical attention is required.
- Medical Interventions:
- The nose may be packed with sterile gauze, sometimes impregnated with vasoconstrictors like adrenaline, or specialized nasal packing devices.
- The nasal plug/pack is typically left in situ for 24-48 hours, with careful monitoring due to the risk of infection (sepsis) and potential airway obstruction.
- Recurrent or persistent bleeding may be treated by chemical (e.g., silver nitrate) or electrical (electrocautery) cauterization of the bleeding vessel.
- In severe cases, surgical ligation of feeding arteries or interventional radiology embolization may be necessary.
- Description: This is the coughing up of blood from the respiratory tract (lungs or bronchial tubes). The blood is typically bright red, frothy (mixed with air), and alkaline. It is often mixed with sputum.
- Common Causes:
- Pulmonary diseases (e.g., Tuberculosis (TB), Bronchiectasis, Pneumonia, Lung abscess).
- Lung cancer (bronchogenic carcinoma).
- Benign tumours of the respiratory tract.
- Injury to the lungs or chest (trauma).
- Pulmonary embolism (especially with infarction).
- Venous congestion into the lungs (e.g., severe heart failure, mitral stenosis).
- Blood disorders (e.g., leukemia, coagulopathies).
- Rupture of an aortic aneurysm into a bronchus (rare but life-threatening).
- Foreign body aspiration.
- Management:
- Immediate Action: Severe cases require urgent medical assessment and treatment to secure the airway and control bleeding.
- Patient Care:
- Maintain a calm environment and reassure the patient (care of the mind).
- Position the patient sitting up to aid breathing and prevent aspiration; usually, the bleeding side down if known, to protect the contralateral lung.
- Ensure total rest.
- Frequent mouth washes to remove the taste of blood.
- Provide non-stimulating fluids.
- Keep the patient warm.
- Medical Interventions:
- Collect blood for Hemoglobin (HB) estimation, blood grouping, and cross-matching for potential transfusion.
- Blood transfusion if bleeding is severe and causing hemodynamic instability.
- Administer antitussives (e.g., codeine, morphine) to suppress cough, which can exacerbate bleeding, and to provide sedation.
- Treat the underlying cause (e.g., antibiotics for infection, chemotherapy/radiation for cancer, bronchoscopic intervention).
- Bronchoscopy for localization and intervention (e.g., laser coagulation, balloon tamponade).
- In severe cases, surgical resection may be considered.
- Description: This is vomiting blood from the upper gastrointestinal (GI) tract (esophagus, stomach, or duodenum). The blood may be bright red (indicating active, fresh bleeding) but is more often brown, resembling "coffee grounds" due to the action of gastric acid on hemoglobin. It is acidic.
- Common Causes:
- Peptic ulcers (gastric or duodenal ulcers).
- Acute gastritis (inflammation of the stomach lining, often due to corrosive drugs like NSAIDs/Aspirin, or alcohol taken on an empty stomach).
- Gastric cancer.
- Oesophageal varices (dilated veins in the esophagus, often due to portal hypertension, e.g., in liver cirrhosis).
- Mallory-Weiss tear (tear in the esophageal lining due to forceful vomiting/retching).
- Swallowed blood (e.g., after severe epistaxis or haemoptysis).
- Fracture base of the skull (blood from nasopharynx tracking down).
- Post-operative bleeding after nose and throat surgeries.
- Blood disorders (e.g., leukemia, coagulopathies).
- Management:
- Initial Assessment: Immediate assessment of hemodynamic stability.
- Investigations:
- Collect blood for HB, grouping, and cross-matching.
- Stool for occult blood test.
- Patient Care:
- Ensure absolute rest and quietness.
- Frequent monitoring of vital signs.
- Provide emotional support.
- Medical Interventions:
- Fluid resuscitation and blood transfusion if indicated.
- Administer morphine for pain and sedation as needed, while carefully monitoring respiratory status and vital signs.
- Specific Treatment According to Cause:
- Proton pump inhibitors (PPIs) for ulcers/gastritis.
- Endoscopic intervention (e.g., banding, sclerotherapy for varices; clipping, coagulation for ulcers).
- Surgical intervention for refractory cases or severe bleeds not amenable to endoscopy.
- General nursing care including NPO (nothing by mouth) and monitoring for further bleeding.
- Description: This is the passage of dark, tarry, sticky stools (faeces) with a characteristic foul odor. It results from bleeding in the upper GI tract, where blood has been digested and altered by intestinal bacteria. Usually indicates bleeding from a site high in the GIT (esophagus, stomach, duodenum, or small bowel).
- Common Causes:
- Duodenal ulcers (most common cause).
- Gastric ulcers.
- Gastritis.
- Bleeding from the small bowel.
- Swallowing of a large amount of blood (e.g., from severe epistaxis or haemoptysis).
- Certain medications like iron supplements (can cause dark stools, but not true melaena, which is positive for occult blood) or bismuth subsalicylate.
- Investigation: Stool for occult blood (guaiac test) confirms the presence of blood. Endoscopy is usually required to identify the source.
- Management: As for internal haemorrhage, focusing on hemodynamic stabilization, identifying the source, and definitive treatment (often endoscopic or medical).
- Description: Is the passage of blood in urine, making it appear pink, red, or dark brown/cola-colored. It can be macroscopic (visible to the naked eye) or microscopic (detectable only with urinalysis).
- Common Causes:
- Trauma to the urinary tract (e.g., ruptured kidney, bladder injury).
- Urinary tract infections (UTIs).
- Renal calculi (kidney stones) – often associated with pain.
- Chronic kidney infection (pyelonephritis).
- Tuberculosis (TB) of the kidney.
- Post-operative causes (e.g., prostatectomy, bladder surgery).
- Growths/tumours in the bladder, kidney, or prostate (can be painless haematuria, requiring urgent investigation).
- Leukemia or other blood disorders affecting clotting.
- Inflammation of the urinary tract (e.g., cystitis, glomerulonephritis, bilharzia/schistosomiasis).
- Certain medications (e.g., anticoagulants).
- Management:
- Less Severe Cases: Rest in bed and reassurance, along with treatment of the underlying cause.
- More Severe Cases: If there's significant damage to the bladder or kidneys, or a mass, surgical intervention (e.g., to remove stones, excise tumors, repair trauma) may be indicated.
- Specific treatment varies significantly according to the underlying cause. This may include antibiotics for infection, medical management for kidney disease, or interventional procedures for stones/tumors.
Special Terms for Haemorrhage from Specific Sites/Contexts
These terms describe the location of blood accumulation or specific bleeding patterns:
- Haemothorax: Bleeding into the pleural cavity (space between the lungs and the chest wall). Often due to chest trauma or lung pathology.
- Haemoperitoneum: Bleeding into the peritoneal cavity (abdominal cavity). Often associated with ruptured organs (e.g., spleen, liver) or major vessel injury.
- Haemarthrosis: Bleeding into a joint space. Common in individuals with bleeding disorders like haemophilia or following trauma.
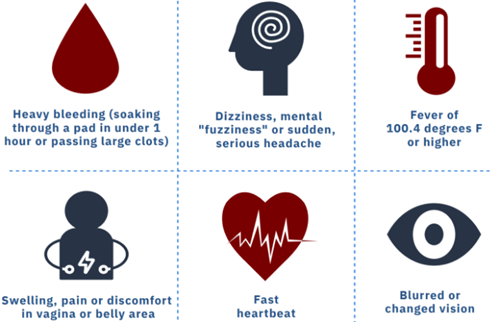
- Menorrhagia: Excessive or prolonged menstrual bleeding at regular intervals.
- Metrorrhagia: Irregular, acyclic uterine bleeding occurring between expected menstrual periods.
- Menometrorrhagia: Prolonged or excessive bleeding occurring at irregular and frequent intervals.
- Haemopericardium: Bleeding into the pericardial sac (the sac surrounding the heart). Can lead to cardiac tamponade, a life-threatening condition.
- Haematomyelia: Bleeding into the spinal cord parenchyma.
- Haematoma: A localized collection of extravasated blood, usually clotted, in an organ, space, or tissue (e.g., a bruise).
- Ecchymosis: A discoloration of the skin resulting from bleeding underneath, typically caused by bruising. Larger than petechiae.
- Petechiae: Small (1-2 mm), pinpoint, non-blanching red or purple spots on the skin caused by minor hemorrhage.
- Purpura: Red or purple discolored spots on the skin that do not blanch on pressure, caused by bleeding underneath the skin. Larger than petechiae but smaller than ecchymoses.
HAEMORRHAGE: Nursing Lecture Notes Read More »
BURNS LECTURE NOTES
BURNS
Burns are injuries to the skin due to extremes of temperature i.e cold or hot, chemicals or radiations. Burns occur when there is injury to the tissues of the body caused by heat, chemicals, electric current or radiations.
Anatomical review of the skin.
- Skin is the largest organ of the body that protects against injury, loss of fluid and from infection.
- It also maintains a constant body temperature with sebum, hair follicles. The skin has got two layers;
- -Epidermis (outer layer) and -Dermis (inner layer).
- Under the skin is sebaceous tissue mainly fat.
- The top part of the skin (epidermis) is made up of fat cells which are constantly shed and are replaced by new cells which come from underneath the layer.
- The epidermis has got an oily layer called sebum produced by sebaceous gland. It prevents heat loss (it thickens when it’s cold).
- Sebum makes the skin water proof, makes skin supplies plethoric.
- The dermis contains blood vessels, nerve, muscles, sweat glands, hair follicles, sebaceous glands; the ends of the sensory nerves in the dermis register sensation from the body surface.
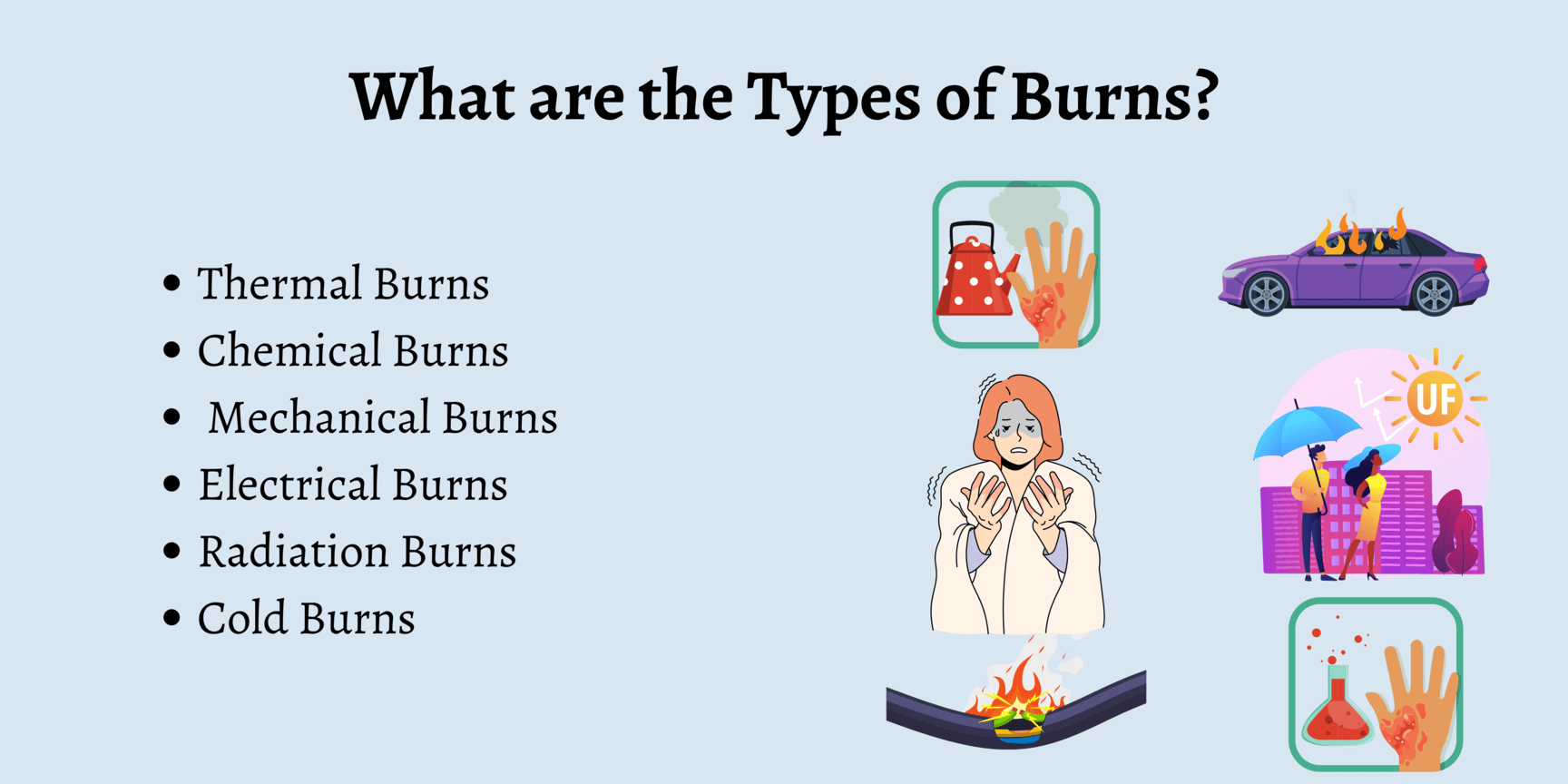
TYPES OF BURNS
Thermal burns
These can be caused by flame, flash, scald, or contact with hot object.
Chemical burns
These are the result of tissue injury and destruction from necrotizing substance. Chemical burns are most commonly caused by acids; however alkalis can also cause a burn e.g. cleaning agents, drain cleaners and lye’s.
Electrical burns
These result from coagulation necrosis that is caused by intense heat generated from an electrical current. It can also result from direct damage to nerves and vessels causing tissue anoxia and death. The severity of the electrical injury depends on the amount of voltage, tissue resistance, current pathways, and surface area in contact with the current and on the length of time the current flow was sustained.
Smoke and inhalation injury
It results from inhalation of hot air or noxious chemicals that can cause damage to the tissues of the respiratory tract. Smoke inhalation injuries are an important determinant of motility in the fire victims.
- Carbon monoxide poisoning.
- Inhalation injury above the glottis, it is thermally produced and above is chemically produced.
- Inhalation injury below the glottis is related to the length of exposure to smoke or toxic fumes.
Cold thermal injury
These are due to extreme cold temperatures e.g. frost bite, freezing metals.
Irradiations
I.e. sun burn, radiation therapy, medical therapy e.g. treatment of cancer of the cervix.
SCALDS
Are injuries caused by moist heat, and hot liquids?
CLASSIFICATION OF BURN INJURY
Burns are classified according to;
- Depth of the burn.
- Extent of the burn.
- Location of the burn.
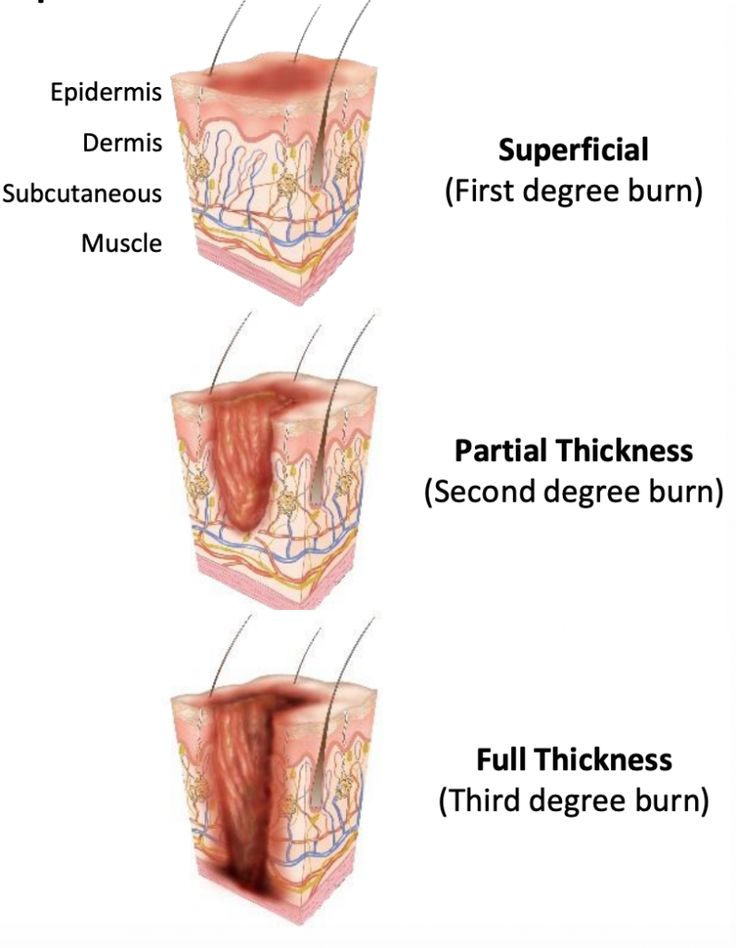
DEPTH OF THE BURN
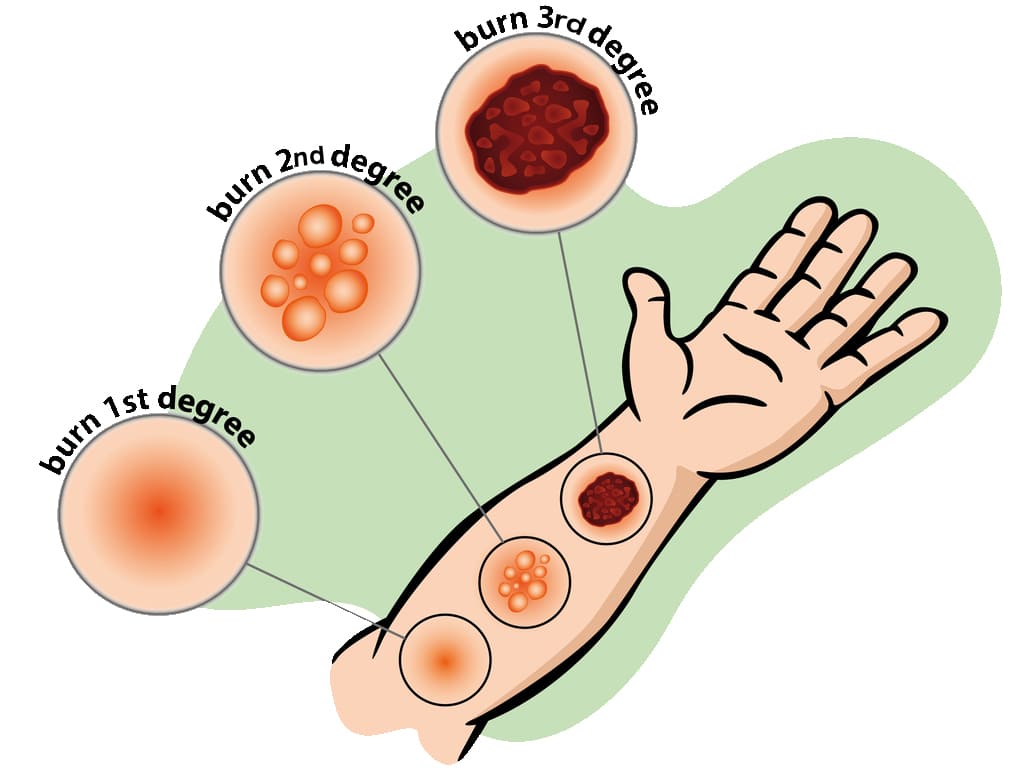
In the past, burns were defined by degrees; first degree, second degree and third degree burns. They now advocate more explicit definition categorizing the burn according to the depth of skin destruction.
- SUPERFICIAL BURNS: Involves only the outer most skin layer. They have redness, swelling, and tenderness. It usually heals well, if first aid is given promptly and if blisters don’t form. Burns from sun, charcoal stove. Are also known as first degree burns.
- PARTIAL THICKNESS BURNS: The damage to epidermis is severe, we almost always have blister formation and very painful. Completely destroys the epidermis. Blisters form because of fluid released from the damaged tissue, usually heal well but may be fatal if more than 30% of skin is involved. Also known as second degree burns.
- FULL THICKNESS/DEEP BURNS: The dermis is involved including other structures like muscles, bones. All layers involved blood vessels, fat and nerves. There is either no pain or minimal. This may mislead that the burns are not severe. You need immediate help; the skin is pale and charred (like toasted meat).
LOCATION OF BURN
- The location of the burn wound is related to the severity of the burn injury. Burns to the face and neck and circumferential burns of the chest may inhibit respiratory function by virtue of mechanical obstruction secondary to edema or scar formation.
- These injuries may also indicate the possibility of inhalation injury and respiratory mucosal damage.
- Burns of the hands, feet, joints, and eyes are of concern because they make self-care very difficult and may jeopardize future function.
- The ears and nose, composed mainly of cartilage, are susceptible to infection because of poor blood supply to the cartilage.
- Burns of buttocks and genitalia are highly susceptible to infection.
- Circumferential burns of the extremities can cause circulatory compromise distal to the burn with subsequent neurologic impairment of the affected extremity.
- Patient may develop compartment syndrome from direct heat damage to the muscles, multiple intravenous access attempts or pre burn vascular problems.
EXTENT OF A BURNT AREA.
Two commonly used guides for determining the total body surface area (TBSA) affected or the extent of a burn wound are the Lund-Browder chart and rule of nines. Only partial thickness burns and full thickness burns are included when calculating the burnt area because it is more accurate. The patient’s age, in proportions to relative body area size, is taken into account. For irregular or odd-shaped burns, the palmar surface of the patient’s hand is considered to be approximately 1% of the TBSA.
USES OF WALLACE’S RULE OF 9 (for Adults)
- Head and neck is 9% (NB. The head alone is 8% and the neck is 1%).
- Each arm is 9% (both arms carry 18%).
- Anterior trunk-18% (chest and abdomen).
- Posterior trunk-18% (from neck to symphysis, coccyx).
- Each lower limb-18% (both limbs 36%).
- Perineal/genital area-1%.
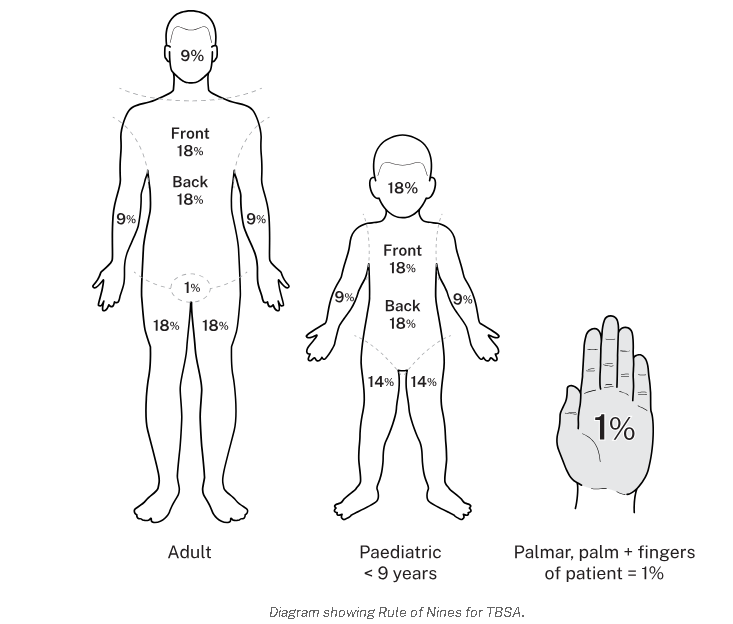
WALLACE’S RULE IN CHILDREN (slight difference)
- Head -18%
- Arms -9%
- Chest and trunk -18%
- Back of trunk -18%
- Legs -14%
- Perineal and genital area -1%
Use of Lund Browder’s chart
| Head | 7% |
| Neck | 2% |
| Anterior trunk | 13% |
| Posterior trunk | 13% |
| Rt buttock | 2.5% |
| Lt buttock | 2.5% |
| Genitalia | 1% |
| Rt upper arm | 4% |
| Lt upper arm | 4% |
| Rt lower arm | 3% |
| Lt lower arm | 3% |
| Rt hand | 2.5% |
| Lt hand | 2.5% |
| Rt thigh | 9.5% |
| Lt thigh | 9.5% |
| Rt leg | 7% |
| Lt leg | 7% |
| Rt foot | 3.5% |
| Lt foot | 3.5% |
| Total | 100% |
PREDISPOSING FACTORS & ASSESSMENT
PREDISPOSING FACTORS
- Age, children and old (weak)
- Disease-commonly epilepsy, leprosy
- alcoholism, and cigarette smoking
- Occupation-e.g. electricians, industrial workers, alcohol brewers
- Poverty e.g crowded kitchen.
- Fights (wrangles and conflicts)
- Race e.g. frost bite common in whites
- Skin bleaching.
SIGNS AND SYMPTOMS OF BURNS
- History of involvement with any of the cause of burns.
- Blistering due to vasodilation hence collection of serum between the dermis and epidermis.
- Necrosis due to coagulation of proteins.
- Functional impairment of the temperature regulation process of the burnt area.
- Shock due to fluid loss and blood loss (hypovoleamic shock).
- Shock can also occur due to severe pain (neurogenic shock).
- Toxaemia depending on the type and cause of burns. Histamines and adenocytes produced are released from the burnt surface and they find their way into the blood stream.
ASSESSMENT OF BURNS
- Circumstances and cause of burns i.e. where and when did it occur.
- Was the airway affected? Assess whether it was in closed spaces (inhaled hot gases).
- Assess the extent, location and depth. The bigger the burn, the higher the extent (%) the greater the surface area.
CRITERIA FOR ADMISSION OF BURNT PATIENT.
- Burns involving the airways
- Full thickness.
- Admit all children for observation
- The bigger the surface area above 5% superficial burns.
- Special areas involved e.g. face, hands, joints, neck, and genitalia.
- Circumferential burns give a tourniquet effect may cause gangrene.
- Electric burns because all electric burns are said to be deep until proved otherwise.
- Chemical burns, can continue burning for several days.
- If you are not sure; below 15% burns, GIT absorption is intact, oral route work in fluid replacement.
FIRST AID FOR BURNS.
AIMS
- Maintain an open airway.
- Minimize the risk of infection
- Treat any other associated injuries
- Make sure you watch for signs of shock.
- Make sure you check for signs of respiratory distress.
ACHIEVING THE FIRST AID MANAGEMENT
- Decrease temperature /stop fire if possible.
- Call for help.
- Evacuate the patient; pour water on the affected area.
- Undress the patient.
- Assume the airway has been affected until proved otherwise continue pouring water on the burnt area for minimally 20min to reduce injury i.e neutralized heat.
- Lie patient down but avoid the burnt area touching the ground.
- Pour water on burns for 20mins.
- Continue pouring water until pain stops.
- Put on gloves.
- Remove rings, shoes, watches, necklace, belts, stockings and clothes before tissue damage.
- Cover the injured area with sterile cloth or sterile dressing.
- Record details of injuries.
- Regularly monitor and record the vital signs and the level of consciousness, urine output.
- Treat shock if present.
- Re-assure and give words of hope.
- Avoid over cooling the patients especially children and elderly because they may get hypothermia.
- Do not remove anything stuck on the burnt wound to prevent spread of infections and more injuries.
- Do not touch the burnt area with your fingers.
- Do not apply lotions on the burn apart from anti-septic.
- Do not burst any blisters.
- If burns are on the face do not cover them for easy assessment of respiratory distress.
FOR AIRWAY BURNS
Burns of the face, mouth, throat, nose, airway passages, are serious because the airway passage rapidly becomes swollen because of inflammation.
How to assess for airway burns.
- History taking.
- Respiratory rate increased.
- Examine the nostrils i.e there is no soot.
- Examine the nasal hair i.e if they are burnt, short with a Taft.
- There would be damaged to the skin around the nose and mouth.
- Has difficulty in breathing.
- Has hoarse voice due to inflammation of vocal cords.
AIMS OF MANAGEMENT
- To recognize the airway burns.
- To maintain the airway and after take the patient to hospital management.
First Aid Management for Airway Burns
- Open the mouth (airway) and check whether he is breathing.
- Sweep the tongue.
- If not breathing, give rescue breaths, mouth to mouth. Put patient in a recovery position and call for help.
- Take the steps to improve the airway e.g remove clothes or unbutton, clear the place.
- Re assure the patient.
- Monitor and record vital observations until help arrives.
Interventions in the hospital
Put patient on oxygen therapy. Intubate the patient with endotracheal tube, connected to oxygen cylinder.
FOR CHEMICAL BURNS
The commonest cause of chemical burns in Uganda are domestic fights and it’s commonly women to women.
FIRST AID
- Ensure your safety.
- Disperse the powerful chemical by wiping away the chemical, pouring water (plenty) for about 30min. This dilutes the chemical.
- Arrange to transfer patient to hospital but label the chemical if you have identified it.
- Do not attempt to neutralize the chemical with another chemical.
- Ensure that you remove contaminated clothing.
- If the face has been burnt, expect the burns of the airway. Make sure that the airway is open and functioning.
How do you recognize chemical burns
- There may be chemicals in the vicinity.
- The pain is intense and stinging (itching).
- Later discoloration, blistering and peeling of the skin forming wound.
- Supportive treatment with anti-inflammatory drugs, anxiolytics, painkillers.
- Re-assure the patient.
FOR ELECTRIC BURNS
These occur when electricity passes through the body, person a conductor through which electricity passes. Most of the visible damage occurs at points of entry and exit of the current. You may have an internal tract where wounds are mainly concentrated. The current follows mainly muscle, nerves and blood vessels. If it follows the nerves, it can cause cardiac arrest which is the commonest cause of death in electric burns.
NOTE:
The current will cause muscle spasms which may prevent patient from breaking contact with electric source hence continues electric shock. Switch off the main switch. Do not touch a patient with live hands or metallic materials to break the contact. Assess the ABC immediately. Shout for help. Be safe, do something and waste no time.
FIRST AID {AIMS}
- Ensure your safety first.
- Ensure that electric source is disconnected or blocked i.e you may use your shoes or clothes to disconnect the source from patient.
- Flood the exit and entry points with water to cool the burn and prevent further burning process.
- Protect the burn from infection.
- Re-assure
- Give treatment for shock.
ASSESSMENT FOR BURNS TO THE EYE.
Patient is usually unconscious or semi-conscious. If eyes are burnt with chemicals, it will cause scarring and blindness so gets water and wash the eyes to dilute and disperse the acid. Let them not rub the eyes (don’t touch the eyes), continue pouring water in the eyes.
SIGNS AND SYMPTOMS OF EYE BURNS.
- Continue watering the eyes
- Swollen
- redness
Treatment
- Have gloves on.
- Lie the patient with the affected eye low and most so that water does not affect the rest of the face.
- Open that eye and run cold water for more than 30 minutes.
- Make sure that the water is penetrating into all parts of the eye. Open eye with your hands if they cannot open.
- Get a clean bandage and close the eye until the opthalmist comes.
- Try to identify the chemical and record or label.
GENERAL MANAGEMENT OF BURNS
Aims of management
- To arrest bleeding.
- To prevent the condition from worsening.
- To preserve life.
- To correct electrolyte imbalances. Etc
N.B Burns with a TBSA greater than 15% the following is done. It is a surgical emergency so quit assessment and immediate care is needed plus quick admission. (Immediate nursing care).
Airway maintenance
Through opening and clearing the airway, In case of a suspected cervical spine, keep movements of the neck to a minimum and never hyperflexion or hyperextend to head or neck. If smoke inhalation is suspected intubate before oedema makes it difficult. The head of the bed is elevated and nasal pharynx suction is done incase of excessive secretions.
Breathing and ventilation.
Expose the chest and make sure that chest expansion is adequate. Always provide oxygen in severe burns or when inhalation injury is suspected give 4-8 hr/min. Assess breathing sounds and respiratory rate. Monitor for hypoxia. Encourage aggressive pulmonary care e.g. turning, coughing and deep breathing.
Circulation and hemorrhage control
Stop bleeding with direct pressure. Check capillary if greater than 2secs it means hypovolaemia. Monitor pulse and check pallor which occurs with 30%. Insert 2 large bore peripheral IV lines in superficial burns.
Assessment of the neurological status.
This is done through using a glasgowcoma scale. This helps to check the levels of consciousness that is checking;
- Alertness (A)
- Response to vocal stimuli (V)
- Response to painful stimuli (U)
- Unresponsive.
Examine the pupils for light reaction. Hypoxia can cause reduced levels of response. Keep the patient flat and covered with a sterile sheet to relieve the pain induced by circulatory air currents. Keep the patient warm and check for any adherent clothing, cut around it, when removing the cloth i.e cut around the edges of the clothes disturbing the wound as little as possible.
GENERAL NURSING CARE OF A BURN PATIENT
Maintenance of an aseptic environment.
All attendants must wear capes, gowns, masks and cover shoes. Hands should be washed thoroughly. Cleaning should consist of sloughing skin and use of aseptic solution like hibitane or savlon, the surface is then dried with warm air or sterile dressing (gauze). Afterwards the burnt area is treated by either the exposure method or closed of dressing.
Management of wounds.
- Nurse the patient in a special room to prevent infections (burns are normally sterile). Make sure that you maintain asepsis as much as possible.
- Avoid touching the wound with bear hands i.e. use sterile gloves and use a disinfectant after attending to the patient.
- You must have a mask while examining the patient.
- Use the mosquito net to protect the patient from flies.
- Limit visitors as these increase the risk of infection we give definitive treatment (dress) after resuscitation for burns involving the eyes attend to airway then the burnt eyes and resuscitation later.
FLUID REPLACEMENT
Always replace the lost fluids, can be IV or orally since fluid absorption in the GIT is now very poor. IV fluids are recommended. If an adult loses 15% of the body fluid or as little as 10% in a small child, this will lead to shock. Replacement needs to be continued for at least 48hours.
In deep burns, plasma is given as this is what the patient is losing in 48hours. Towards the end of 48hours, whole blood is given to replace RBCs destroyed, later N/S to replace electrolytes. Glucose to replace energy loss.
Fluid Replacement Calculation (Parkland Formula basis)
The volume of fluid replacement (Y) = (weight in kg X surface area of burns) mls / 2. This volume is given over 8 hours.
Example: Y = (70kg X 20%) / 2 = 700mls. Y=700mls in 4 hours so multiply it by 2 = 1400mls in first 8hours.
- Y=1400mls in the next 16hours
- Y=1400mls in the next 24hours
But adults require 3 liters in 24hours with or without burns (normal physiological fluid requirement). How much is needed Z = (3000x1)/24 = 125mls per hour.
The rate of fluid loss in children below 6yrs is twice that of adults hence double the fluids to be replaced.
Management of Wounds
- Nurse the patient in a special room to prevent infections (burns are normally sterile).
- Avoid touching the wound with bear hands i.e. use sterile gloves and use a disinfectant after attending to the patient.
- You must have a mask while examining the patient.
- Use the mosquito net to protect the patient from flies.
- Limit visitors as these increase the risk of infection.
EXPOSED METHOD
Nothing touches the burn except air and anti-bacterial agent e.g. hibitane, ghee and honey. This indicates for burns of the face especially scalds. It is good for areas that are difficult to dress e.g. perineum, buttocks, face, Axilla.
OCCLUSIVE / CLOSED METHOD.
This method keeps the wound sterile, also aims at applying anti-bacterial agents. E.g. ghee, honey, neomycin cream, tetracycline, hibitane etc.
PROCEDURE FOR BURN DRESSING APPLICATION
This procedure emphasizes a "no-touch" sterile technique to prevent infection.
- Ensure Sterility: Utilize a number touch technique, meaning no human hand shall directly touch the burn or the dressing materials, except when sterile. All instruments used must be sterile.
- Consider Sedation: Administer appropriate sedation if required, to ensure patient comfort and cooperation during the procedure.
- Clean the Area: Gently clean the burn wound and the surrounding healthy skin with Chlorhexidine solution.
- Manage Blisters: Leave any blisters intact; do not puncture them, as they provide a natural protective barrier against infection.
- Apply Impregnated Gauze: Using a sterile spatula, carefully apply the impregnated gauze directly onto the burn wound.
- Apply Dry Gauze: Cover the impregnated gauze with at least 2cm of dry gauze.
- Add Cotton Wool: Place approximately 3cm of cotton wool over the dry gauze layer.
- Secure with Crepe Bandage: Apply a crepe bandage to secure all layers of the dressing.
- Extend Dressing Margins: Ensure the entire dressing extends beyond the wound margin by about 10cm to provide adequate coverage and protection.
Prevention of Burns
- Treat the epileptics, teach them, and mobilize the community about epileptics with burns.
- Raised fire places.
- Keep flues out of the houses e.g. petrol.
- Keep chemical in raised places and out of reach of children.
- Avoid bleaching.
- Keep children out of hot or fire places.
COMPLICATIONS OF BURNS
- Shock.
- Excessive oedema, quite dangerous if burns are of the face, neck as it causes obstruction of the airway and oesophagus.
- Renal failure; due to failure to give adequately fluids.
- Toxaemia and infections; infection of the burnt area causing sepsis resulting in septicaemia, gas gangrene and tetanus.
- Depression of the bone marrow.
- Contractures.
- Keloid formation
- Electrolyte imbalance
- Anaemia due to haemolysis.
- Thrombosis due to plasma loss.
- GIT bleeding, ulcers develop due to increased production of gastric acid.
- Paralytic ileus.
- Sepsis.
- Neuromas
- Cosmetic disfigurement
- Mal-function of the body part
BURNS LECTURE NOTES Read More »
Surgical Shock
COMMON SURGICAL CONDITIONS
SHOCK
Definition
- Shock is a state of poor perfusion with impaired cellular metabolism manifesting with severe pathophysiological abnormalities. It is due to circulatory collapse and tissue hypoxia. Shock is meant by ‘inadequate perfusion` to maintain normal organ function.
- The condition associated with circulatory collapse when the arterial blood pressure is too low to maintain an adequate supply of blood to the tissues.
- The failure of the circulatory system to adequately supply oxygen to the tissues.
Shock is a life-threatening medical condition characterized by inadequate tissue perfusion and oxygenation, leading to cellular dysfunction, widespread organ damage, and if uncorrected, irreversible organ failure and death. It's not simply low blood pressure, but rather a critical imbalance between the demand for oxygen and nutrients by the cells and the body's ability to deliver them.
ETIOLOGY AND PATHOPHYSIOLOGY
Shock has a multitude of causes. The most common cause of shock is severe blood loss i.e. if it exceeds 1.2 liters.
The circulation may fail because of the following:
Sudden malfunction of the heart. This may occur as a result of:- Coronary arterial occlusion with acute myocardial ischaemia.
- Trauma with structure damage to the heart
- Toxaemia – bacterial or viral
- Effects of drugs
- Postoperative atelectasis and pneumonia
- Thoracic injuries, particularly tension pneumothorax, bruising and laceration of the lungs
- Obstruction of the pulmonary artery by an embolus.
- Disturbances of lung function following surgery and anesthesia.
- Whole blood – haemorrhage
- Plasma – significant in burns
- Water and electrolyte which occurs in: Peritonitis, Intestinal obstruction and paralytic ileus, Severe diarrhoea and vomiting.
- Adrenal deficiency
- The common faint. The arterioles in the muscle relax
- Over dosage of drugs eg analgesic like pethedine
- Following therapy with beta blocking agents for angina, hypertension etc
- Noxious stimuli, such as pain, if severe with cause vasodilation
- Systolic dysfunction: it is the inability of the heart to pump forward like in myocardial infarction and cardial myopathy
- Diastolic dysfunction: it is the inability of the heart to fill e.g. cardiac tamponade, ventricular hypertrophy and cardial myopathy
- Dysrhythmias eg in bradyrhythmias and tarchyrhythmias
- Structural factors like valvular stenosis or regurgitation, ventricular septal rapture
- Internal bleeding like fracture of long bones, ruptured spleen heamopneumothorax and severe pancreatitis
- Fluid shift like in burns and cysts
- Spinal anesthesia
- Vasomotor center depression
Types, and Clinical Manifestations
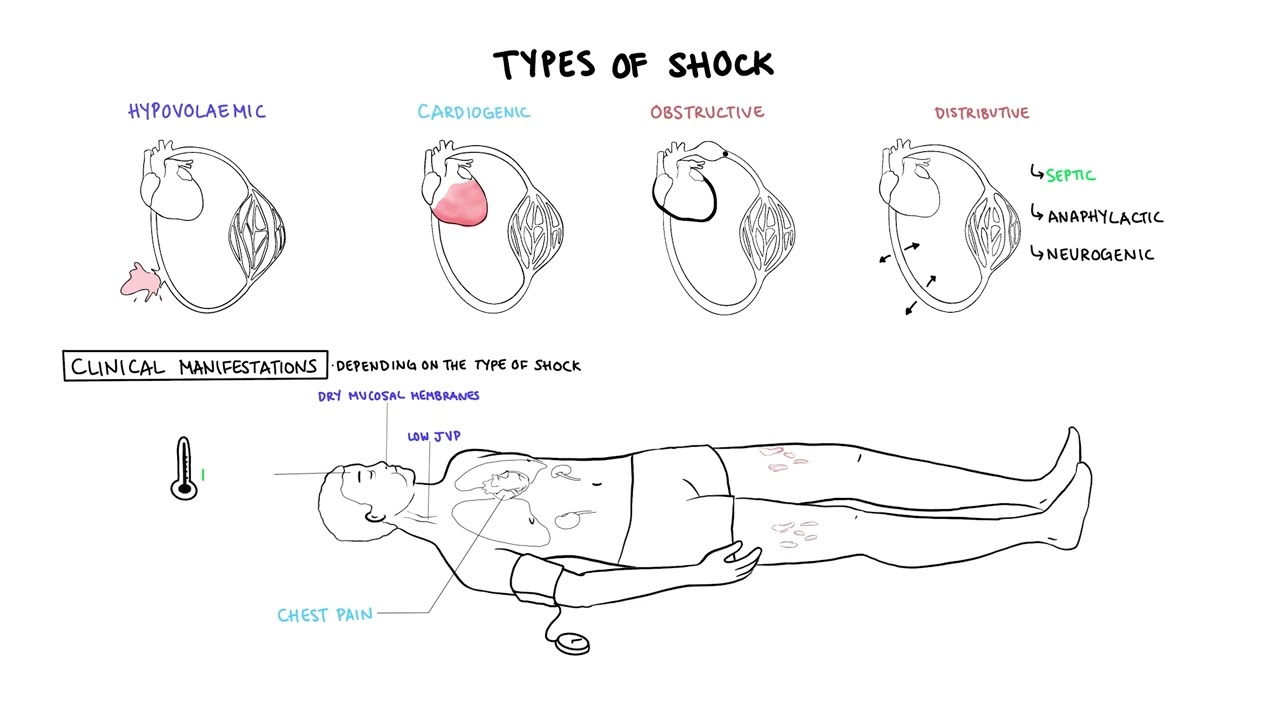
Types of Shock: Categorization by Underlying Pathophysiology
Shock is broadly classified into several types based on the primary physiological mechanism causing the inadequate tissue perfusion. While these types have distinct primary causes, they often share common clinical features and can coexist or lead to one another.
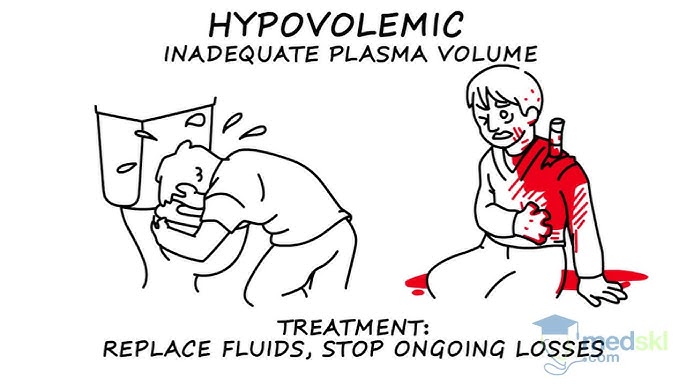
1. Hypovolemic Shock (Inadequate Circulating Volume)
- Trauma (external or internal bleeding)
- Gastrointestinal bleeding (e.g., peptic ulcer, variceal bleeding)
- Post-surgical bleeding
- Obstetric hemorrhage (e.g., postpartum hemorrhage)
- Aortic rupture
- Severe Dehydration: Vomiting, diarrhea, inadequate fluid intake.
- Severe Burns: Massive fluid shifts from intravascular space into interstitial space.
- Peritonitis/Bowel Obstruction: Fluid sequestration within the abdominal cavity or bowel lumen.
- Diabetic Ketoacidosis (DKA) / Hyperosmolar Hyperglycemic State (HHS): Profound osmotic diuresis.
- Excessive Diuretic Use.
2. Cardiogenic Shock (Pump Failure)
- Myocardial Infarction (MI): Especially extensive anterior or left ventricular MI, which damages a significant portion of the heart muscle.
- Severe Arrhythmias: Tachyarrhythmias (e.g., ventricular tachycardia, atrial fibrillation with rapid ventricular response) or bradyarrhythmias that significantly reduce ventricular filling time or heart rate.
- Valvular Heart Disease: Acute severe mitral regurgitation, aortic stenosis.
- Cardiomyopathies: Acute exacerbation of chronic heart failure.
- Myocarditis: Inflammation of the heart muscle.
- Acute Papillary Muscle Rupture.
3. Distributive Shock (Vasogenic Shock / Abnormal Vasodilation)
a. Septic Shock:
- Definition: A life-threatening organ dysfunction caused by a dysregulated host response to infection, leading to persistent hypotension requiring vasopressors to maintain mean arterial pressure (MAP) ≥ 65 mmHg and having a serum lactate level > 2 mmol/L despite adequate fluid resuscitation.
- Pathophysiology: Triggered by severe infection (bacterial, viral, fungal). Pathogen-associated molecular patterns (PAMPs) and danger-associated molecular patterns (DAMPs) released from pathogens and damaged host cells activate a complex inflammatory cascade. This leads to widespread endothelial dysfunction, microcirculatory alterations, profound vasodilation, increased capillary permeability (fluid leakage into interstitial spaces leading to relative hypovolemia and edema), and myocardial depression.
- Causes: Severe infections, particularly with Gram-negative bacteria (e.g., *E. coli, Klebsiella, Pseudomonas*) or Gram-positive bacteria (e.g., *Staphylococcus aureus, Streptococcus pneumoniae*). Common sources include pneumonia, urinary tract infections, abdominal infections (e.g., appendicitis, diverticulitis), and skin/soft tissue infections.
- Clinical Features: Often presents as "warm shock" in early stages (warm, flushed skin, bounding pulses) due to vasodilation, progressing to "cold shock" as compensatory mechanisms fail and cardiac output falls.
- Definition: A severe, life-threatening systemic allergic reaction characterized by rapid onset of profound vasodilation, increased vascular permeability, and bronchoconstriction.
- Pathophysiology: Exposure to an allergen triggers a massive release of inflammatory mediators (e.g., histamine, leukotrienes, prostaglandins) from mast cells and basophils. These mediators cause widespread vasodilation and leakage of fluid from capillaries into the interstitial space, leading to circulatory collapse and airway obstruction.
- Causes: Exposure to allergens such as insect stings, certain foods (e.g., peanuts, shellfish), medications (e.g., antibiotics, NSAIDs), or latex.
- Definition: Occurs due to loss of sympathetic nervous system tone, leading to widespread vasodilation and pooling of blood in the periphery. Unlike other forms of shock, the heart rate may be paradoxically normal or even bradycardic.
- Pathophysiology: Damage to the sympathetic nervous system (typically above T6) interrupts the normal vasoconstrictive impulses to peripheral blood vessels. This results in unopposed parasympathetic activity, leading to profound vasodilation and often bradycardia.
- Causes:
- Spinal cord injury (most common cause).
- Spinal anesthesia.
- Guillain-Barré Syndrome.
- Severe head trauma (less common as a primary cause).
- Certain drugs (e.g., ganglionic blockers, adrenergic antagonists).
- Definition: Shock resulting from acute hormonal deficiencies that disrupt normal cardiovascular function and metabolic processes.
- Causes: Adrenal crisis (acute adrenal insufficiency leading to severe hypotension refractory to fluids and vasopressors due to lack of cortisol) or myxedema coma (severe hypothyroidism leading to decreased cardiac output, bradycardia, and hypothermia).
4. Obstructive Shock (Extracardiac Obstruction to Blood Flow)
- Pulmonary Embolism (PE): Massive PE obstructs blood flow from the right ventricle into the pulmonary circulation.
- Cardiac Tamponade: Accumulation of fluid or blood in the pericardial sac, compressing the heart and preventing adequate ventricular filling.
- Tension Pneumothorax: Air accumulation in the pleural space collapses the lung and shifts the mediastinum, compressing the great vessels and heart.
- Constrictive Pericarditis (severe acute exacerbation).
- Critical Valvular Stenosis (less common as primary obstructive shock).
5. Vasovagal Shock (Neurocardiogenic Syncope)
- Definition: While often presenting as syncope (fainting), severe forms can lead to a transient state of shock. It's characterized by a sudden, exaggerated reflex response that results in both widespread peripheral vasodilation and bradycardia.
- Pathophysiology: Triggered by certain stimuli (e.g., pain, fear, emotional stress, prolonged standing, specific odors). The vagus nerve is overstimulated, leading to parasympathetic activation (bradycardia) and sympathetic inhibition (vasodilation), causing a temporary drop in blood pressure and cerebral perfusion.
- Clinical Significance: Usually self-limiting and resolves upon lying down. Rarely life-threatening unless associated with significant trauma from a fall. Not considered a true "shock state" in the critical care sense as it's typically transient and reversible with simple measures.
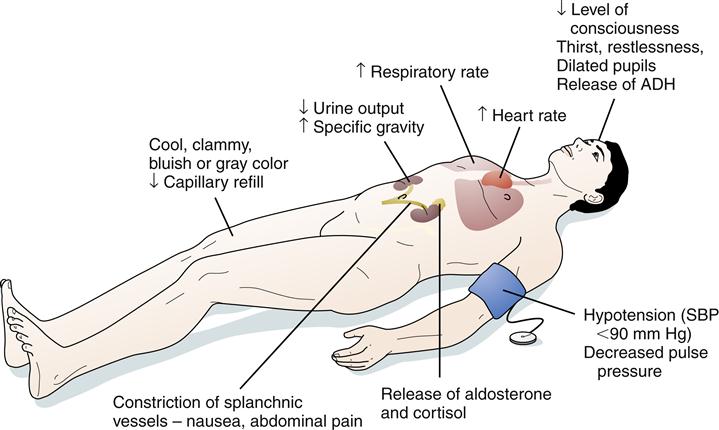
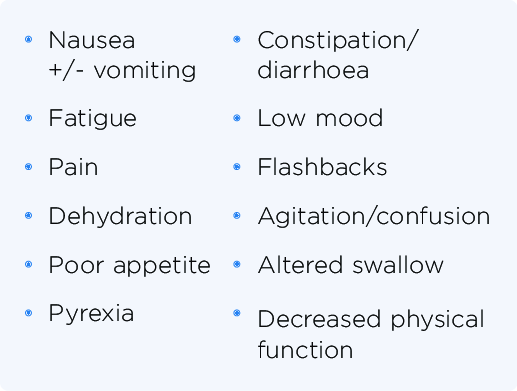
Recognition Features of Shock / Signs and Symptoms of Shock
The signs and symptoms of shock are a reflection of the body's compensatory mechanisms attempting to maintain vital organ perfusion, followed by the failure of these mechanisms as shock progresses. The specific presentation can vary slightly depending on the type and stage of shock.
I. Early / Compensatory Stage (Body's attempt to maintain vital organ perfusion)
In this initial stage, the body activates its sympathetic nervous system and hormonal responses to maintain blood pressure and vital organ blood flow. This often leads to increased heart rate and vasoconstriction.
Cardiovascular:- Rapid Pulse (Tachycardia): The earliest and most consistent sign. The heart beats faster to compensate for reduced cardiac output.
- Normal to Slightly Decreased Blood Pressure: The body is still able to maintain BP through vasoconstriction.
- Pale, Cool, Clammy Skin: Due to peripheral vasoconstriction shunting blood away from the skin to vital organs. The clamminess is due to diaphoresis (sweating) caused by sympathetic stimulation.
- Delayed Capillary Refill: >2 seconds (indicates poor peripheral perfusion).
- Restlessness, Anxiety, Agitation: Early signs of cerebral hypoperfusion and catecholamine release.
- Increased Thirst: Due to fluid shifts and activation of the renin-angiotensin-aldosterone system.
- Oliguria: Decreased urine output (< 0.5 mL/kg/hr) as kidneys conserve fluid and blood flow is shunted away.
- Slightly Increased Respiratory Rate: Due to metabolic acidosis (from anaerobic metabolism) and increased oxygen demand.
II. Progressive / Decompensatory Stage (Compensatory mechanisms begin to fail)
As shock progresses, the compensatory mechanisms become overwhelmed, leading to widespread cellular hypoxia, anaerobic metabolism, and accumulation of lactic acid. Organ function begins to deteriorate.
Cardiovascular:- Hypotension: Significant drop in systolic blood pressure (<90 mmHg or MAP <65 mmHg) or a drop of >40 mmHg from baseline. This is a critical sign that compensation has failed.
- Weak, Thready Pulse: Rapid but difficult to palpate, indicating profound vasoconstriction and low stroke volume.
- Progressively Colder, Mottled Skin: Especially in extremities (e.g., "grey-blue skin," cyanosis of lips and nail beds) due to severe peripheral vasoconstriction and pooling of deoxygenated blood.
- Lethargy, Drowsiness, Confusion: Worsening cerebral hypoperfusion.
- Decreased Responsiveness to Stimuli.
- Nausea, Vomiting: Due to reduced blood flow to the GI tract.
- Abdominal Pain.
- Rapid, Shallow Breathing (Tachypnea): The body's attempt to compensate for metabolic acidosis.
- Increasing Lactic Acidosis: Due to anaerobic metabolism.
III. Irreversible / Refractory Stage (Widespread cellular and organ damage)
In this final stage, cellular and organ damage becomes so severe that it is irreversible, even with aggressive interventions. Multi-organ dysfunction syndrome (MODS) develops, leading inevitably to death.
Cardiovascular:- Profound Hypotension: Unresponsive to fluids and vasopressors.
- Severe Tachycardia or Bradycardia: With eventual cardiac arrest.
- Absent Peripheral Pulses.
- Unconsciousness, Coma.
- Fixed, Dilated Pupils.
- Loss of Reflexes.
- Gasping for Air (Agonal Respirations): Severe respiratory distress.
- Respiratory Failure.
- Anuria: Complete cessation of urine production.
- Acute Kidney Injury.
- Severe Lactic Acidosis: Uncorrectable.
- Electrolyte Imbalances.
- Disseminated Intravascular Coagulation (DIC): Widespread clotting and bleeding.
- Multi-Organ System Failure (MOSF).
Special Considerations: Warm Shock (Septic Shock in Early Stages)
While most forms of shock present with cool, clammy skin due to vasoconstriction, early septic shock (hyperdynamic or "warm shock" phase) can present differently due to the profound systemic vasodilation:
- Warm, Dry, Flushed Skin: Due to peripheral vasodilation.
- Rapid, Strong (Bounding) Pulse: Indicating a hyperdynamic state and decreased systemic vascular resistance.
- Fever: Evidence of underlying infection.
- Hyperventilation: To compensate for metabolic acidosis.
- Despite these initial "warm" signs, tissue perfusion is still inadequate at the microcirculatory level, and this phase rapidly progresses to decompensated ("cold") shock if not aggressively treated.
MANAGEMENT OF SHOCK
AIMS
- To treat the cause
- To improve cardiac function
- To improve tissue perfusion
Emergency treatment for shock
- Help patient to lie down and place patient in supine position
- Cover patient and keep him or her warm
- Raise and support her legs as high as possible
- Administer oxygen if possible
- Determine underlying cause and treat if possible e.g. applying pressure for bleeding.
- Lessen any tight clothing, undo anything that constrict the neck, chest and wrist
- Monitor breathing, pulse and response
- Monitor and record vital observation like pulse breathing, monitor level of response, if the casualty become unconscious, open the airway and check breathing.
General management
- Treat the cause e.g. arrest haemorrhage, drain pus etc.
- Fluid replacement e.g. plasma normal saline dextrose ringers lactate, plasma expanders maximum 1 liter can be given in 24hours.
- Blood transfusion is done whenever necessary, hypotonic solutions like dextrose are poor volume expanders and so should not be used in shock.
- Inotropic agents e.g. dopamine, dobutamine, adrenaline infusions.
- Correction of acid base balance. Acidosis is corrected by using 8.4 sodium bicarbonate intravenously.
- Steroid is often life saving. 500- 1000mg of hydrocortisone can be given. It improves perfusion, reduces the capillary leakage and systemic inflammatory effects.
- Antibiotics in patients with patients with sepsis; proper control of blood sugar and ketosis in diabetic patients.
- Catheterization to measure urine output (30 – 50mls/hour or > 0.5 ml/kg/ hour should be maintained).
- Nasal oxygen to improve oxygenation or ventilator support with intensive care unit monitoring has to be done.
- Haemodialysis (a process of removing a waste part e.g. kidney) may be necessary if kidneys are not functioning.
- Control pain using morphine (4mg iv).
- Injection ranitidine iv or omeprazole iv or pantoprazole iv.
- Activated c protein, it is beneficial as it prevents the release of inflammatory response.
- Diuretics, mannitol is an osmotic that neither absorbed in the renal tubules nor metabolized. It may be given when acidosis and Oliguria have been corrected but if oliguria persist frusemide may also be given.
- Anticoagulants may occasionally be indicated if micro- circulatory thrombosis is suspected.
Prevention of shock
Pre operative measures
- Take thorough history which include biographic data, medical history, obstetric history, gynaecological.
- Assess the level of consciousness.
- Take the baseline vital observation which include temperature, pulse, respiration and blood.
- General body assessment from head to toe to rule out abnormalities like oedema, hemorrhage, cyanosis and pallor.
- If there is external heamorrhage arrest the bleeding by positioning the patient.
- Empty the bladder by passing a catheter.
- Antibiotic prophylaxis is given to prevent sepsis.
- Take investigation such as hemoglobin estimation, cross matching, blood grouping and cross matching, clotting factor, malaria slide etc.
- Give anxiolytics to allay anxiety and give pain killer to reduce pain.
- Resuscitate patient with iv fluids.
- Reassure the patient.
- The patient should be educated about physical exercises which are done post operatively.
- Circulatory collapse should be avoided by strenuous measures if all possible.
- Preoperatively patient should be fit as possible from the point of view of the circulatory system: His blood should be a adequate in quality and volume, His tissues should be hydrated adequately, He should be mobile so that there is no stagnation in the circulatory system.
Intra operatively
- Patient is kept warm on his journey from the ward to the theater and back.
- Fear is allied and tranquiller are commonly used pre- operatively.
- The blood pressure is monitored continuously and recorded more so for the serious cases.
- Blood and fluid replacement is commenced in good time and the patient is monitored using fluid balance chart.
- Major operations are commenced only after satisfactory infusions have been established.
- The head of the bed is lowered if the blood pressure falls (Trendelenburg position).
- The anesthetist induces and maintains an adequate level of anesthesia ensuring good oxygenation and tissue perfusion.
Post operatively measures
- Fluid and electrolyte replacement (saline, 5% dextrose, Hartman solution, plasma and blood as indicated).
- Position the patient in a recovery position.
- Maintain air way patent.
- Give antibiotics to prevent infections.
- Give inflammatory drugs.
- Check the conscious level of the patient.
- Initiate exercise like coughing, deep breathing and ambulation to aid normal circulation.
- Rest and relieve of pain are continued to prevent shock.
General Nursing Considerations and Principles for Patients in Shock
Nursing care for a patient in shock is complex, dynamic, and requires rapid assessment, intervention, and continuous monitoring. The primary goals are to optimize tissue perfusion, restore hemodynamic stability, identify and treat the underlying cause, and prevent complications. Nurses work collaboratively with the medical team to implement a comprehensive plan of care.
Nursing Diagnoses)
Nursing diagnoses guide the individualized care plan for patients. Examples for a patient in shock might include:
- Decreased Cardiac Output related to altered preload, afterload, contractility, or heart rate, as evidenced by hypotension, tachycardia, altered mental status, decreased urine output, and cool, clammy skin.
- Ineffective Tissue Perfusion (Cardiac, Cerebral, Renal, Gastrointestinal, Peripheral) related to hypovolemia, impaired cardiac pump function, maldistribution of blood flow, or obstruction, as evidenced by pallor, cyanosis, delayed capillary refill, weak peripheral pulses, altered mental status, oliguria, and increased serum lactate.
- Impaired Gas Exchange related to ventilation/perfusion mismatch, increased metabolic demand, or pulmonary edema, as evidenced by tachypnea, dyspnea, abnormal blood gas values, and cyanosis.
- Deficient Fluid Volume related to active fluid loss, failure of regulatory mechanisms, or third-space fluid shift, as evidenced by hypotension, tachycardia, decreased urine output, and dry mucous membranes.
- Risk for Infection related to invasive procedures, compromised immune status, or presence of underlying infection.
- Acute Confusion related to decreased cerebral perfusion, metabolic imbalances, or hypoxia, as evidenced by disorientation, agitation, or altered level of consciousness.
- Risk for Imbalanced Body Temperature related to altered metabolic rate, infection, or environmental factors.
- Anxiety/Fear related to critical illness, threat of death, or unpredictable prognosis.
Nursing Interventions (General Principles - specific actions depend on the type of shock)
Interventions are aimed at supporting vital organ function, addressing the underlying cause, and minimizing further deterioration. These often fall into categories of hemodynamic support, respiratory support, infection control, and monitoring.
1. Optimize Hemodynamic Status and Perfusion:
- Fluid Resuscitation: Administer intravenous fluids (crystalloids or colloids) as prescribed and monitor response (e.g., blood pressure, heart rate, urine output, central venous pressure).
- Vasopressors/Inotropes: Administer vasoactive medications (e.g., norepinephrine, dopamine, dobutamine) as prescribed to improve blood pressure and cardiac output, titrating carefully to desired effect and continuously monitoring for adverse effects (e.g., arrhythmias, tissue ischemia).
- Blood Product Administration: Administer blood transfusions (e.g., packed red blood cells, plasma, platelets) for hemorrhagic shock as indicated.
- Positioning: Position the patient to optimize cardiac output and venous return (e.g., modified Trendelenburg for hypovolemic shock if tolerated and not contraindicated).
- Maintain Body Temperature: Prevent hypothermia, which can worsen acidosis and coagulopathy. Use warming blankets if necessary.
2. Support Respiratory Function and Oxygenation:
- Oxygen Therapy: Administer high-flow oxygen via appropriate device (e.g., non-rebreather mask).
- Airway Management: Assess and maintain a patent airway. Prepare for and assist with intubation and mechanical ventilation if respiratory failure is imminent or present.
- Ventilator Management: Monitor ventilator settings, ensure proper oxygenation and ventilation, and prevent ventilator-associated complications.
- Arterial Blood Gas (ABG) Monitoring: Frequently assess ABG results to monitor oxygenation, ventilation, and acid-base balance.
3. Monitor and Assess Continuously:
- Vital Signs: Monitor heart rate, blood pressure (preferably arterial line), respiratory rate, and oxygen saturation continuously and frequently.
- Cardiac Monitoring: Continuous ECG monitoring for arrhythmias and signs of ischemia.
- Neurological Status: Assess level of consciousness, pupillary response, and motor function frequently to detect changes in cerebral perfusion.
- Urine Output: Insert an indwelling urinary catheter and monitor hourly urine output as a sensitive indicator of renal perfusion and overall hemodynamic status.
- Skin Assessment: Monitor skin color, temperature, turgor, and capillary refill for changes in perfusion.
- Laboratory Values: Monitor serial laboratory tests (e.g., CBC, electrolytes, lactate, renal and liver function tests, coagulation studies) to track response to treatment and detect complications.
- Fluid Balance: Accurately track all intake and output.
- Pain Assessment: Administer analgesia as needed, considering its effects on hemodynamics.
4. Identify and Treat the Underlying Cause:
- Administer broad-spectrum antibiotics promptly after obtaining cultures.
- Identify and control the source of infection (e.g., drainage of abscess, removal of infected line).
- Administer medications to improve cardiac contractility or reduce afterload as prescribed.
- Prepare for and assist with interventions like angioplasty, thrombolysis, or intra-aortic balloon pump (IABP) insertion.
- Identify and stop the source of bleeding or fluid loss.
- Administer fluids/blood products.
- Prepare for and assist with interventions to relieve obstruction (e.g., pericardiocentesis for tamponade, needle decompression/chest tube for tension pneumothorax).
5. Prevent Complications:
- Infection Control: Maintain strict aseptic technique for all invasive procedures (e.g., IV line insertion, Foley catheter care, wound care).
- Skin Integrity: Implement pressure injury prevention strategies (e.g., frequent repositioning, pressure-relieving devices) due to poor perfusion and immobility.
- Nutrition: Initiate enteral or parenteral nutrition as soon as feasible to support metabolic needs and gut integrity.
- Psychological Support: Provide emotional support to the patient and family, explain procedures, and answer questions honestly.
- Deep Vein Thrombosis (DVT) Prophylaxis: Administer prophylactic anticoagulants or use pneumatic compression devices as ordered.
6. Documentation and Communication:
- Document all assessments, interventions, and patient responses accurately and in a timely manner.
- Communicate effectively with the interdisciplinary team (physicians, respiratory therapists, pharmacists, etc.) regarding patient status, changes, and concerns.
GANGRENE
GANGRENE
Definition
Causes: Ischemia and Infection as Primary Drivers
- Thrombosis: Formation of a blood clot within a blood vessel, obstructing flow.
- Embolism: A piece of clot, fat, or other material travels and lodges in a blood vessel, blocking it.
- Atherosclerosis: Hardening and narrowing of arteries, leading to chronic reduction in blood flow, especially to the extremities.
- Vasoconstriction/Vasospasm: Severe narrowing of blood vessels (e.g., in Raynaud's phenomenon).
- External Compression: Pressure on blood vessels (e.g., from tight casts, prolonged immobility leading to pressure ulcers).
- Gas Gangrene: Caused predominantly by *Clostridium perfringens* and other anaerobic bacteria, which produce potent toxins and gas within tissues.
- Streptococcal and Staphylococcal Infections: While less common as a primary cause of widespread gangrene compared to clostridial species, severe invasive infections (e.g., necrotizing fasciitis) can rapidly lead to tissue death.
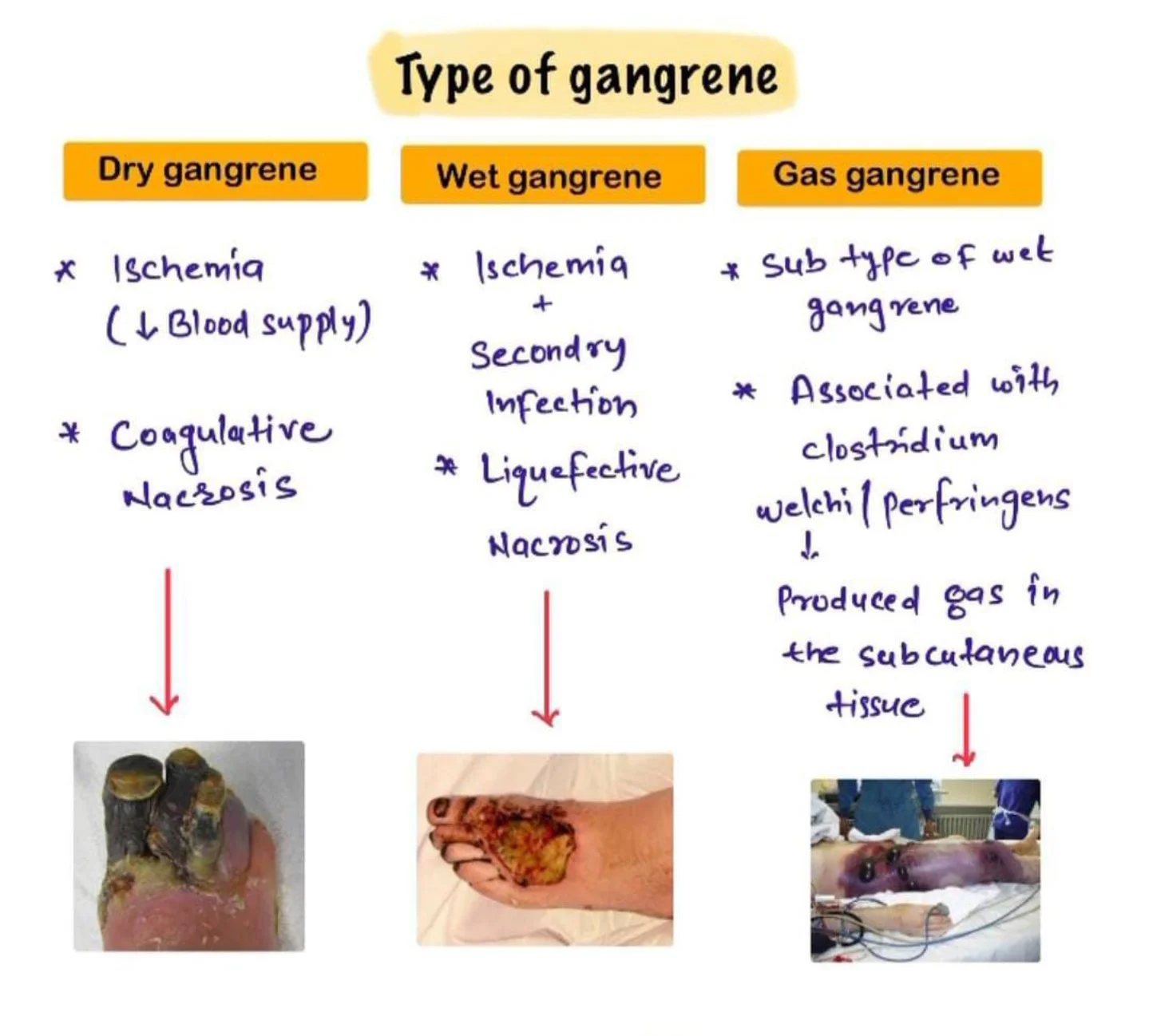
Types of Gangrene
Dry Gangrene
- Dry gangrene begins at the distal part of the limb due to ischemia and often occurs in the toes and feet of elderly patients due to arteriosclerosis (abnormal thickening and hardening of the arterial walls).
- Dry gangrene spreads slowly until it reaches the point where the blood supply is inadequate to keep tissue viable.
- The affected part is dry, shrunken and dark black, resembling mummified flesh.
- If the blood flow is interrupted for a reason other than severe bacterial infection, the result is a case of dry gangrene.
- People with impaired peripheral blood flow, such as diabetics, are at greater risk of contracting dry gangrene.
- The early signs are a dull ache and sensation of coldness in the affected area.
- If caught early, the process can sometimes be reversed by vascular surgery.
- If necrosis sets in, the affected tissue must be removed and treated like a case of wet gangrene.
Wet Gangrene
- Wet gangrene occurs in naturally moist tissue and organs such as the mouth, bowel, lungs, cervix, and vulva.
- Bedsores occurring on body parts such as the sacrum, buttocks and heels (not in “moist” areas) are also categorized as wet gangrene infections.
- In wet gangrene, the tissue is infected by microorganisms, which cause tissue to swell and emit a foul odour.
- Wet gangrene usually develops rapidly due to blockage of venous and/or arterial blood flow.
- The affected part is saturated with stagnant blood which promotes the rapid growth of bacteria.
- The toxic products formed by bacteria are absorbed causing systemic manifestation of bacteria and finally death.
- The affected part is soft, putrid, rotten and dark.
- The darkness in wet gangrene occurs due to the same mechanism as in dry gangrene.
Gas Gangrene
- Gas gangrene is a bacterial infection that produces gas within tissues.
- It is a deadly form of gangrene usually caused by bacteria.
- Infection spreads rapidly as the gases produced by bacteria expand and effect healthy tissue.
- Gas gangrene is caused by environmental bacteria; Clostridium perfringens.
- It can also be from; Group A Streptococcus, Staphylococcus aureus & Vibrio vulnificus.
- These Bacteria are mostly found in soil.
- These environmental bacteria enter the muscle through a wound and cause necrotic tissue and powerful toxins.
- These toxins destroy nearby tissue, generating gas at the same time.
- Gas gangrene can cause necrosis, gas production, and sepsis.
- Progression to toxemia and shock is often very rapid.
- Because of its ability to quickly spread to surrounding tissues, gas gangrene should be treated as a medical emergency.
Internal Gangrene
- Strangulated Hernia: A loop of intestine becomes trapped and its blood supply is cut off.
- Volvulus: Twisting of the intestine.
- Intussusception: A portion of the intestine telescopes into another.
- Ischemic Colitis: Reduced blood flow to the colon.
- Acute Mesenteric Ischemia: Blockage of major arteries supplying the intestines.
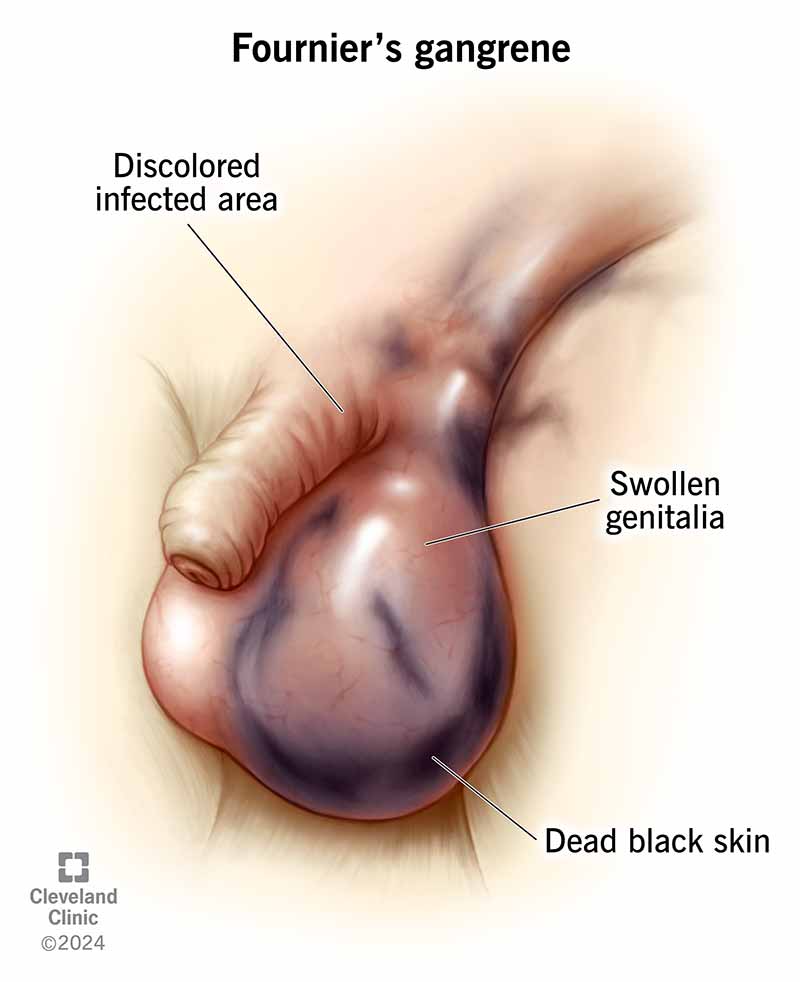
Fournier's Gangrene
Meleney's Gangrene (Progressive Bacterial Synergistic Gangrene)
- Description: A rare, chronic, and progressively spreading necrotizing soft tissue infection, often occurring as a complication of surgery (especially abdominal surgery) or trauma.
- Etiology: Caused by a synergistic infection, typically involving a microaerophilic non-hemolytic Streptococcus and a Staphylococcus aureus.
- Clinical Presentation: Patients develop exquisitely painful, rapidly enlarging skin lesions, often one to two weeks after an operation. The lesion has a characteristic appearance: a central area of necrosis and ulceration surrounded by a purplish zone, which is then surrounded by an outer ring of erythema.
- Management: Requires aggressive debridement and targeted antibiotic therapy.
Risk Factors & Clinical Picture: Who is at Risk and What to Look For
General Risk Factors for Gangrene Development
Any condition that impairs blood flow, compromises the immune system, or increases susceptibility to severe infections can elevate the risk of gangrene.
- Atherosclerosis: Hardening and narrowing of arteries, leading to Peripheral Arterial Disease (PAD).
- Peripheral Arterial Disease (PAD): Critical reduction of blood flow to the limbs.
- Raynaud's Phenomenon: Severe vasoconstriction in fingers and toes, though typically not severe enough to cause gangrene unless prolonged and severe.
- Severe Vasculitis: Inflammation of blood vessels.
- Diabetes Mellitus: A leading cause. Imbalanced blood sugar levels damage blood vessels (micro- and macroangiopathy) and nerves (neuropathy), reducing sensation and blood flow, making feet especially vulnerable to injury and infection.
- Smoking: Significantly damages blood vessels, accelerates atherosclerosis, and reduces oxygen delivery to tissues.
- Obesity: Contributes to diabetes and vascular disease.
- Alcoholism: Can lead to malnutrition and a weakened immune system.
- Intravenous Drug Use (IVDU): Can cause local infections, abscesses, and damage to blood vessels at injection sites.
- Weak Immune System: Conditions like HIV/AIDS, cancer, chemotherapy, or long-term corticosteroid use impair the body's ability to fight infection.
- Serious Injury or Trauma: Crush injuries, deep penetrating wounds, frostbite, severe burns, and scalds can directly damage tissues and blood vessels, leading to ischemia and providing entry points for bacteria.
- Surgery: While rare, can introduce bacteria or compromise blood supply if not managed carefully.
- Direct infection by highly virulent bacteria (e.g., *Clostridium perfringens*, Group A Streptococcus) can cause gangrene even in initially healthy tissue, particularly in necrotizing fasciitis.

Signs and Symptoms: Recognizing the Clinical Presentation
Symptoms typically begin suddenly and can worsen rapidly, especially in wet or gas gangrene. Clinical presentation varies by type but generally includes:
- Pain: Moderate to severe pain, which can be disproportionate to the visible injury (especially in gas gangrene or necrotizing fasciitis). Pain may initially be dull or aching, progressing to intense, throbbing, or burning.
- Skin Discoloration:
- Dry Gangrene: Initial pallor, progressing to dull red, purple, then ultimately black, resembling mummified tissue.
- Wet/Gas Gangrene: Initial pallor or bronze discoloration, rapidly progressing to dark red, purplish, or black.
- Swelling (Edema): Progressive and often rapid swelling around the affected area. The tissue may feel tense and firm.
- Blisters/Bullae: Formation of vesicles or large bullae (blisters) filled with brown, foul-smelling, or serosanguineous (blood-tinged) fluid.
- Foul Odor: A putrid, sweetish, mousy, or decaying smell emanating from the affected tissue, particularly in wet and gas gangrene due to bacterial activity.
- Skin Breakdown: Ulceration, sloughing of skin, and visible decay.
- Crepitus: A palpable crackling or crunching sensation when the affected area is pressed, indicating the presence of gas in the subcutaneous tissues (a hallmark of gas gangrene).
- Fever: Moderate to high-grade fever, often accompanied by chills and rigors.
- Tachycardia: Rapid heart rate.
- Tachypnea: Rapid breathing.
- Hypotension: Low blood pressure, especially as sepsis progresses to septic shock.
- Diaphoresis: Profuse sweating.
- Altered Mental Status: Confusion, disorientation, stupor, or delirium, progressing to coma in severe cases.
- Oliguria/Anuria: Decreased or absent urine output due to kidney injury.
- Nausea, Vomiting, Abdominal Pain: If internal organs are affected.
- General Malaise: Feeling unwell, weakness, fatigue.
Diagnostics: Confirming the Diagnosis and Guiding Treatment
Diagnosis of gangrene is primarily clinical, but diagnostic tests are crucial for confirming the type, identifying the causative organism, assessing the extent of tissue damage, and guiding treatment.
- Complete Blood Count (CBC): Marked leukocytosis (elevated white blood cell count) with a left shift is typical, indicating bacterial infection. Anemia may also be present.
- Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Procalcitonin levels can also be useful in assessing the severity of bacterial infection.
- Blood Cultures: To identify bacteremia and systemic infection. Crucial for guiding systemic antibiotic therapy.
- Electrolytes, Renal Function Tests (BUN, Creatinine): To assess for fluid and electrolyte imbalances and kidney injury, especially with sepsis.
- Liver Function Tests (LFTs): To assess for liver involvement.
- Blood Glucose: Especially important for diabetic patients to assess control.
- Gram Stain of Fluid/Tissue Aspirate: Rapid identification of bacterial morphology (e.g., Gram-positive rods suggestive of Clostridium).
- Aerobic and Anaerobic Tissue/Fluid Culture and Sensitivity: Definitive identification of causative organisms and their susceptibility to antibiotics. This is critical for targeted therapy.
- Plain X-rays: Can reveal gas in soft tissues (subcutaneous emphysema), especially useful for suspected gas gangrene. May also show foreign bodies or underlying bone involvement (osteomyelitis).
- Ultrasound: Can show fluid collections, tissue edema, and sometimes gas. Also useful for assessing blood flow (Doppler ultrasound).
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images, clearly delineating the extent of soft tissue involvement, fascial plane involvement, and the presence and distribution of gas. Essential for pre-surgical planning.
- Magnetic Resonance Imaging (MRI): Offers superior soft tissue contrast, invaluable for assessing muscle involvement, edema, and differentiating between viable and non-viable tissue. Can be particularly useful for identifying necrotizing fasciitis early.
- Angiography (CT Angiography, MR Angiography, Conventional Angiography): To visualize arterial blood flow and identify blockages in cases of suspected dry gangrene or critical limb ischemia, guiding revascularization procedures.
Management of Gangrene
Managing necrotizing infections like gangrene requires a multi-faceted approach, integrating medical, surgical, and comprehensive nursing interventions. Historically, methods like maggot therapy (biodebridement) were used for necrotic tissue. While largely superseded by antibiotics, maggot therapy has seen a resurgence in specific chronic wound care cases due to its efficacy in consuming only devitalized tissue.
I. Medical & Surgical Management (Collaborative Care)
A. On Admission & Initial Assessment:
- Patient Placement: Admit to a surgical ward; consider isolation precautions (e.g., contact precautions) if the infection is highly virulent or there's significant exudate/drainage. Barrier nursing principles are paramount to prevent cross-contamination.
- Positioning: Position the patient for comfort and to optimize circulation to unaffected areas. Elevate affected limbs if swelling is present, unless contraindicated by arterial insufficiency. Frequent repositioning is essential to prevent pressure injuries.
- Vital Signs & General Observation: Obtain and meticulously record baseline vital signs (temperature, pulse, respiration, blood pressure, oxygen saturation). Observe for signs of systemic infection (JACCOLD: Jaundice, Anemia, Cyanosis, Clubbing, Oedema, Lymphadenopathy, Dehydration – though for acute infection, focus more on fever, tachycardia, tachypnea, hypotension, altered mental status). Assess for signs of sepsis and septic shock.
- Intravenous Access: Establish immediate IV access for fluid resuscitation, antibiotic administration, and other necessary medications, according to physician's orders.
- Pain Assessment: Perform a comprehensive pain assessment using an appropriate pain scale.
B. Investigations:
Prompt diagnostic testing is crucial for identifying the causative organism and assessing the extent of systemic involvement.
- Wound Culture & Sensitivity: Aspirate fluid or tissue from the wound for Gram stain, aerobic and anaerobic culture, and sensitivity testing to guide targeted antibiotic therapy.
- Blood Cultures: Obtain blood cultures (typically two sets from different sites) to identify bacteremia and potential sepsis.
- Imaging Studies:
- X-ray: To determine the presence of gas (crepitus/bubbles) in soft tissues (suggestive of gas gangrene) or bone involvement (osteomyelitis).
- CT/MRI: Provide more detailed visualization of soft tissue involvement, extent of necrosis, and gas patterns.
- Hematological Studies:
- Complete Blood Count (CBC): To assess for leukocytosis (elevated WBC count, indicating infection), anemia (due to chronic disease or blood loss), and platelet count.
- Coagulation Profile (PT/INR, PTT): To assess clotting status, especially in severe sepsis or disseminated intravascular coagulation (DIC).
- C-Reactive Protein (CRP) & Erythrocyte Sedimentation Rate (ESR): Inflammatory markers indicating systemic inflammation.
- Biochemical Studies:
- Electrolytes, Renal Function Tests (BUN, Creatinine): To monitor for fluid and electrolyte imbalances and assess kidney function, especially with antibiotic use or sepsis.
- Liver Function Tests (LFTs): To assess for liver involvement/damage.
- Blood Glucose: Especially important for diabetic patients, as hyperglycemia can worsen infections.
- Type & Crossmatch: Prepare for potential blood transfusions to correct anemia or support hemodynamic stability, especially in severe cases or impending surgery.
C. Treatment (Pharmacological & Surgical):
- Antibiotic Therapy:
- Administer broad-spectrum antibiotics intravenously immediately after cultures are drawn, without waiting for results. Examples include high-dose penicillin (e.g., Penicillin G 2.4 million units IV q4-6h) for clostridial infections, along with synergistic agents like clindamycin to inhibit toxin production.
- Cephalosporins (e.g., ceftriaxone), fluoroquinolones (e.g., ciprofloxacin), and metronidazole (for anaerobic coverage, typically 500mg IV q6-8h) are often part of combination therapy, tailored to suspected pathogens.
- Antibiotics alone are often insufficient because they may not adequately penetrate ischemic or necrotic muscles.
- Antitoxins: In specific cases (e.g., gas gangrene caused by *Clostridium perfringens*), antitoxin administration may be considered, though its efficacy is debated and it's less commonly used than antibiotics.
- Analgesia: Aggressive pain management is crucial. Administer analgesics as prescribed, such as diclofenac 75mg IM, or opioids like tramadol IV or IM, titrated to effect. Consider patient-controlled analgesia (PCA) for severe pain.
- Blood Transfusion: Administer packed red blood cells as indicated to correct anemia and improve oxygen-carrying capacity, especially in hemodynamically unstable patients.
- Surgical Intervention:
- Emergent Debridement: The most critical intervention. Surgical debridement to remove all necrotic, infected tissue is often life-saving. This involves extensive incision and drainage to establish a larger wound opening for aeration (as many causative bacteria are anaerobic) and promote drainage. Repeat debridements may be necessary.
- Amputation: If the limb is extensively gangrenous, non-viable, or threatening the patient's life due to uncontrolled infection, amputation (surgical removal of the limb) may be necessary to prevent further spread and save the patient's life.
- Revascularization: For arterial gangrene, restoring blood flow to the affected area (e.g., bypass surgery, angioplasty) is the best treatment option, as it addresses the underlying ischemia. This may precede or follow debridement depending on the clinical situation.
- Hyperbaric Oxygen Therapy (HBOT): Administration of 100% oxygen at increased atmospheric pressure. This can inhibit the growth of anaerobic bacteria, enhance the killing power of phagocytes, and promote angiogenesis and wound healing. It's often used as an adjunctive therapy, particularly in gas gangrene.
II. Nursing Diagnoses & Interventions
A. Impaired Tissue Integrity (Related to necrotic tissue, infection, impaired circulation)
- Wound Care & Debridement Assistance:
- Assist physician/surgeon with debridement procedures (surgical, mechanical, enzymatic, autolytic).
- Perform meticulous wound care with strict aseptic technique (medical and surgical asepsis). Ensure all equipment and linens are autoclaved and sterile.
- Irrigate wounds as prescribed (e.g., with normal saline, hydrogen peroxide for specific anaerobic infections).
- Apply prescribed dressings (e.g., moist-to-dry, specialized antimicrobial dressings, negative pressure wound therapy [NPWT]).
- Observe the wound closely for bleeding, oozing, increased exudate, foul odor, changes in color, and signs of spreading infection (e.g., cellulitis, crepitus). Document findings thoroughly.
- Monitor drainage and secretions. Implement appropriate isolation precautions (e.g., contact precautions) based on institutional policy and pathogen.
- Educate patient and family on proper hand hygiene and avoiding contamination of the wound.
- Circulatory Management:
- Elevate affected limb if edema is present (unless contraindicated by arterial disease) to promote venous return.
- Assess peripheral pulses, capillary refill, skin color, and temperature regularly in the affected and unaffected limbs.
- Avoid restrictive clothing or bedding that could impede circulation.
- Nutritional Support: Ensure adequate protein, calorie, vitamin (especially C and A), and mineral (zinc) intake to promote wound healing. Consult with a dietitian.
B. Acute Pain (Related to tissue damage, surgical incisions, infection)
- Pain Assessment & Management:
- Regularly assess pain intensity, characteristics, and location using an appropriate pain scale (e.g., 0-10 numeric scale).
- Administer prescribed analgesics proactively and on a schedule, rather than waiting for severe pain. Utilize a multimodal approach (e.g., opioids, NSAIDs, adjuncts).
- Evaluate the effectiveness of pain medication and adjust as needed in collaboration with the physician.
- Teach and encourage non-pharmacological pain relief methods (e.g., relaxation techniques, guided imagery, distraction, repositioning, application of heat/cold if appropriate and safe).
- Comfort Measures:
- Ensure patient is in a comfortable position, using pillows for support.
- Maintain a quiet and calming environment. Minimize unnecessary disturbances.
C. Risk for Infection / Sepsis (Related to invasive procedures, compromised immune status, necrotic tissue)
- Infection Control:
- Adhere to strict hand hygiene before and after all patient contact and procedures.
- Maintain sterile technique for all invasive procedures (e.g., dressing changes, IV insertion, catheterization).
- Monitor for signs of systemic infection (fever, chills, tachycardia, hypotension, altered mental status, increased WBC count).
- Administer prescribed antibiotics on time and monitor for adverse effects.
- Maintain meticulous Foley catheter care (if applicable) to prevent urinary tract infections.
- Ensure proper care of all IV lines to prevent phlebitis or line infections.
- Fluid & Electrolyte Balance: Monitor intake and output, urine specific gravity, and electrolyte levels. Administer IV fluids as prescribed to maintain hydration and perfusion.
- Early Ambulation: Encourage early mobilization as tolerated to prevent complications like pneumonia and deep vein thrombosis (DVT), which can worsen systemic compromise.
D. Disturbed Sleep Pattern (Related to pain, hospital environment, anxiety)
- Environmental Modifications:
- Optimize sleep environment: dim lights, control noise on the ward (e.g., wear soft-soled shoes, lower voices, prompt treatment of alarms).
- Bundle nursing care to minimize nighttime interruptions.
- Comfort & Relaxation:
- Administer pain medication before sleep if pain is a factor.
- Offer warm beverages (if allowed), back rubs, or a quiet conversation.
- Suggest relaxation techniques or play soft, calming music for those who find it helpful.
- Daytime Activities: Encourage appropriate daytime activity and exposure to natural light to help regulate circadian rhythm.
E. Self-Care Deficit (Related to pain, weakness, impaired mobility)
- Hygiene & Personal Care:
- Assist with daily bed baths or showers as tolerated. Maintain personal hygiene.
- Perform oral care at least twice daily, or more frequently if patient is NPO or has a dry mouth.
- Provide meticulous skin care, especially for pressure areas, by repositioning every 2 hours and using pressure-relieving devices.
- Elimination: Ensure regular bowel and bladder elimination. Offer bedpan/urinal frequently or assist to commode/bathroom as mobility allows. Monitor for constipation or urinary retention.
- Encourage Independence: Promote patient independence in self-care activities as much as possible to foster a sense of control and recovery.
III. Long-Term Management & Discharge Planning
A. Patient Education:
Comprehensive patient and family education is vital for successful recovery and prevention of recurrence.
- Medication Compliance: Emphasize the importance of completing the full course of antibiotics, even if symptoms improve, to prevent antibiotic resistance and recurrence.
- Wound Care at Home: Provide clear, step-by-step instructions (and demonstration) on wound care, dressing changes, and signs of infection to report immediately.
- Activity Restrictions: Explain any activity restrictions or limitations on the affected limb/area.
- Nutrition: Reinforce the importance of a balanced diet to support healing.
- Recognition of Complications: Educate on signs and symptoms of potential complications (e.g., worsening infection, fever, increasing pain, changes in wound, signs of sepsis) and when to seek immediate medical attention.
- Lifestyle Modifications: Discuss management of underlying conditions (e.g., strict glycemic control for diabetics, smoking cessation for PVD).
B. Follow-up Care:
- Schedule follow-up appointments with the surgeon, wound care specialist, and primary care provider.
- Arrange for home health nursing services if indicated for complex wound care or continued monitoring.
- Provide contact information for emergencies and questions.
IV. Potential Complications
Close monitoring for and prompt intervention against complications are essential for positive patient outcomes.
- Disfiguring or disabling, permanent tissue damage (e.g., loss of limb function, scarring).
- Osteomyelitis (bone infection).
- Recurrence of infection.
- Sepsis: Life-threatening organ dysfunction caused by a dysregulated host response to infection.
- Septic Shock: Sepsis with persistent hypotension requiring vasopressors and elevated lactate.
- Acute Kidney Injury/Failure (due to sepsis or nephrotoxic medications).
- Liver damage/Jaundice (due to sepsis, severe infection, or certain medications).
- Disseminated Intravascular Coagulation (DIC).
- Acute Respiratory Distress Syndrome (ARDS).
- Stupor
- Delirium
- Coma
- Chronic pain.
- Impaired mobility and functional limitations requiring rehabilitation.
- Psychological distress (anxiety, depression, body image issues).
Natural Body Defence Mechanism
Topic 3.10 / 3.11: Natural Body Defence Mechanism
The human body possesses a sophisticated array of natural defense mechanisms designed to protect against pathogens (e.g., bacteria, viruses, fungi) and foreign substances, as well as to repair damaged tissues. These defenses can be broadly categorized into non-specific (innate) defenses and specific (adaptive) defenses.
I. Non-Specific (Innate) Defenses:
These are the body's first line of defense, providing immediate, general protection against a wide range of threats without prior exposure. They do not differentiate between types of pathogens.
- Skin: Intact skin acts as a formidable physical barrier, preventing pathogen entry. It also produces antimicrobial peptides and has a slightly acidic pH (acid mantle) which inhibits bacterial growth.
- Mucous Membranes: Line all body cavities open to the exterior (respiratory, gastrointestinal, genitourinary tracts). They trap pathogens with sticky mucus and often contain antimicrobial substances.
- Cilia: Hair-like projections in the respiratory tract that sweep mucus and trapped pathogens upwards for expulsion (e.g., coughing, sneezing).
- Normal Flora (Microbiota): Non-pathogenic microorganisms colonizing various body surfaces (skin, gut, vagina) that compete with pathogens for nutrients and space, often producing inhibitory substances.
- Body Secretions:
- Tears & Saliva: Contain lysozyme, an enzyme that breaks down bacterial cell walls.
- Gastric Acid: Highly acidic environment in the stomach destroys most ingested pathogens.
- Urine: The acidic pH and flushing action help prevent bacterial colonization of the urinary tract.
- Vaginal Secretions: Acidic pH inhibits the growth of many pathogens.
- Cerumen (Earwax): Traps particles and contains antimicrobial properties.
If pathogens breach the first line, the second line of defense activates, involving cellular and chemical responses.
- Phagocytes: Specialized white blood cells that engulf and digest foreign particles and pathogens.
- Neutrophils: Abundant, early responders to infection, highly phagocytic.
- Macrophages: Develop from monocytes, larger and longer-lived, act as "clean-up crews" and antigen-presenting cells.
- Natural Killer (NK) Cells: Lymphocytes that non-specifically kill virus-infected cells and cancer cells by inducing apoptosis (programmed cell death).
- Inflammatory Response: A localized tissue response to injury or infection, characterized by redness (rubor), heat (calor), swelling (tumor), and pain (dolor). Its purpose is to:
- Prevent spread of damaging agents.
- Dispose of cell debris and pathogens.
- Set the stage for repair.
Key chemical mediators like histamine and prostaglandins cause vasodilation and increased capillary permeability.
- Antimicrobial Proteins:
- Interferons (IFNs): Proteins released by virus-infected cells that protect neighboring uninfected cells from viral replication.
- Complement System: A group of plasma proteins that, when activated, enhances inflammation, promotes phagocytosis (opsonization), and directly lyses (bursts) bacterial cells.
- Fever: Systemic response to infection, raising body temperature. Moderate fever can:
- Inhibit the growth of some microorganisms.
- Increase metabolic rate, speeding up repair processes.
- Enhance phagocytic activity.
II. Specific (Adaptive) Defenses:
This is the body's third line of defense, which is highly specific, systemic, and has memory. It targets specific pathogens and improves with each subsequent exposure.
- Specificity: Recognizes and targets specific antigens.
- Memory: Remembers previous encounters with pathogens, allowing for a faster and stronger response upon re-exposure.
- Systemic: Not restricted to the initial infection site.
- Lymphocytes:
- B Lymphocytes (B cells): Responsible for humoral immunity. They produce antibodies that circulate in bodily fluids and target extracellular pathogens (e.g., bacteria, toxins).
- T Lymphocytes (T cells): Responsible for cellular immunity. They directly attack infected cells, cancer cells, or foreign cells. Types include:
- Helper T cells (CD4+): Coordinate both humoral and cellular immunity.
- Cytotoxic T cells (CD8+): Directly kill target cells.
- Regulatory T cells: Suppress immune responses to prevent autoimmunity.
- Antigen-Presenting Cells (APCs): Cells (e.g., macrophages, dendritic cells) that present antigens to T cells, initiating an adaptive immune response.
- Antibodies (Immunoglobulins): Proteins produced by plasma cells (differentiated B cells) that bind specifically to antigens, marking them for destruction.
- Active Immunity: Develops when the body produces its own antibodies or activated T cells in response to an antigen.
- Naturally acquired active immunity: Infection (e.g., getting sick with measles).
- Artificially acquired active immunity: Vaccination (e.g., MMR vaccine).
- Passive Immunity: Occurs when antibodies are transferred from one individual to another. Provides immediate but temporary protection as the body does not produce its own memory cells.
- Naturally acquired passive immunity: Antibodies passed from mother to fetus via placenta or to infant via breast milk.
- Artificially acquired passive immunity: Injection of pre-formed antibodies (e.g., antivenom, rabies immunoglobulin).
Interrelationship of Defenses:
It's crucial to understand that these defense mechanisms do not operate in isolation. Innate defenses provide immediate protection and also activate and guide the more specific adaptive immune responses. For example, inflammation helps to bring immune cells to the site of infection, and macrophages (innate) can act as APCs, linking to adaptive immunity. A healthy immune system relies on the coordinated action of all these components.
INFLAMMATION
Inflammation is part of the body's immune response to irritation, injury, or infection. Inflammation is a defensive mechanism in the body. Inflammation is a defensive reaction intended to neutralize, control or eliminate the offending agent and to prepare the site for repair.
It can be beneficial when, for example, your knee sustains a blow and tissues need care and protection. However, sometimes, inflammation can persist longer than necessary, causing more harm than benefit.
Cells or tissues of the body may be injured or killed by any of the agent (physical, chemical, infections) when this happens, an inflammatory response (inflammation) naturally occurs in healthy tissues adjacent to the site of injury.
Note: inflammation is not the same as infection, an infectious agent is only one of several agents that may trigger an inflammatory response. An infection exist when the infectious agent is living, growing and multiplying in the tissues and is able to overcome the body’s normal defense.
Inflammation differs from antibody mediated immunity and cell mediated immunity (AMI and CMI) in two important ways:
- Inflammatory protection is immediate but short term. It does not provide true immunity on repeated exposure to the same organisms.
- Inflammation is a non-specific body defense to invasion or injury and can be started quickly by almost any event, regardless of where it occurs or what causes it.
Functions of inflammation
- When something harmful or irritating affects a part of our body, there is a biological response to try to remove it. The signs and symptoms of inflammation can be uncomfortable but are a show that the body is trying to heal itself.
- Cells of inflammation or tissues of the body may be injured or killed by any of the agents (physically chemical, infectious) when this happens an inflammatory response (inflammation) naturally occurs in the healthy tissues adjacent to the site of injury.
- It provides immediate protection against the effects of tissue injury and invading foreign proteins.
- Inflammation also helps start both antibodies mediated and cell mediated actions to activate full immunity.
- It can be a barrier to prevent organisms from entering the body or can be an attacking force that eliminates organisms that have already entered the body.
- This type of immunity cannot be transferred from one person to another and is not an adaptive response to exposure or invasion by foreign proteins.
- The inflammatory response are part of innate immunity and other parts of innate immunity include;- This is the body’s ability to resist invading organisms and It is achieved through natural barriers, biologically functionally and chemically using:
- The skin as a barrier,
- Mucus to trap organisms,
- mucus membranes as a barrier
- Biological agents like normal flora
- Functional like taking a lot of fluids to flash
- Chemical secretions like tears to clear away
- Cell mediated like lymphocytes or antibodies
CELL TYPES INVOLVED IN INFLAMMATION
The leukocytes (white blood cells) involved in inflammation are neutrophils, macrophages, eosinophil’s and basophils. An additional cell type important in inflammation is the tissue mast cell. Neutrophils and macrophages destroy and eliminate foreign invaders. Basophils, Eosinophil’s and mast cells release chemicals that act on blood vessels to cause tissue level responses that help neutrophil and microphage actions.
NEUTROPHILS
- Mature neutrophils make up between 55% and 70% of the normal total white blood cell count.
- Neutrophils come from the stem cells and complete the maturation process in the bone marrow.
- They are also called granulocytes because of the large number of granules present inside each cell; other names of neutrophils are based on their appearance and maturity.
- Mature neutrophils are also called segmented neutrophils because of their nuclear shape.
- Usually, growth of a stem cell into a mature neutrophil requires 12 to 14 days.
- In a healthy person with full immunity, more than 100 billion fresh, mature neutrophils are released from the bone marrow into the circulation daily.
- This huge production is needed because the life span of each neutrophil is short about 12 to 18 days.
- Neutrophil function provides protection after invaders especially bacteria enter the body. This powerful army of small cells destroys invaders by phagocytosis and enzymatic digestion, although each cell is small and can take part in only one episode of phagocytosis.
MACROPHAGE
- Macrophage come from the committed myeloid stem cells in the marrow: and form the mono nuclear phagocyte system.
- The stem cells first form monocytes which are released into the blood stream at this stage until they mature. Monocytes have limited activity.
- Most monocytes move from the blood into the body tissues where they mature into macrophage.
- Some macrophages become fixed in position within the tissues whereas others can move within and between tissues.
- The liver, spleen and intestinal tract within large numbers of these cells.
FUNCTIONS
- Macrophage protects the body in several ways;-
- These cells are important in immediate inflammatory responses and also stimulate the longer-lasting immune responses of antibody mediated immunity and cell mediated immunity.
- Macrophage functions include phagocytosis, repair antigen presenting and secretion of cytokines for the immune system control.
BASOPHILS
- Basophils come from myeloid stem cells and make up only about 1% of the total circulating white blood cell count.
- These cells cause the manifestation of inflammation.
Functions
- Basophils act on blood vessels and release chemicals which include;- heparin, histamine, serotonin, kinins and leukotriene’s.
- Basophils have sites that bind the portion of immune-globulin E (IgE) molecules which binds to and is activated by allergens.
- When allergens bind to the IgE on the basophils, the basophils membrane opens and releases the vaso-active amines into the blood, where most of them act on smooth muscle and blood vessel walls.
- Heparin inhibits blood and proteins clotting.
- Histamine constricts small veins inhibiting blood flow and decreasing venous return.
- This effect causes blood to collect in capillaries and arterioles.
- Kinins dilate arterioles and increase capillary permeability.
- These actions cause blood plasma to leak into the interstial space.
EOSINOPHILS
- These come from the myeloid line and contain many vaso-active chemical.
Functions
- Eosinophil’s are very active against infestations on rurastic larvae and also limits inflammatory reaction.
- The eosinophil granules contain many different substances; some are enzymes that degrade the vaso-active chemicals released by other leukocytes.
TISSUE MAST CELLS
- These cells have functions very similar to basophils and eosinophils. Although mast cells do originate in the bone marrow, they come from different parent cells than leukocytes and do not circulate as mature cells.
- Instead they differentiate and mature in tissues especially those near blood vessels, nerves, lung tissues skin and mucous membranes.
- Some mast cells also respond to the inflammatory products made and released by T. lymphocytes.
The tissue mast cells have important roles in maintaining and prolonging inflammatory and hypersensitivity reactions.
STAGES/ PHASES OF INFLAMMATION
Injury
- Any type of injury of exogenous (outside the body) or endogenous (inside the body) injury can initiate the inflammatory y response; heat cold, radiations, chemicals, trauma infections, immunological injuries, neoplasms etc.
- Whatever the stimulus the response itself is the same but the degree of response varies with the type and severity of the injury.
Vascular response
- The vascular response consists of transitory vasoconstriction followed by immediate vasodilation. This reaction is due to chemical mediators such as histamine, serotonin or kinins being released at the site of infection or injury.
- The mediator cause increase in blood flow to the area causing redness and heat.
- They also cause increased permeability of the capillaries which increase blood flow to the interstitial space. The extra fluid dilutes toxins and microorganism the area and serves as a vehicle by which phagocytes and nutrients needed for healing to reach the injured site.
Fluid exudation
- Fluid exudation from the capillaries into the interstitial spaces begins immediately and is most active during the first 24hours after.
- The exudate is serous fluid but the capillary walls become more permeable and proteins are lost into the interstitial spaces causing increased pressure in this space which encourages tissue swelling and oedema.
Cellular exudation
- It occurs when WBCS are summoned to the vessels in the affected area as a result of the release of chemostastic substance from injured cells and activation of complement.
- WBCS adhere to the capillary walls and migrate through the walls. Neutrophils are the first to respond usually within first few hours.
- Neutrophils ingest dead tissue cells and then die, releasing proteolytic enzyme that liquefy the dead neutrophils, dead bacteria and other dead cells forming pus.
Healing
The inflammatory response contains the spread of bacteria and prepares tissue for healing by two overlapping process: reconstruction and maturation. For repair to proceed, acute inflammation must subside and pus and dead tissue must be removed. Repair of wound involves three processes:
- Filling in the wound
- Sealing the wound
- Shrinking the wound
Reconstruction
- Once the inflamed area is clean or debrided, reconstruction begins and new cells are produced to fill in the space left by the injury.
- Fibroblast is attracted to the area which secret fibrin – a thread like structure that encircles the space.
Maturation
- Maturation follows reconstruction phase, during maturation which can last for months to years, scar is remodeled. Capillaries contract leaving a vascular scar and structure and function of damaged tissue are restored.
Types of inflammation
There are three main types of inflammation and its categorized by its duration and the type of exudate produced.
- Acute inflammation
- Chronic inflammation
- Sub-acute inflammation
ACUTE INFLAMMATION
An acute inflammation is one that starts rapidly and becomes severe in a short space of time. Signs and symptoms are normally only present for a few days but may persist for a few weeks in some cases.
The 5 Cardinal Signs (PRISH):
- Pain: The inflamed area is likely to be painful, especially during and after touching.
- Redness: This occurs because the capillaries in the area are filled with more blood than usual.
- Immobility: There may be some loss of function in the region of the inflammation.
- Swelling: This is caused by a buildup of fluid.
- Heat: More blood flows to the affected area, and this makes it feel warm to the touch.
Causes of Acute Inflammation
- Burns
- Chemical irritants
- Frostbite
- Toxins
- Infection by pathogens
- Physical injury, blunt or penetrating
- Immune reactions due to hypersensitivity
- Radiation
- Foreign bodies, including splinters, dirt and debris
- Trauma
Examples of diseases, conditions, and situations that can result in acute inflammation include:
- acute bronchitis
- infected ingrown toenail
- a sore throat from a cold or flu
- a scratch or cut on the skin
- high-intensity exercise
- acute appendicitis
- dermatitis
- tonsillitis
- infective meningitis
- sinusitis
- a physical trauma
CHRONIC INFLAMMATION
This refers to long-term inflammation and can last for several months and even years. It can result from:
- Failure to eliminate whatever was causing an acute inflammation.
- An autoimmune disorder that attacks normal healthy tissue.
- Exposure to a low level of a particular irritant, such as an industrial chemical, over a long period.
Examples of diseases and conditions that include chronic inflammation:
- Rheumatoid arthritis
- Asthma
- Chronic peptic ulcer
- Tuberculosis
- Periodontitis
- Ulcerative colitis and Crohn's disease
- Sinusitis
- Active hepatitis
| Acute | Chronic | |
|---|---|---|
| Caused by | Harmful bacteria or tissue injury | Pathogens that the body cannot break down, including some types of virus, foreign bodies that remain in the system, or overactive immune responses |
| Onset | Rapid | Slow |
| Duration | A few days | From months to years |
| Outcomes | Inflammation improves, turns into an abscess, or becomes chronic | Tissue death and the thickening and scarring of connective tissue |
Management of Inflammation
Investigation
- White blood cell count
- Bacteriological examination of specimen got from the site of infection.
- Serum tests for the presence of antibodies.
Common treatments
- Simple measures like fluid intake and rest can be considered to aid resolution.
- Antibiotics may be given to combat infection.
- Rest of the affected part.
- Surgical interventions may be necessary if all fails, excision and removal of necrotic tissue can be done.
- Incision and drainage may be done to drain pus.
- Rehabilitation is done to restore the functions.
Anti-inflammatory medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) can be taken to alleviate the pain caused by inflammation. Examples of NSAIDs include naproxen, ibuprofen, and aspirin.
- Acetaminophen, such as paracetamol or Tylenol, can reduce pain without affecting the inflammation.
- Corticosteroids, such as cortisol, are a class of steroid hormones that prevent a number of mechanisms involved in inflammation.
Inflammation diet
There are several foods that can have been shown to help reduce the risk of inflammation, including:
- olive oil, tomatoes, nuts, leafy greens, fatty fish, fruit.
Avoid eating foods that aggravate inflammation, including:
- fried foods, white bread, soda and sugary drinks, red meat, Margarine.
Natural Body Defence Mechanism Read More »
Aseptic technique & Special investigations in surgical nursing
Topic 3.7: Aseptic Technique & Special Investigations
Sub-topic 3.7.3: Aseptic Technique / Surgical Asepsis
Introduction to Surgical Asepsis
- It is defined as the absence of micro-organisms that can cause disease.
- Surgical asepsis promotes tissue healing by determining pathogens from coming into contact with the surgical wound.
- Practices that suppress, reduce and inhibit injection processes are known as aseptic technique.
- Surgical asepsis prevents contamination of surgical wounds.
- All members of the operating theatre (OR) team are responsible for strict adherence to aseptic techniques.
- It is essential that OR nurses acquire a surgical conscience – vigilant adherence to aseptic technique throughout the entire peri-operative period.
Operating Theatre Environment and Asepsis
The purpose of maintaining asepsis in the operating theatre is paramount. The theatre environment should have the following:
- Air conditioned ventilation.
- Charnel enclosure for orthopedic work.
- Easily cleanable fabric.
- A one way traffic circulation from clean area to dirty area.
- Adequate shower facilities for medical staff after finishing a day’s operation.
Basic Rules of Surgical Asepsis in the OR
-
Scrubbed persons function within sterile field
Scrubbed personnel wear gloves and gowns at the surgical field. The gown of scrubbed team member is considered sterile in front, from the chest to the level of the sterile field and the sleeves are sterile front two inches above the elbow to the stockinette cuff. The non-sterile areas of the gowns include; stockinet cuff, neckline, shoulder, axillary region and back. Dressing in OR attire proceeds from head to toe.
-
Sterile drapes are used to create a sterile field
Sterile drapes are placed on the patient equipment and furniture used within the sterile field. Draped tables are sterile only at the table level; items extending over the table edge are contaminated. Handling of the drapes should be minimized.
-
All items used in the sterile field are sterile
If the sterility of an item is questioned, it must be considered unsterile. Packaging materials must guarantee that items will remain sterile until removed.
-
Supplies introduced into the sterile field
Are delivered in a manner that ensures the sterility of the item and maintains the integrity of the sterile field. The nurse opens a sterile package from the far side first and near side last and holds the wrapper tails when the item is presented to the sterile field. The nurse pours solutions carefully to avoid splashing liquids on to the field. After opening a bottle of a sterile solution, the nurse must present the entire contents to the sterile field or discard it.
-
Maintenance and monitoring of sterile field
The possibility for contamination increases with time, therefore the sterile field should be established as close to the time of use as possible. Un-attended sterile field is considered contaminated.
-
The integrity of the sterile field must be maintained by individuals moving within or around the sterile field
Only scrubbed personnel touch and reach over sterile areas. Sterile persons remain close to the sterile field and never turn their backs to it. Sterile individuals change positions by passing back to back or face to face. Un-scrubbed personnel only touch and reach over non-sterile areas, do not walk between sterile fields and approach sterile fields by facing them.
SURGICAL ASEPSIS
- It is defined as the absence of micro-organisms that can cause disease.
- Surgical asepsis promotes tissue healing by determining pathogens from coming into contact with the surgical wound.
- Practices that suppress, reduce and inhibit injection processes are known as aseptic technique.
- Surgical asepsis prevents contamination of surgical wounds.
- All members of the operating theatre (OR) team are responsible for strict adherence to aseptic techniques.
- It is essential that OR nurses acquire a surgical conscience – vigilant adherence to aseptic technique throughout the entire peri-operative period.
The purpose of maintaining asepsis, operating theatre. They should have the following;
- Air conditioned ventilation.
- Charnel enclosure for orthopedic work.
- Easily cleanable fabric.
- A one way traffic circulation from clean area to dirty area.
- Adequate shower facilities for medical staff after finishing a day’s operation.
Client Preparation for Surgery
Although much preparation have taken place prior to clients transfer to the surgical department additional activities such as shaving and positioning may be performed.
Skin preparation
The goal of skin preparation is to reduce the risk of post-operative wound infection by;
- Removing transient microbes from the skin
- Reducing the resident microbes count to sub-pathogenic amounts
- Inhibiting rapid rebound growth of microbes
The skin is prepared by mechanically scrubbing or cleaning around the surgical site with anti-microbial agents. If the patient is very hairy or if the hair will interfere with the surgical procedure, the nurse removes it; usually either wet shaving, clippers or use of depilatory agent. The area is then scrubbed in a circular motion. The principal of scrubbing from the clean area (site of incision) to the dirty area (periphery) is observed at all times. A liberal area is cleansed to allow added protection and unexpected occurrences during the procedure. After preparation of the skin, the sterile members of the surgical team drape the area. Only the site to be incised is left exposed.
Positioning the patient
- It is a critical part of every procedure and usually follows administration of the anesthesia.
- Anesthetist will indicate when to begin the positioning.
- The circulating nurse ensures optimal positioning and continually assess the client.
- The position of the patient should allow accessibility to the operative site, administration and monitoring of anesthetic agents and maintenance of the patient’s airway.
- Improper positioning would potentially result into muscle strain, joint damage and other unwanted effects.
- It is a nurse’s responsibility to secure the extremities provide adequate padding and support and obtain sufficient physical or mechanical help to avoid unnecessary straining of self or patient frequently.
Positions used frequently include;
- The surprise position: it is used for many abdominal surgeries, thoracic surgeries and some surgeries on the extremities
- The semi-sitting up position: it is used for surgeries on the thyroid and neck areas
- The prone position: it is used for spinal fusions and removal of hemorrhoids
- The lateral chest position: it is used for gynecological, perinea or rectal surgeries
- The jackknife: it is used for proctologic and some spinal surgeries
- The Trendelenburg position: it is used for examinations and for performing abdominal surgeries
- Lateral position: it is used for surgeries of the anal area
NB: see positions in medical surgical nursing (patient centered collaborative care 8th edition)
Anesthesia
The term anesthesia is derived from the word anesthesis meaning “no sensation” therefore anesthesia is limited or total loss of feeling (normal sensation) with or without loss of consciousness. There are two broad classifications of anesthesia; general and local anesthesia.
General Anesthesia
Involves unconsciousness, complete insensitivity to pain, amnesia, motionless and muscle relaxation. It involves four overlapping stages i.e. induction (going to sleep), maintenance, emergence (waking up) and recovery.
- Induction time period starting with pre-operative medication, initiation of appropriate IV access, application of monitors, initiation of sequence of medication that render the patient unconscious, securing airway, drugs used include; benzodiazepines, narcotics, hypnotics and volatile gases.
- Maintenance-time period during which the surgical procedures is performed, patient remains in an unconscious state with appropriate measures to ensure safety of the airway. Drugs are the same as above.
- Emergence-time – it is a period during which the surgical procedure is completed. Patient is prepared for return to return to consciousness and removal of airway assist devices. Drugs used; reversal agents – anticholinergic, sympathometics, narcotic, antagonists, benzodiazepines antagonist.
- Recovery-time / period during which the patient regains his/her clear thinking ability. This often takes longer with some residual thinking difficulty persisting for several days or even weeks. Many anesthetic drugs are metabolized slowly. The speed of metabolism depends on amount of drug given, the length of surgery and how deeply the patient is breathing.
Local Anesthesia
Allows operative procedures to be performed on a particular part of the body without loss of consciousness or sedation. The duration of action of the local anesthetic frequently carries into the post-operative period providing continued analgesia.
The disadvantages
- Inadvertent IV administration producing hypotension and potential seizures
- Inability to precisely match the duration of action of the agents administered to the duration of surgical procedure
- Technique difficulty and discomfort that may be associated with infections
Methods of administration
- Topical application – application of the agent directly to the skin, mucous membranes or open surface
- Local infiltration – injection of the agent into the tissues through which the surgical incision will pass
- Regional nerve block – injection of the agent into or around a specific nerve or group of nerves. Examples of spinal anesthesia (injection of the agent into CSF found in the subarachnoid space, usually below L2 ) and epidural black (injection of agent epidural space via either a thoracic or lumber approach)
Conscious sedation
A minimally depressed level of consciousness with maintenance of patient’s protective airway, reflexes. Its primary goal is to reduce the patient’s anxiety and discomfort and to facilitate cooperation. Often a combination of sedative. The anesthetist determines the choice and method of administering the anesthesia according to;
- Patient’s preferences, age, physical status and emotional status
- Type and length of the surgical procedure
- Patient’s positioning during surgery
- Co-existing disease
NB: operating theatre nurses do not administer anesthetic agents but they must understand the various anesthetics used in surgery and the potential side effects and complications (check pharmacology). This knowledge enables the nurse to plan intra-operative nursing care to assist the anesthesia team.
Sub-topic 3.7.4: Special Investigations in Surgical Nursing
Special investigations are diagnostic procedures used to confirm or rule out a surgical condition, determine the extent of disease, and plan for surgery. The nurse plays a vital role in patient preparation, education, and post-procedure care.
X-ray & Contrast Studies
The X-ray has been called one of the most significant advances in medical history. Routine X-rays involve exposing a body part to a small dose of radiation to produce an image of an internal organ. It is a fast and easy procedure. Patients will experience no discomfort or side effects from their examination and are allowed to leave immediately following their X-ray test.
General Preparation of Patients for X-rays
- Explain to the patient what is going to happen. This is especially necessary for x-rays which are done in a darkened room e.g. barium meal.
- Remove jewellery e.g. necklaces for a chest X-rays.
- Take the patient to the X-ray room, in a chair, or on a stretcher, or walking as ordered by the doctor, and bring with you the patient’s chart and previous x-rays, if any.
- On arrival, remove the patient’s clothing and put on an X-rays gown.
Contrast Studies
- Esophagram (Barium Swallow): An examination of the pharynx and oesophagus using still and fluoroscopic X-ray images, after the patient drinks a barium solution.
- Upper GI Series: A series of X-rays of the oesophagus, stomach, and small intestine taken after the patient drinks a barium solution.
- Small Bowel or Small Intestine Series: A series of X-rays of the part of the digestive tract that extends from the stomach to the large intestine.
- Barium Enema / Lower GI Series: A series of X-rays of the lower intestine (colon) and rectum taken after the patient is given an enema with a barium solution.
- Intravenous Pyelogram (IVP): An X-ray examination of the kidneys, their drainage to the bladder, and the bladder, using an injected contrast dye.
- Hysterosalpingogram: X-ray of the uterus and Fallopian tubes; usually done in diagnosing infertility.
- Arthrogram: X-ray of a joint after the injection of a contrast medium.
Advanced Imaging Techniques
MRI (Magnetic Resonance Imaging)
MRI is a method of obtaining detailed pictures of internal body structures without the use of radiation. It uses a magnetic field and radio waves. The patient will hear a repeated drum-like knocking sound as the scans are recorded. High quality images require the patient to lie still.
How to Prepare For the MRI Exam
- Patient wears loose, comfortable clothing without metal snaps or zippers.
- Patient goes with a referral form from the doctor.
- If the patient is having an MRI of the abdomen performed, advise the patient not to eat or drink anything after midnight the night before your procedure.
CT (Computed Tomography)
CT scanning is a rapid, painless diagnostic examination that combines X-rays and computers to see the location, nature, and extent of many different diseases or abnormalities.
HOW to Prepare For the CT Exam
- The meal prior to your CT examination should consist of CLEAR liquids ONLY.
- If oral contrast (barium drink) is required, specific instructions on when to drink it will be given (e.g., TWO HOURS BEFORE and ONE HOUR BEFORE the appointment).
Nuclear Imaging
This provides information about both structure and function by using safe and painless techniques to image the body and treat disease. It involves introducing a small amount of a radioactive chemical (radionuclide or radiotracer) into the body.
- PET/CT: Combines Positron Emission Tomography (PET) with CT to identify areas of abnormal metabolic activity, often used in cancer diagnosis and staging.
- SPECT/CT: Combines Single-Photon Emission Computed Tomography (SPECT) with CT for similar purposes.
Common Nuclear Scans
- Bone Scan: A radionuclide collects in areas of high bone activity (fractures, infection, cancer), seen as 'hot spots'.
- Cardiac Scan: Assesses blood flow to the heart muscle.
- Renal Scan, Hepatobiliary Scan, etc.
Preparation for Nuclear Medicine Exams
Preparation varies. Some scans require no prep (Bone Scan), while others require fasting (Cardiac Scan, PET/CT). Patients must inform staff if they are diabetic or pregnant.
Endoscopy
Endoscopy means looking inside and typically refers to looking inside the body for medical reasons using an endoscope, an instrument used to examine the interior of a hollow organ or cavity of the body. Unlike most other medical imaging devices, endoscopes are inserted directly into the organ.
Components of an Endoscope:
- A rigid or flexible tube
- A light delivery system
- A lens system
- An eyepiece
- An additional channel to allow entry of medical instruments or manipulators
Uses (Examples by Body System):
- GI Tract: Esophagogastroduodenoscopy (EGD), Colonoscopy, ERCP.
- Respiratory Tract: Rhinoscopy, Bronchoscopy.
- Urinary Tract: Cystoscopy.
- Joints: Arthroscopy.
Preparation and Risks
Preparation usually involves fasting to ensure the organ is empty. Risks, though infrequent, include infection, perforation (a tear) of the organ lining, and bleeding.
Advanced Imaging Techniques
MRI (Magnetic Resonance Imaging)
Magnetic Resonance Imaging (MRI) is a method of obtaining detailed pictures of internal body structures without the use of radiation or radioactive substances of any kind.
This is accomplished by placing the patient in a magnetic field while radio waves are turned on and off.
This causes the body to emit its own weak radio signals which vary according to tissue characteristics.
These signals are then picked up by a sensitive antenna and fed to a computer which produces detailed images of the body for interpretation by trained radiologists.
During the examination the patient will not feel anything unusual. He/she will, however, hear a repeated drum-like knocking sound as the scans are recorded. The patient is free to bring a favourite CD or cassette tape to listen to during the scan to make her/himself comfortable. Hearing protection are provided to those patients who do not wish to listen to music.
To produce high quality images, the patient has to lie still during the examination while breathing normally. The average scan takes 5 to 15 minutes—the complete examination about 30 to 45 minutes—during which time several dozen images will be produced.
How to Prepare For the MRI Exam
- Patient wears loose, comfortable clothing without metal snaps or zippers.
- Patient goes with a referral form from the doctor.
- If the patient is having an MRI of the abdomen performed, advise the patient not to eat or drink anything after midnight the night before your procedure.
CT (Computed Tomography)
Computed Tomography (CT) scanning is a rapid, painless diagnostic examination that combines X-rays and computers.
A CT scan allows the radiologist to see the location, nature, and extent of many different diseases or abnormalities inside your body.
HOW to Prepare For the CT Exam
The meal prior to your CT examination should consist of CLEAR liquids ONLY. (You may have coffee/tea WITHOUT milk; broth; soda; and grape, cranberry or apple juice.)
If you are having an out patient, provide the barium drink to the patient to take home. The patient SHOULD NOT REFRIGERATE the barium drink.
TWO (2) HOURS BEFORE THE SCHEDULED APPOINTMENT
- The patient removes cap and drinks the liquid within 30 minutes to the first designated line on the container.
ONE (1) HOUR BEFORE THE SCHEDULED APPOINTMENT
- Drink the liquid within 30 minutes to the 2nd designated line on the container.
REMAINDER OF LIQUID
- THE patient brings the remainder of the liquid to the hospital.
- The patient will finish drinking the liquid when the study begins.
- Prescription medications may be taken as usual.
- EXCEPTION: Do not take Glucophage.
Nuclear Imaging
Nuclear Medicine provides doctors with information about both structure and function by using safe and painless techniques to image the body and treat disease. It is a superior way to gather medical information that would otherwise be unavailable or require surgery.
Nuclear Imaging now offers two of the most advanced nuclear imaging modalities for the early detection of disease: PET/CT and SPECT/CT.
PET/CT
PET/CT is a state-of-the-art technique that combines Positron Emission Tomography (PET) with Computed Tomography (CT) to image tissue and organ function. This scan is designed to accurately identify even small areas of abnormal metabolic activity, which are associated with several disease processes. PET/CT’s major clinical impact to date is in cancer diagnosis and staging; however, PET/CT is also a useful modality for imaging the heart and brain. PET/CT can show more than just where tumours are located. PET/CT can reveal whether lesions are benign or malignant and can assess the effectiveness of treatment, whether surgery, chemotherapy, or radiation therapy.
When the patient arrives at the Nuclear Imaging Suite, a technologist will discuss the PET/CT procedure with him/her and ask if s/he has any questions. When the patient is ready for the PET/CT scan, s/he will have the blood sugar tested. Next, most patients will receive an oral contrast (barium drink). An IV will then be started, and s/he will receive an injection of a small amount of safe, radioactive sugar (radiotracer). The patient will then be asked to wait very quietly in a seated area. Any activity, even talking or gum chewing, may affect the results of the test. Prior to the scan, the patient will be asked to empty his/her bladder.
The patient will lie on a bed that passes slowly through the scanner. For scanning purposes, it is important that the patient lies quietly and remain still on the bed during the scan. The length of time between scans can vary depending on the body areas being studied, typically between 30 to 60 minutes. The patient should plan to spend approximately three hours total time at the Nuclear Imaging Suite for the entire PET/CT procedure.
How to Prepare For the PET/CT Exam
- Refrain from eating for at least six hours prior to the exam since the results of the test are affected by the blood sugar level.
- It is important to be well hydrated for the test, so please make sure that the patient drinks plenty of water beginning the day before the exam up to the appointment time.
- Do not perform any heavy lifting or exercising the day before or the day of the PET/CT scan.
- If the patient is diabetic, please notify the technologist so that s/he may administer special instructions to you as necessary prior to the PET/CT scan.
- It is also recommended that the patient wears comfortable clothing.
SPECT/CT
SPECT/CT is an advanced medical imaging technology that combines Single-Photon Emission Computed Tomography (SPECT) with Computed Tomography (CT) to enable physicians to detect heart disease, cancer and other diseases earlier and target treatments with greater precision.
SPECT, like Positron Emission Tomography (PET), is a nuclear medicine exam that allows direct visualization of tissues, tumours and organs, such as the heart. SPECT/CT system allows physicians to obtain more detailed information and increased image clarity in a single, non-invasive procedure than is possible through separate procedures. The system detects changes in patients’ molecular activity – before structural changes become visible – and combines this information with precise anatomical detail obtained through CT technology to pinpoint the location of abnormal tissue.
When the patient arrives at the Nuclear Imaging Suite, a technologist will discuss the SPECT/CT procedure with him/her and ask ifs/he has any questions. Then a small amount of radiopharmaceuticals will be introduced into the body by injection, swallowing or inhalation. The radiopharmaceuticals are attracted to specific organs, bones or tissues. The amount of radiopharmaceuticals used for the patient’s exam will be carefully determined to provide the least amount of radiation exposure and to ensure an accurate test.
The scanner then creates images of the area being examined and identifies “hot spots” that indicate the location and extent of disease, such as the increased metabolic activity characteristic of cancer. The combination of high-resolution CT through the SPECT/CT allows physicians to accurately localize these hot spots and make a definitive diagnosis.
How to Prepare For the Nuclear Medicine Exam
- Bone Scan
- The patient may eat and drink prior to his/her scan.
- Please do not schedule an X-ray barium study on the same day as the patient’s Bone Scan.
- You may schedule a CT exam on the day of the patient’s Bone Scan.
- If the patient had a Barium Enema (BE) a day or two before the scheduled appointment time, an X-ray may be taken to make sure that the barium is all out of the system.
- Cardiac Scan
- Please do not eat or drink after midnight, the day before the Cardiac Scan.
- At the time of scheduling your exam, the patient will be told whether or not s/he will receive Persantine during the exam. If the patient will be receiving Persantine, let him/her not ingest caffeine for 24 hours prior to the exam.
- The doctor will advise the patient of which medications s/he may and may not take the morning of exam.
- Hepatobiliary: Please do not eat or drink after midnight, the day before the scan.
- Gastric Emptying: Please do not eat or drink after midnight, the day before your scan.
- Brain: There is no preparation for this exam. The doctor will advise the patient of which medications s/he may and may not take the morning of exam.
- Parathyroid: There is no preparation for this exam.
- Renal Scan: There is no preparation for this exam.
Ultrasound
Ultrasound uses sound waves to obtain a medical image or picture of various organs and tissues in the body. It is a painless and safe procedure. Ultrasound produces very precise images of the soft tissues (heart, blood vessels, uterus, bladder, etc.) and reveals internal motion such as heart beat and blood flow. It can detect diseased or damaged tissues, locate abnormal growths and identify a wide variety of changing conditions, which enable the doctor to make a quick and accurate diagnosis.
What will the exam be like?
A technologist will assist the patient onto the examination table. At this time, a water-based transmission gel will be applied to the area of the body that will be examined. A transducer will be moved slowly over the body part being imaged. The transducer sends a signal to an on-board computer which processes the data and produces the ultrasound image. It is from this image that the diagnosis is made.
The patient won’t feel a thing except for the slight pressure and movement of the transducer over the part of the body being imaged. It is important that the patient remains still and relaxed during the procedure. The ultrasound images will appear on a monitor similar to a TV screen and will be recorded either on paper or film for a detailed study.
How to prepare for The Ultrasound exam of the pelvis
Eat meals - DO NOT FAST! Drink 32 ounces of clear liquids (no soda) one hour and 15 minutes prior to the time of the appointment. (All of the liquid is to be in your system one hour before the appointment so that the bladder will be full.) DO NOT EMPTY the bladder until the study has been completed or the patient has spoken with a technologist.
How to prepare for The Ultrasound exam for pregnancy, kidneys, and bladder
- Eat meals - DO NOT FAST! Drink 20 ounces of water one hour and 15 minutes prior to the time of the appointment.
- Continue as above
How to Prepare For the Ultrasound Exam of the Abdomen
- Do not eat or drink anything after midnight the night before the procedure.
Bone Density (DEXA)
Bone Densitometry is a fast, safe and painless test that uses advanced technology called DEXA (Dual Energy X-Ray Absorptiometry) to measure symptoms of osteoporosis -- such as low density and mineral content of bone -- that may have developed unnoticed over many years. Because osteoporosis can result in bone fractures that can cause chronic pain, disability and loss of independence, it is important to begin treating osteoporosis at an early stage. Bone densitometry can detect the early signs of osteoporosis so that patients can begin treating it before a debilitating fracture occurs.
During a comprehensive DEXA bone evaluation, a patient lies comfortably on a padded table while the DEXA unit scans one or more areas of his/her body, usually the spine or hip because they are particularly prone to fracturing.
When the exam is complete, the patient’s images are sent to a computer and analyzed. They are then given to a radiologist, a physician who specializes in the diagnostic interpretation of medical images. After the study has been reviewed, the doctor will receive a report of the findings. This report will include patient’s bone mineral density (BMD), along with the FRAX (Fracture Risk Assessment Tool) results. The radiologist will use the FRAX assessment tool, developed by the World Health Organization, to obtain two results, expressed as percentages. These numbers are a ten-year probability of hip fracture and ten-year probability of a major osteoporotic fracture (clinical spine, forearm, hip or shoulder fracture).
Digital Mammography
A mammogram is a safe low-dose X-ray procedure that takes pictures of the internal tissues of the breasts. This simple exam is performed as a screening or diagnostic study, to determine the possibility of irregularities within the breast. It can reveal areas too small or deep to feel, which may or may not require further investigation. Digital Mammography is the most advanced diagnostic technology available for the early detection of breast cancer.
What are the benefits of Digital Mammography?
There are numerous benefits to digital mammography. For the patient, digital mammograms are faster. The test is "filmless," so nothing has to be developed. Images are read on a monitor and stored electronically in the PACS (Picture Archiving and Communications System). For the radiologist, digital mammograms provide more comprehensive visibility. Calcifications can be enhanced or magnified on the screen to aid the radiologist in interpreting whether or not the calcifications are suspicious. That is good news for younger women and those who have dense breasts. Digital mammography units are also able to accommodate women with larger breasts. This means fewer images and less radiation for these patients.
Radionuclide (Isotope) Scan
A radionuclide scan is a way of imaging bones, organs and other parts of the body by using a small dose of a radioactive chemical. A radionuclide (sometimes called a radioisotope or isotope) is a chemical which emits a type of radioactivity called gamma rays. A tiny amount of radionuclide is put into the body, usually by an injection into a vein. (Sometimes it is breathed in, or swallowed, depending on the test.)
Gamma rays are detected by a device called a gamma camera. The computer builds a picture by converting the differing intensities of radioactivity emitted into different colours or shades of grey. Areas of the target organ or tissue which emit lots of gamma rays may be shown as red spots ('hot spots'). Areas which emit low levels of gamma rays may be shown as blue ('cold spots').
Are there any risks with radioisotope scans?
The term 'radioactivity' may sound alarming. But, the radioactive chemicals used in radionuclide scans are considered to be safe, and they leave the body quickly in the urine. The dose of radiation that your body receives is very small. However:
- As with any other types of radiation (such as X-ray), there is a small risk that the gamma rays may affect an unborn child. So, tell your doctor if you are pregnant or if you may be pregnant.
- Rarely, some people have an allergic reaction to the injected chemical. Tell your doctor if you are allergic to iodine.
Endoscopy
Endoscopy means looking inside and typically refers to looking inside the body for medical reasons using an endoscope, an instrument used to examine the interior of a hollow organ or cavity of the body. Unlike most other medical imaging devices, endoscopes are inserted directly into the organ.
Risks
- Infection
- Punctured organs
- Over-sedation
The main risks are perforation, or a tear, of the stomach or oesophagus lining and bleeding. Although perforation generally requires surgery, certain cases may be treated with antibiotics and intravenous fluids. Bleeding may occur at the site of a biopsy or polyp removal. Seldom does surgery become necessary.
After the Endoscopy
After the procedure the patient will be observed and monitored by a qualified nurse in the endoscopy room or a recovery area until a significant portion of the medication has worn off. Occasionally the patient is left with a mild sore throat, which may respond to saline gargles, or chamomile tea. The patient may have a feeling of distention from the insufflate air that was used during the procedure. Both problems are mild and fleeting. When fully recovered, the patient will be instructed when to resume their usual diet.
Aseptic technique & Special investigations in surgical nursing Read More »
EMPHYSEMA / PULMONARY EMPHYSEMA
EMPHYSEMA / PULMONARY EMPHYSEMA
Introduction
Definition: Emphysema is a chronic and progressive lung disease primarily characterized by the destruction and enlargement of the air sacs (alveoli) at the end of the smallest airways (bronchioles) in the lungs. This damage leads to a significant reduction in the surface area available for gas exchange, resulting in chronic and progressively worsening difficulty breathing.
More specifically, emphysema is a pathological diagnosis that affects the air spaces distal to the terminal bronchiole. It is defined by an abnormal, permanent enlargement of the air spaces, accompanied by the destruction of their walls without obvious fibrosis. This destruction of the lung parenchyma leads to a loss of elastic recoil, increased air trapping, thoracic over-distention (hyperinflation), and often, a compromised function of the diaphragm. While sputum accumulation can be present, it is more characteristic of chronic bronchitis, which often coexists with emphysema.
Pulmonary emphysema is a major component and a progressive form of Chronic Obstructive Pulmonary Disease (COPD). The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines COPD as "a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases."
NB: Emphysema, Chronic Bronchitis, and Asthma (when overlapping with persistent airflow limitation) are the primary disease entities that fall under the umbrella term of COPD.
Pathology (Pathophysiology)
The core pathological process in emphysema involves the irreversible breakdown of the elastic fibers and walls of the alveoli, which are the tiny air sacs responsible for gas exchange. This destruction leads to the coalescence of smaller air sacs into larger, irregularly shaped, and less efficient air spaces. The process unfolds as follows:
- Alveolar Destruction and Enlargement: The delicate walls separating individual alveoli are progressively destroyed. This leads to the formation of fewer, but much larger, air-filled spaces. These enlarged spaces, often referred to as bullae if they are greater than 1 cm in diameter, have significantly reduced surface area for the efficient exchange of oxygen into the blood and carbon dioxide out of it.
- Loss of Elastic Recoil: The lung tissue, particularly the elastic fibers that normally allow the lungs to recoil and expel air during exhalation, are damaged or lost. This loss of elasticity means that air becomes trapped within the enlarged air spaces, leading to hyperinflation of the lungs.
- Air Trapping: Due to the loss of elastic recoil and the destruction of alveolar walls, air becomes trapped in the lungs, particularly during exhalation. This increases the residual volume and functional residual capacity, leading to a perpetually overinflated chest.
- Bronchiolar Collapse: The small airways (bronchioles) that lead to the alveoli are also affected. Due to the loss of surrounding parenchymal support and elastic recoil, these airways tend to collapse prematurely during exhalation, further contributing to air trapping.
- Inflammation and Protease-Antiprotease Imbalance: The primary trigger for this destructive process is chronic exposure to irritants, most notably cigarette smoke. These irritants activate an inflammatory response in the lungs. Inflammatory cells (e.g., neutrophils, macrophages) release proteolytic enzymes, particularly neutrophil elastase, which are capable of breaking down elastic fibers and connective tissue in the lung. Normally, the lungs are protected by anti-proteases, such as alpha-1 antitrypsin (AAT). However, in individuals exposed to smoke, the activity of these protective anti-proteases is overwhelmed or directly inhibited by components of cigarette smoke. This imbalance between proteases and anti-proteases leads to the unchecked destruction of the alveolar walls and the breakdown of elastic tissue and collagen.
- Impaired Gas Exchange: The loss of alveolar tissue drastically reduces the surface area available for gas exchange. Additionally, the destruction of the capillary beds surrounding the alveoli (which are part of the alveolar wall) leads to reduced blood flow through the pulmonary capillary system. This combined effect severely impairs the transfer of oxygen into the blood and the removal of carbon dioxide.
- Permanent Damage: The damage to the alveolar structures and elastic tissue is permanent and irreversible. While interventions can manage symptoms and slow progression, the ability to breathe properly cannot be fully restored once this destruction has occurred.
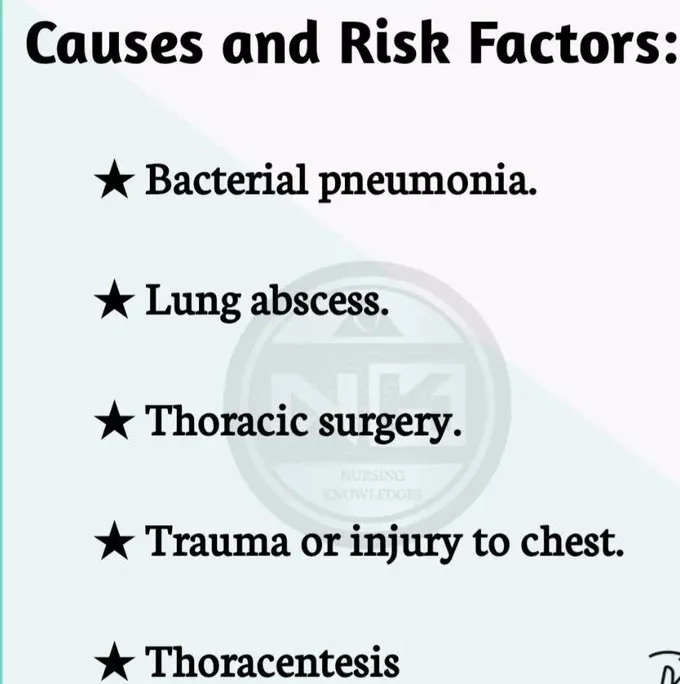
Causes of Emphysema
Emphysema is predominantly caused by long-term exposure to inhaled irritants, with genetic factors playing a significant role in susceptibility for some individuals.
- Occupational Dusts: Such as coal dust (in coal miners), grain dust, cotton dust, and silica.
- Chemical Fumes: Exposure to cadmium, isocyanates, and other industrial chemicals.
- Indoor Air Pollution: Smoke from biomass fuels (e.g., wood, animal dung) used for cooking and heating in poorly ventilated homes, particularly common in developing countries.
- Outdoor Air Pollution: Chronic exposure to high levels of urban air pollution, including particulate matter and ozone.
Contributory Risk Factors (can exacerbate or increase susceptibility)
- Bronchial Asthma: While distinct, severe, chronic, or poorly controlled asthma can lead to airway remodeling and contribute to fixed airflow obstruction, sometimes blurring the lines with COPD, especially "asthma-COPD overlap syndrome."
- Aging: As people age, natural changes occur in the lung structure, including a decrease in elastic recoil, which can make them more susceptible to emphysema.
- Infections: Frequent respiratory infections can accelerate lung damage in susceptible individuals.
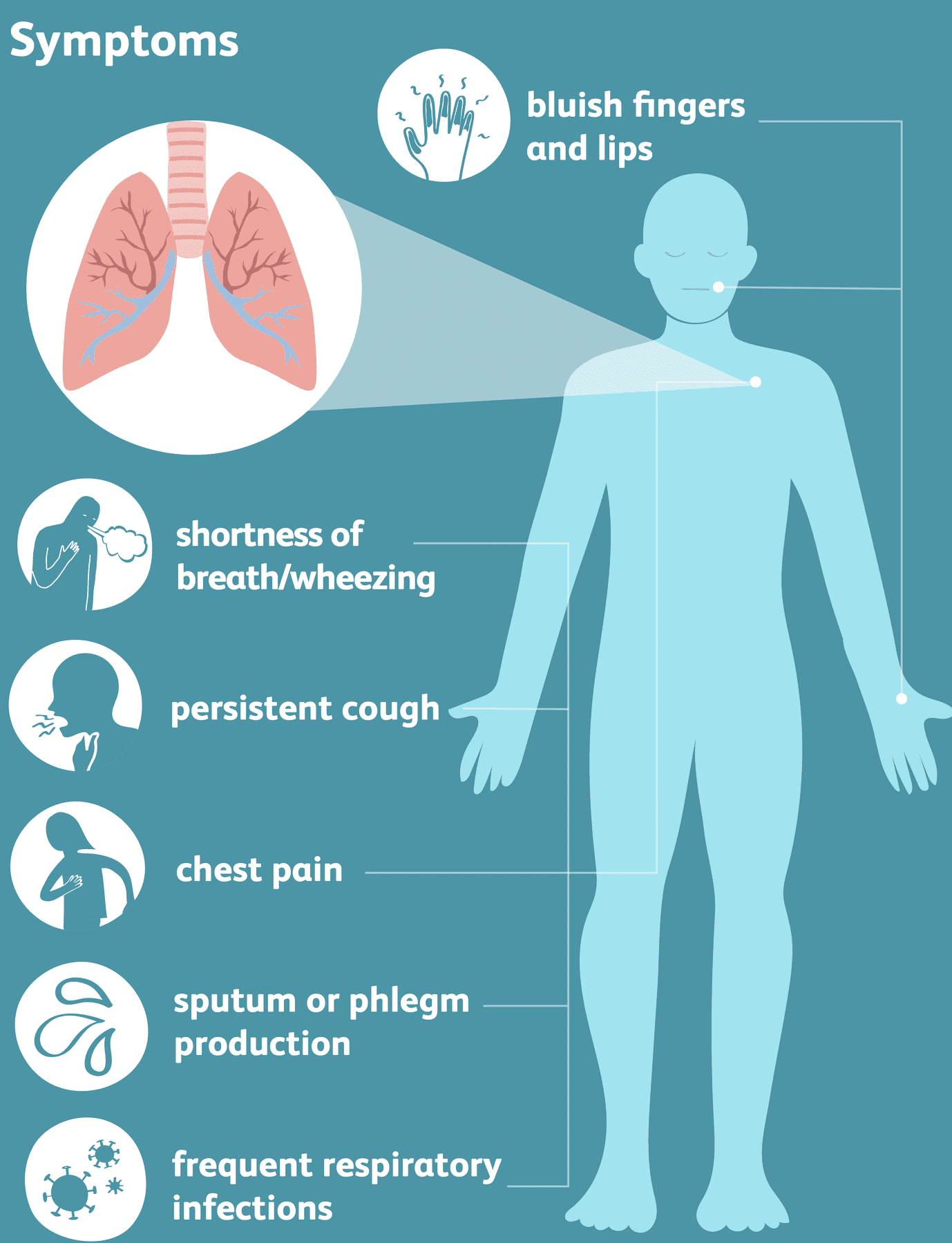
Signs and Symptoms of Emphysema
The symptoms of emphysema typically develop gradually over many years and progressively worsen. They reflect the impaired gas exchange and increased work of breathing.
- Dyspnea (Shortness of Breath): This is the hallmark symptom and is typically progressive. Initially, it may only occur during physical exertion, but as the disease advances, it becomes noticeable even with minimal activity or at rest. Patients often report feeling "air hungry."
- Chronic Cough: While more characteristic of chronic bronchitis, a persistent cough, which may or may not be productive of sputum, can also be present in emphysema, particularly if bronchitis coexists.
- Wheezing: A whistling sound during breathing, caused by narrowed airways.
- Frequent Lung Infections: Due to impaired mucociliary clearance and damaged lung tissue, individuals with emphysema are more susceptible to recurrent respiratory infections (e.g., bronchitis, pneumonia).
- Weight Loss: Significant weight loss can occur due to the increased energy expenditure associated with the constant work of breathing, reduced appetite, and systemic inflammation.
- Fatigue: Chronic dyspnea, increased work of breathing, hypoxemia, and sleep disturbances contribute to profound fatigue.
- Cyanosis: Bluish discoloration of the skin, lips, or nail beds, indicating insufficient oxygen in the blood. This is a sign of advanced disease.
- Anxiety and Depression: The chronic, debilitating nature of the disease, coupled with the constant struggle for breath and fear of suffocation, often leads to significant psychological distress.
- Sleep Problems: Dyspnea, coughing, and hypoxemia can disrupt sleep patterns, leading to insomnia or frequent awakenings.
- Morning Headaches: Can be a sign of hypercapnia (high carbon dioxide levels) during sleep due to hypoventilation.
- Barrel Chest: Due to chronic air trapping and hyperinflation, the chest wall may expand, giving it a rounded, barrel-like appearance.
- Pursed-Lip Breathing: A compensatory breathing technique used to create back pressure in the airways, helping to keep them open during exhalation and reduce air trapping.
- Use of Accessory Muscles of Respiration: As the diaphragm's efficiency decreases, patients may rely on neck and shoulder muscles (e.g., sternocleidomastoid, scalenes) to assist with breathing.
Management of a Patient with Emphysema
The management of emphysema is focused on relieving symptoms, slowing disease progression, preventing and treating complications, and improving the patient's quality of life. As emphysema is irreversible, the goal is not a cure but effective disease management.
Aims of Management
- To optimize respiratory function and restore the best possible breathing pattern.
- To prevent or minimize the frequency and severity of acute exacerbations.
- To alleviate symptoms such as dyspnea and cough.
- To improve exercise tolerance and overall physical functioning.
- To prevent and manage complications, including infections and heart problems.
- To enhance the patient's quality of life and reduce anxiety/depression associated with the disease.
- To provide education and support for self-management.
General Management and Nursing Interventions
A multi-faceted approach involving medical, nursing, and rehabilitative interventions is crucial.
1. Assessment and Monitoring:
- Admission of the patient to a medical ward, ideally quiet and well-ventilated, to promote rest and reduce environmental irritants.
- Thorough initial assessment of respiratory status: rate, rhythm, depth, use of accessory muscles, breath sounds (e.g., diminished, wheezes, rhonchi), and oxygen saturation (SpO2).
- Regular monitoring of vital observations: temperature, pulse, respiration, and blood pressure. These must be meticulously recorded on the patient's file and trended to identify changes or signs of deterioration (e.g., fever indicating infection, increased respiratory rate, tachycardia).
- Assess for signs of hypoxemia (cyanosis, confusion) and hypercapnia (morning headaches, somnolence, confusion).
- Monitor fluid balance, especially if there is increased insensible loss from tachypnea or if diuretics are used for cor pulmonale.
- Assess nutritional status and provide dietary support if needed.
2. Positioning and Comfort:
- Position the patient in a sitting-up position (e.g., High Fowler's, orthopneic position) to maximize lung expansion and aid breathing by reducing pressure on the diaphragm.
- Provide emotional support and reassurance to allay anxiety, which can worsen dyspnea. Teach relaxation techniques.
3. Oxygen Therapy:
- Administration of supplemental oxygen therapy as prescribed, guided by SpO2 levels and arterial blood gases (ABGs). The goal is to maintain adequate oxygenation (e.g., SpO2 > 90%) while carefully monitoring for CO2 retention, especially in advanced stages (start with low flow rates, e.g., 1-2 L/min, and titrate based on patient response and ABGs). Oxygen therapy helps improve oxygen delivery to the lungs and tissues.
4. Pharmacological Management (Drug Therapy):
- Bronchodilators: These medications relax the smooth muscles of the airways, helping to open them up and reduce bronchospasm. They are typically given via inhalers (nebulizers or metered-dose inhalers with spacers).
- Short-acting beta-agonists (SABAs) e.g., Albuterol (Salbutamol): For quick relief of acute dyspnea.
- Long-acting beta-agonists (LABAs) e.g., Salmeterol, Formoterol: For long-term maintenance.
- Short-acting anticholinergics e.g., Ipratropium: For quick relief.
- Long-acting anticholinergics (LAMAs) e.g., Tiotropium: For long-term maintenance.
- Methylxanthines e.g., Theophylline: Less commonly used due to side effects and narrow therapeutic window, but may be used in some cases.
- Corticosteroids:
- Inhaled Corticosteroids (ICS): Often used in combination with LABAs for patients with frequent exacerbations or significant symptoms, particularly if they have an "asthma-like" component. E.g., Fluticasone, Budesonide.
- Oral Corticosteroids: Used for acute exacerbations to reduce inflammation and improve airflow. E.g., Prednisone. Long-term use is generally avoided due to significant side effects.
- Antibiotics: Prescribed for acute exacerbations if there is evidence of bacterial infection (e.g., increased sputum purulence, fever).
- Diuretics: May be used if the patient develops cor pulmonale with peripheral edema.
- Mucolytics: (e.g., acetylcysteine) May be considered in some patients with very thick, tenacious sputum, although their routine use is debated.
- Alpha-1 Antitrypsin Augmentation Therapy: For patients with documented severe AAT deficiency, intravenous infusion of pooled human alpha-1 antitrypsin can help slow the progression of emphysema.
5. Pulmonary Rehabilitation:
- A comprehensive program that includes exercise training, nutritional counseling, education on lung disease, and psychological support. This significantly improves exercise tolerance, reduces symptoms, and enhances quality of life.
- Physical exercises: Encouraged within the patient's tolerance, such as walking, cycling (stationary bikes). These help the body use oxygen more efficiently, improve muscle strength, and reduce breathlessness.
- Breathing Techniques: Teaching pursed-lip breathing and diaphragmatic breathing can help control dyspnea and improve exhalation.
6. Nutritional Support:
- Patients with advanced emphysema often have increased caloric needs due to the work of breathing but may experience reduced appetite. Nutritional counseling and calorie-dense, small, frequent meals can help prevent weight loss and maintain muscle mass.
7. Surgical Interventions (for select cases):
- Lung Volume Reduction Surgery (LVRS): In highly selected patients with upper lobe emphysema and low exercise capacity, surgical removal of the most diseased parts of the lung can reduce hyperinflation and improve lung function.
- Bullectomy: Surgical removal of large bullae that are not contributing to gas exchange and are compressing healthy lung tissue.
- Lung Transplantation: A last-resort option for very severe emphysema in carefully selected candidates.
Health Education on Emphysema
Comprehensive health education is fundamental to empowering patients to manage their condition effectively, prevent complications, and maintain the best possible quality of life.
- Smoking Cessation: This is the single most important intervention. Emphasize that quitting cigarette smoking (and avoiding all other tobacco products) is crucial to slow the progression of the disease and prevent further lung damage. Provide resources for smoking cessation programs, nicotine replacement therapy, or medications.
- Vaccination: Highly recommended to prevent respiratory infections that can trigger acute exacerbations.
- Annual influenza (flu) immunization.
- Pneumococcal vaccination: Typically, a series of two vaccinations (PCV13 and PPSV23) for adults with chronic lung disease, with specific intervals. (Note: "5 yearly one against pneumonia" is a simplified guideline, and current recommendations for pneumococcal vaccines should be followed).
- COVID-19 vaccination and boosters.
- Pertussis (whooping cough) vaccine.
- Nutritional Guidance: A healthful diet with plenty of fresh fruits, vegetables, whole grains, lean proteins, and a low intake of processed foods, unhealthy fats, and added sugars is necessary. Advise on strategies to manage appetite and maintain weight, such as smaller, more frequent meals.
- Physical Activity and Exercise: Encourage regular, gentle physical exercises within the patient's tolerance (e.g., walking, using stationary bikes, light resistance training). Explain that these help the body use oxygen more efficiently, improve muscle strength, and hence improve breathing and overall well-being. Emphasize the importance of pulmonary rehabilitation.
- Breathing Techniques: Teach and reinforce effective breathing techniques such as pursed-lip breathing (to control breathlessness and prevent airway collapse) and diaphragmatic (abdominal) breathing (to maximize diaphragm efficiency).
- Medication Adherence: Educate on the purpose, correct administration (especially for inhalers), dosage, and potential side effects of all prescribed medications. Emphasize the importance of consistent use of maintenance medications.
- Symptom Recognition and Action Plan: Teach patients to recognize early signs of worsening symptoms or acute exacerbations (e.g., increased dyspnea, increased cough, change in sputum color/volume, fever) and provide a clear action plan on when to contact their healthcare provider or seek emergency care.
- Avoidance of Irritants: Advise avoiding exposure to environmental lung irritants such as secondhand smoke, air pollution, chemical fumes, and strong odors.
- Infection Control: Practice good hand hygiene, avoid crowds during flu season, and manage underlying conditions that increase infection risk.
- Psychological Support: Address anxiety and depression. Encourage open communication, support groups, and professional counseling if needed.
- Follow-up Care: Emphasize that regular follow-up visits with healthcare providers are crucial for ongoing assessment, adjustment of treatment plans, and early detection of complications.
- Energy Conservation Techniques: Advise on strategies to conserve energy and manage daily activities, such as pacing oneself, taking breaks, and using assistive devices if necessary.
Complications of Emphysema
The complications of emphysema range from direct respiratory issues to systemic effects, often progressing in severity as the disease advances.
- Acute Exacerbations of COPD (AECOPD): Emphysema patients are highly susceptible to acute worsening of their symptoms, often triggered by respiratory infections (viral or bacterial) or increased exposure to irritants. These exacerbations can be severe, requiring hospitalization and significantly impacting lung function and quality of life.
- Pneumonia: Due to impaired lung defenses and altered lung architecture, individuals with emphysema are at increased risk of developing bacterial or viral pneumonia, which can be life-threatening.
- Pneumothorax (Collapsed Lung): The destruction of alveolar walls can lead to the formation of large air-filled sacs (bullae). These bullae can sometimes rupture, allowing air to escape into the space between the lung and the chest wall (pleural space), leading to a collapsed lung (spontaneous pneumothorax). This is a medical emergency.
- Bullae: While bullae themselves are part of the emphysematous process, very large bullae can compress healthy lung tissue, further impairing function. They also carry the risk of rupture.
- Pulmonary Hypertension: The chronic hypoxemia (low blood oxygen) in emphysema causes the blood vessels in the lungs to constrict (pulmonary vasoconstriction). This leads to increased pressure in the arteries of the lungs, a condition known as pulmonary hypertension.
- Cor Pulmonale (Right-Sided Heart Failure): Persistent pulmonary hypertension places increased strain on the right side of the heart, which is responsible for pumping blood to the lungs. Over time, this increased workload can cause the right ventricle to enlarge and weaken, leading to right-sided heart failure (cor pulmonale). Symptoms include swelling in the ankles and legs (peripheral edema), jugular venous distension, and liver enlargement.
- Respiratory Failure: In advanced stages or during severe exacerbations, the lungs' ability to adequately oxygenate the blood and remove carbon dioxide becomes severely compromised, leading to acute or chronic respiratory failure. This may necessitate mechanical ventilation or long-term oxygen therapy.
- Polycythemia: Chronic hypoxemia can stimulate the bone marrow to produce more red blood cells (erythrocytosis or polycythemia) as the body attempts to compensate for low oxygen levels. This increases the viscosity (thickness) of the blood, raising the risk of blood clots (e.g., deep vein thrombosis, pulmonary embolism).
- Weight Loss and Malnutrition: The increased metabolic demands from the work of breathing, reduced appetite, and systemic inflammation often lead to unintentional weight loss and muscle wasting.
- Osteoporosis: Patients with emphysema are at higher risk of developing osteoporosis due to chronic inflammation, corticosteroid use, and reduced physical activity.
- Muscle Weakness and Dysfunction: Systemic inflammation and deconditioning contribute to weakness and atrophy of skeletal muscles, further impacting exercise capacity and quality of life.
- Depression and Anxiety: The chronic and debilitating nature of emphysema significantly impacts mental health, often leading to depression and anxiety.
EMPHYSEMA / PULMONARY EMPHYSEMA Read More »
BRONCHITIS
BRONCHITIS
Introduction
Bronchitis is a common respiratory condition characterized by an inflammation of the mucous membranes lining the bronchi. These are the larger and medium-sized airways that serve as critical conduits for airflow, transporting air from the trachea (windpipe) into the more distal and delicate lung parenchyma, where gas exchange occurs. This inflammation leads to a cascade of physiological changes, including swelling, increased mucus production, and irritation of the airways, which collectively impair normal respiratory function.
Types of Bronchitis
Bronchitis is broadly classified based on its duration and clinical presentation into two main categories: acute and chronic.
- Acute Bronchitis:
This form of bronchitis represents a transient inflammation of the large airways of the lung, typically characterized by a sudden and rapid onset of symptoms. It is usually self-limiting, meaning it resolves spontaneously, often within a period of 10 days to 3 weeks, although the associated cough can sometimes persist for several weeks longer. Acute bronchitis is commonly a sequela of an upper respiratory tract infection.
- Chronic Bronchitis:
In contrast, chronic bronchitis is defined by a persistent and recurrent inflammation of the large airways of the lung. Its development is often gradual, and the defining characteristic is a chronic productive cough that lasts for at least 3 months in a year for two consecutive years, in the absence of other underlying lung diseases that could explain the cough. This condition is often a component of Chronic Obstructive Pulmonary Disease (COPD) and is typically associated with long-term exposure to irritants, most notably cigarette smoke.
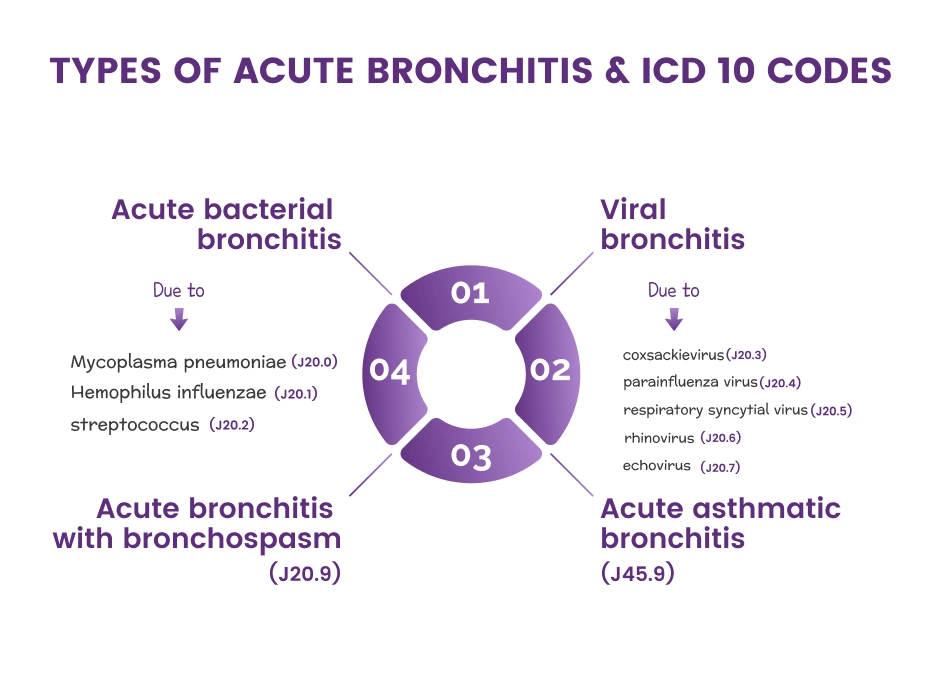
Classification of bronchitis according to cause
Beyond duration, bronchitis can also be classified based on its etiology, distinguishing between infectious and non-infectious triggers.
1. Infectious/Contagious Bronchitis:This type of bronchitis occurs when the inflammation of the bronchi is caused by a living biological agent, or pathogen. These pathogens are transmitted from person to person or from the environment. Common infectious causes include:
- Viral Bronchitis: By far the most common cause, accounting for approximately 90-95% of acute bronchitis cases in healthy adults. Viruses such as Influenza A and B, Parainfluenza, Adenovirus, Respiratory Syncytial Virus (RSV), Rhinovirus, and Coronavirus are frequent culprits.
- Bacterial Bronchitis: Less common in acute settings, but can occur, often as a secondary infection following a viral illness. Common bacterial agents include Mycoplasma pneumoniae, Chlamydophila pneumoniae, Bordetella pertussis (whooping cough), Streptococcus pneumoniae, and Haemophilus influenzae. Bacterial bronchitis may also be seen in chronic bronchitis exacerbations.
- Fungal Bronchitis: Rarer, typically affecting individuals with compromised immune systems (e.g., those with HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapy). Examples include Aspergillus species or Candida species.
This form of bronchitis is not caused by a pathogen and therefore is not transmissible. Instead, it results from exposure to various irritants or other underlying conditions. Common non-infectious causes include:
- Chemical Irritants: Inhalation of toxic fumes, industrial pollutants, strong chemicals (e.g., ammonia, chlorine, sulfur dioxide), or particulate matter can directly irritate and inflame the bronchial lining.
- Environmental Factors: Exposure to high levels of air pollution, smog, dust, or allergens (e.g., pollen, pet dander, mold spores) can trigger an inflammatory response in the airways.
- Allergic Reactions: In susceptible individuals, exposure to specific allergens can induce an allergic bronchial inflammation, sometimes referred to as allergic bronchitis.
- Gastric Reflux: Chronic gastroesophageal reflux disease (GERD) can lead to micro-aspiration of stomach acid into the airways, causing irritation and inflammation, particularly contributing to chronic cough and sometimes chronic bronchitis.
- Drug Side Effects: Certain medications, though less common, can rarely induce a form of bronchitis as a side effect.
- Mechanical Irritation: Prolonged exposure to very cold or very dry air can sometimes cause irritation, particularly in sensitive airways.
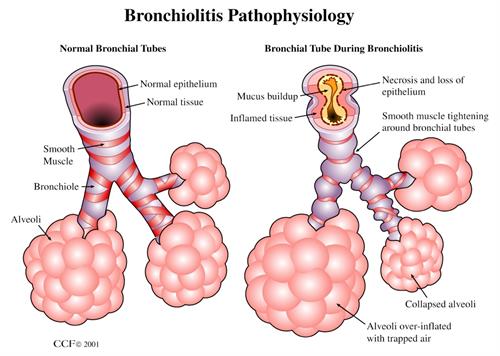
Pathophysiology
The pathophysiological processes underlying acute and chronic bronchitis differ significantly, reflecting their distinct etiologies and clinical courses.
Acute Bronchitis
Acute bronchitis is fundamentally the result of acute inflammation of the bronchi, triggered predominantly by various factors, with viral infections being the most common. Other triggers can include bacterial infections, allergens, environmental pollutants, or even aspiration. The inflammatory process unfolds as follows:
- Initial Irritation and Viral Entry: Typically, a viral upper respiratory infection (URI) precedes acute bronchitis. Viruses replicate in the epithelial cells lining the upper airways and can then spread downwards to the larger bronchi.
- Inflammatory Response: The body's immune system mounts an inflammatory response to the invading pathogen or irritant. This leads to the release of inflammatory mediators (e.g., histamine, prostaglandins, bradykinin).
- Mucosal Changes: The inflammation of the bronchial wall results in:
- Mucosal Thickening and Edema: The lining of the airways swells and becomes thicker due to fluid accumulation, narrowing the bronchial lumen.
- Epithelial-Cell Desquamation: The protective epithelial cells that line the airways are damaged and shed.
- Denudation of the Basement Membrane: In some areas, the underlying basement membrane, which supports the epithelial cells, may become exposed, making the airway more vulnerable to further irritation and infection.
- Increased Mucus Production: Goblet cells within the bronchial lining, and submucosal glands, respond to inflammation by overproducing mucus. This mucus often becomes thicker and stickier.
- Airway Obstruction and Symptoms: The combination of mucosal edema, increased and tenacious mucus, and damaged cilia (tiny hair-like structures that help move mucus) leads to partial airway obstruction. This obstruction and irritation trigger the characteristic symptoms of acute bronchitis:
- Cough: The primary symptom, initially non-productive, but often becoming productive as mucus accumulates.
- Wheezing: Due to narrowed airways.
- Shortness of Breath: In more severe cases.
- Resolution: As the immune system clears the infection and the inflammation subsides, the bronchial mucosa heals, and symptoms resolve. The cough may linger due to persistent airway hyperresponsiveness even after the acute inflammation has resolved.
Chronic Bronchitis
Chronic bronchitis is a progressive inflammatory condition primarily characterized by chronic mucus hypersecretion and structural changes in the airways. It is often a key component of Chronic Obstructive Pulmonary Disease (COPD) and is distinct from acute bronchitis in its chronic, often irreversible nature. The pathophysiology involves:
- Chronic Irritant Exposure: The primary trigger is prolonged and repeated exposure to inhaled irritants, with cigarette smoke being the most significant. Other irritants include industrial dusts, air pollution, and occupational chemicals.
- Goblet Cell Hyperplasia and Hypersecretion: In response to chronic irritation, the number and size of mucus-producing goblet cells in the bronchial lining increase (hyperplasia), and they produce excessive amounts of mucus (hypersecretion). Submucosal glands also enlarge and overproduce mucus.
- Impaired Mucociliary Clearance: The cilia, which are responsible for sweeping mucus and trapped particles out of the airways, become damaged, dysfunctional, or are destroyed by the chronic inflammation and irritant exposure. This impairment leads to mucus stasis, further promoting irritation and susceptibility to infection.
- Inflammatory Cell Infiltration and Mediator Release: The chronic irritation triggers a persistent inflammatory response in the bronchial walls. Various inflammatory cells, including macrophages, neutrophils, and lymphocytes, infiltrate the airway. These cells release a range of pro-inflammatory mediators, such as interleukin-8 (IL-8), tumor necrosis factor-alpha (TNF-α), leukotrienes, and proteases (e.g., elastase from neutrophils). These mediators contribute to ongoing inflammation, tissue damage, and mucus production.
- Imbalance of Regulatory Substances: There is often an associated decrease in the release of regulatory substances that normally protect the airway, such as angiotensin-converting enzyme (ACE) and neutral endopeptidase. This imbalance can exacerbate inflammation and bronchoconstriction.
- Airway Remodeling: Over time, chronic inflammation and irritation lead to structural changes in the airways, known as airway remodeling. This includes:
- Thickening of the bronchial walls due to fibrosis and smooth muscle hypertrophy.
- Narrowing of the small airways, leading to increased airway resistance.
- Loss of elastic recoil in the lungs (if emphysema is also present), further impairing airflow.
- Acute Exacerbations: During an acute exacerbation of chronic bronchitis (AECB), typically triggered by viral or bacterial infections, the bronchial mucous membrane becomes acutely hyperemic (engorged with blood) and edematous. Bronchial mucociliary function is further diminished. This, in turn, leads to a significant increase in airflow impediment because of luminal obstruction to small airways by even more copious and tenacious mucus. The airways become further clogged by cellular debris, inflammatory exudates, and thickened mucus, significantly increasing irritation and worsening symptoms.
- Characteristic Cough: The most characteristic symptom of chronic bronchitis, the persistent productive cough, is directly caused by the copious secretion of mucus that the body attempts to clear from the airways.
Causes of Bronchitis
The causes of bronchitis vary significantly depending on whether it is acute or chronic.
Acute Bronchitis
Acute bronchitis is predominantly caused by infections, usually viral, and is generally self-limiting.
- Approximately 90-95% of acute bronchitis cases in healthy adults are secondary to viral infections. The predominant viruses that are causative include:
- Influenza viruses (Type A and B): Commonly cause seasonal epidemics.
- Parainfluenza viruses: Often cause croup in children but can cause bronchitis in adults.
- Adenoviruses: Can cause a range of respiratory illnesses.
- Respiratory Syncytial Virus (RSV): A common cause of bronchiolitis in infants but can affect adults.
- Rhinoviruses: The most common cause of the common cold.
- Coronaviruses: Including those that cause the common cold and SARS-CoV-2 (COVID-19).
- Bacterial infections are less common primary causes but can occur, often as a secondary infection following a viral illness. Dominant bacterial agents include:
- *Mycoplasma pneumoniae*: Often associated with "walking pneumonia" but can cause bronchitis.
- *Chlamydophila pneumoniae*: Another atypical bacterium causing respiratory infections.
- *Bordetella pertussis* (Whooping Cough): Causes a characteristic paroxysmal cough.
- Less commonly, *Streptococcus pneumoniae* or *Staphylococcus aureus*.
- Smoke Inhalation: From fires, strong chemical fumes, or even very heavy tobacco smoke exposure.
- Polluted Air Inhalation: Exposure to high levels of urban air pollution, smog, or particulate matter.
- Dust: Exposure to occupational dusts (e.g., silica, coal dust) or environmental dust.
- Chemical Fumes: Such as those from cleaning products, industrial chemicals, or solvents.
- Allergens: In individuals with allergic sensitivities, exposure to pollen, pet dander, mold spores, or dust mites can trigger an acute asthmatic bronchitis-like reaction.
Chronic Bronchitis
Chronic bronchitis is primarily caused by long-term exposure to respiratory irritants, leading to persistent inflammation and structural changes in the airways.
- Smog and Air Pollution: Chronic exposure to urban air pollutants, ozone, and particulate matter.
- Industrial Pollutants: Fumes, gases, and dusts encountered in various occupations (e.g., mining, construction, manufacturing). Examples include silica, coal dust, grain dust, cotton dust, and chemical vapors.
- Toxic Chemicals: Repeated exposure to irritant gases such as ammonia, sulfur dioxide, chlorine, or acid fumes.
- Asthma: Chronic inflammation and airway hyperresponsiveness in asthma can contribute to symptoms overlapping with chronic bronchitis.
- Cystic Fibrosis: A genetic disorder leading to thick, sticky mucus production and recurrent infections, causing chronic bronchial inflammation.
- Bronchiectasis: A condition characterized by permanent enlargement of parts of the airways, leading to chronic mucus accumulation and recurrent infections.
- Alpha-1 Antitrypsin Deficiency: A genetic condition that predisposes individuals to early-onset emphysema and chronic bronchitis.
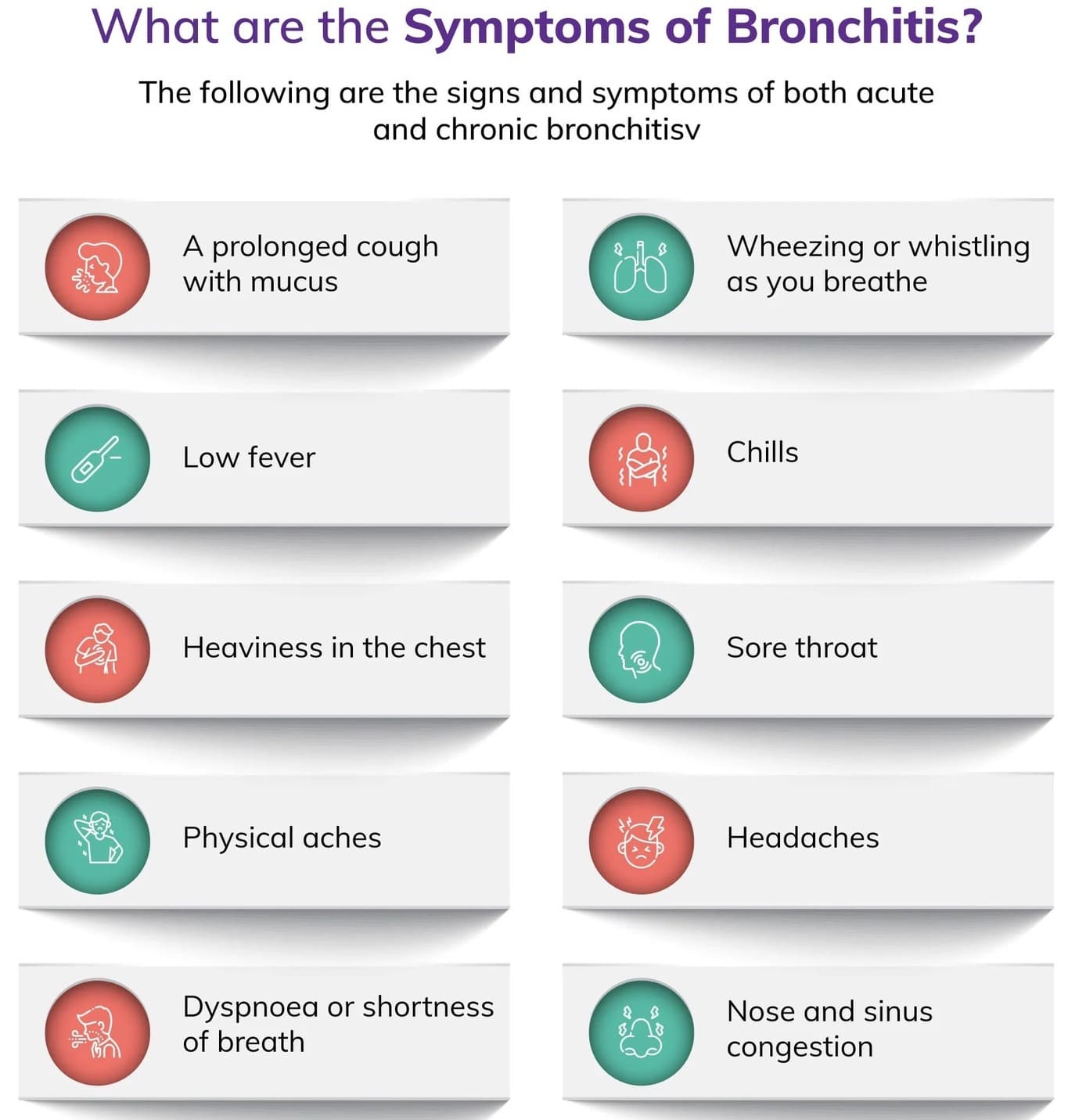
Clinical manifestations of Bronchitis
Acute Bronchitis
Patients with acute bronchitis present with:
- a. Usually, their cough is the predominant complaint and the sputum is clear or yellowish, although sometimes it can be purulent. It's important to note that purulent sputum does not inherently correlate with bacterial infection or necessitate antibiotic use.
- b. The cough after acute bronchitis typically persists for 10 to 20 days but occasionally may last for 4 or more weeks. The median duration of cough after acute bronchitis is 18 days. Paroxysms of cough, especially if accompanied by an inspiratory "whoop" (a high-pitched gasp) or post-tussive emesis (vomiting after coughing), should raise concerns for pertussis (whooping cough).
- c. The cough may be worsened by cold air, smoke, or irritants.
- Runny nose (rhinorrhea)
- Nasal congestion
- Sore throat (pharyngitis)
- Headache
- Muscle aches (myalgia)
Chronic bronchitis
- a. The most common and defining symptom of patients with chronic bronchitis is a persistent cough.
- b. The history of a cough typical of chronic bronchitis is characterized by its presence for most days in a month, lasting for at least 3 months, with at least 2 such consecutive episodes occurring for 2 years in a row.
- c. A productive cough with sputum is present in about 50% of patients. The sputum color may vary from clear, white, yellow, green or at times blood-tinged. The color of sputum may change due to the presence of secondary bacterial infection, but it's important to note that color alone is not a definitive indicator.
- d. Very often, changes in sputum color can be due to peroxidase released by leukocytes in the sputum, giving it a greenish or yellowish hue without a bacterial cause. Therefore, sputum color alone is not a definite indication of bacterial infection and should be interpreted with other clinical signs.
- e. The cough is typically worse in the mornings and in damp or cold weather.
NB: Uncomplicated chronic bronchitis presents primarily with a cough, and there is no evidence of significant airway obstruction physiologically. When airway obstruction is present, it is often indicative of Chronic Obstructive Pulmonary Disease (COPD) with a chronic bronchitis phenotype.
Investigations
- History taking: The diagnosis of bronchitis is primarily made through a detailed history taking, focusing on the onset, duration, and characteristics of symptoms (especially cough), any recent respiratory tract infections, recent or chronic exposure to inhaled irritants (e.g., smoking, occupational hazards, environmental pollutants), and patient's chief complaints.
- Physical examination: This involves a thorough assessment of vital signs, respiratory rate, and oxygen saturation. Key findings during physical examination include:
- Auscultation of lung sounds: May reveal wheezing, rhonchi (coarse rattling sounds), or crackles, indicating inflammation, mucus, or narrowed airways.
- Observation of breathing patterns: Assessment for signs of respiratory distress, such as accessory muscle use, pursed-lip breathing, or tachypnea.
- Palpation of chest: May reveal tenderness due to muscle strain from coughing.
- Inspection: Assessment for cyanosis or clubbing of fingers (in chronic cases).
- Chest X-ray (CXR):
- For acute bronchitis, a chest X-ray is typically normal and is primarily performed to rule out pneumonia or other lung pathologies, especially if symptoms are severe, atypical, or persistent, or if there is a concern for consolidation.
- For chronic bronchitis, a CXR may show increased bronchovascular markings, cardiomegaly (if cor pulmonale is present), or evidence of hyperinflation in advanced cases of COPD. It helps exclude other causes of chronic cough.
- Fiberoptic bronchoscopy: May be both diagnostic (allowing for direct visualization of the airways, collection of qualitative cultures, and biopsy of suspicious lesions) and therapeutic (e.g., for mucus plug removal or re-expansion of lung segments). This is usually reserved for complex or atypical cases, or to rule out other conditions.
- Arterial Blood Gases (ABGs) / Pulse Oximetry:
- Pulse oximetry provides a non-invasive measurement of oxygen saturation (SpO2). Abnormalities may be present, depending on the extent of lung involvement and underlying lung disease.
- ABGs provide a more detailed assessment of oxygenation (PaO2), ventilation (PaCO2), and acid-base balance. In chronic bronchitis, chronic hypoxemia and hypercapnia may be present, especially during exacerbations.
- Gram stain/cultures:
- Sputum collection: Can be done for Gram stain and culture to identify bacterial pathogens and determine antibiotic sensitivity, especially if bacterial infection is suspected (e.g., purulent sputum with fever and worsening symptoms).
- Other samples: Needle aspiration of empyema, pleural fluid, transtracheal or transthoracic fluids, lung biopsies, and blood cultures may be done to recover causative organisms in severe cases or when pneumonia is suspected. More than one type of organism may be present; common bacteria include *Streptococcus pneumoniae*, *Staphylococcus aureus*, alpha-hemolytic streptococcus, *Haemophilus influenzae*; also viral pathogens like Cytomegalovirus (CMV). Note: Sputum cultures may not identify all offending organisms, and blood cultures may show transient bacteremia.
- Complete Blood Count (CBC):
- Leukocytosis (elevated white blood cell count) is usually present in bacterial infections, although a low white blood cell (WBC) count may be present in viral infection, immunosuppressed conditions such as AIDS, and overwhelming bacterial pneumonia.
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are non-specific inflammatory markers that may be elevated.
- Serologic studies: E.g., viral titers (for influenza, adenovirus, RSV), *Legionella* titers, or cold agglutinins (for *Mycoplasma pneumoniae*). These assist in the differential diagnosis of specific organisms, especially in atypical presentations or outbreaks.
- Pulmonary Function Studies (PFTs):
- These tests measure lung volumes, capacities, and airflow. In acute bronchitis, PFTs are typically normal or show mild, transient obstruction.
- In chronic bronchitis, especially when progressing to COPD, volumes may be decreased (due to congestion and alveolar collapse), airway pressure may be increased, and compliance decreased. Obstructive patterns with reduced FEV1/FVC ratio are characteristic. Shunting may be present, leading to hypoxemia.
- Electrolytes: Sodium and chloride levels may be low, particularly in cases of severe illness or syndrome of inappropriate antidiuretic hormone secretion (SIADH) which can sometimes complicate severe respiratory infections.
- Alpha-1 Antitrypsin Deficiency Screening: Recommended in patients with early-onset emphysema or a family history of lung disease, as it is an inherited risk factor for COPD.
Management
Medical Management
Acute Bronchitis
Acute bronchitis is predominantly self-limiting, and treatment is typically symptomatic and supportive, focusing on relieving discomfort and promoting recovery.
- For cough relief, both non-pharmacological and pharmacological therapy should be offered:
- a. Non-pharmacological therapy includes:
- Drinking plenty of fluids (warm water, herbal tea, clear broths) to thin secretions and keep the throat moist.
- Consuming soothing agents like honey (not for infants under 1 year due to botulism risk), ginger, or using throat lozenges or hard candies to relieve throat irritation.
- Using a cool-mist humidifier in the bedroom to moisten the air and help loosen mucus.
- Avoiding irritants such as cigarette smoke (including secondhand smoke), air pollution, and chemical fumes.
- b. Pharmacological antitussive agents:
- Dextromethorphan: An over-the-counter cough suppressant.
- Codeine: A narcotic cough suppressant, sometimes prescribed for severe cough, but its use is generally discouraged due to its addictive potential and side effects.
- Guaifenesin: An expectorant that helps to thin mucus, making it easier to cough up. Often found in combination with antitussives.
- It's important to use these agents judiciously as suppressing a productive cough excessively can hinder clearance of secretions.
- a. Non-pharmacological therapy includes:
- For treatment of wheezing or bronchospasm: Inhaled bronchodilators (e.g., short-acting beta-agonists like albuterol) may be prescribed to reduce bronchospasm, open airways, and promote sputum expectoration, especially if the patient has underlying reactive airway disease or significant wheezing.
- Analgesic and antipyretic agents: Over-the-counter medications like acetaminophen (paracetamol) or ibuprofen can be used to treat associated malaise, myalgia (muscle aches), headache, and fever.
- Corticosteroids: Oral corticosteroids (e.g., prednisone) or inhaled corticosteroids may be considered in cases with significant inflammation or bronchospasm that is unresponsive to bronchodilators, to help with the inflammation. However, their routine use in acute bronchitis is not recommended.
- Lifestyle modification: Smoking cessation is paramount for preventing chronic bronchitis and recurrent acute episodes. The avoidance of allergens and environmental pollutants (e.g., industrial dust, chemicals) also plays an important role in the avoidance of recurrence and complications.
- Vaccinations:
- Influenza vaccine: Especially recommended annually for special groups including adults older than 65, children younger than two years (older than six months), pregnant women, and residents of nursing homes and long-term care facilities.
- Pneumococcal vaccine: Recommended for individuals at higher risk of developing complications (e.g., pneumonia), including people with chronic lung diseases (asthma, COPD), immunocompromised adults, and adults older than 65.
- Antibiotics: A course of oral antibiotics (e.g., a macrolide, doxycycline, or trimethoprim-sulfamethoxazole) may be instituted in specific situations, but their routine use for acute bronchitis is highly controversial and generally not recommended because most cases are viral. Antibiotics are considered only if:
- Bacterial infection is strongly suspected (e.g., high fever, severe purulent sputum, signs of pneumonia on X-ray, or prolonged symptoms).
- The patient is immunocompromised.
- There's a concern for pertussis (treated with macrolides).
Chronic bronchitis
The primary aim of treatment for chronic bronchitis is to relieve symptoms, prevent complications (such as exacerbations and progression to COPD), and slow the progression of the disease. The primary goals of therapy are aimed at reducing the overproduction of mucus, controlling inflammation, managing cough, and improving airflow.
Pharmacological interventions are the following:
- Bronchodilators: These are cornerstone medications for symptomatic relief by opening the airways.
- Short-acting β-Adrenergic receptor Agonists (SABAs) like albuterol (salbutamol): Used as rescue inhalers for quick relief of acute shortness of breath or wheezing.
- Long-acting β-Adrenergic receptor Agonists (LABAs) like salmeterol, formoterol: Used for maintenance therapy to provide sustained bronchodilation.
- Anticholinergic agents (Short-acting: ipratropium; Long-acting: tiotropium, aclidinium): Help by blocking acetylcholine, which leads to bronchodilation, increasing the airway lumen, and reducing mucus production. They also aid in increasing ciliary function and by increasing mucous hydration. Often used in combination with beta-agonists.
- Glucocorticoids: These powerful anti-inflammatory medications reduce inflammation and mucus production.
- Inhaled corticosteroids (ICS) like fluticasone, budesonide: Often used in combination with LABAs (e.g., in COPD exacerbations) to reduce exacerbations and improve quality of life. However, their long-term use can induce systemic side effects (e.g., osteoporosis, diabetes, hypertension, increased risk of pneumonia) and should be administered under medical supervision and for the shortest effective periods.
- Oral corticosteroids: Used for acute exacerbations of chronic bronchitis to reduce severe inflammation, but not for long-term daily use due to significant side effects.
- Antibiotic therapy: Generally not indicated in the stable treatment of chronic bronchitis, as it is a chronic inflammatory condition, not an infection. However:
- Acute exacerbations of chronic bronchitis (AECB) with signs of bacterial infection (e.g., increased sputum purulence, volume, or dyspnea) often warrant antibiotic treatment.
- Long-term macrolide therapy (e.g., azithromycin) has been shown to have anti-inflammatory and immunomodulatory properties and can reduce the frequency of exacerbations in some patients with severe COPD and chronic bronchitis, hence it may have a role in the treatment of chronic bronchitis, but this is typically reserved for severe cases and involves careful risk-benefit assessment.
- Phosphodiesterase-4 (PDE4) inhibitors: Roflumilast is an example of this class. These oral medications decrease inflammation and promote airway smooth muscle relaxation by preventing the hydrolysis of cyclic adenosine monophosphate (cAMP), a substance whose degradation leads to the release of inflammatory mediators. They are used in severe COPD associated with chronic bronchitis and a history of exacerbations.
- Mucolytics: Medications like N-acetylcysteine or carbocysteine may be used to thin mucus, making it easier to clear, though their benefit is often modest.
- Oxygen therapy: For patients with chronic hypoxemia, supplemental oxygen therapy can improve survival and quality of life.
Non Pharmacological Measures
- The most critical non-pharmacological intervention is smoking cessation. Smoking cessation significantly improves mucociliary function, decreases goblet cell hyperplasia (which contributes to mucus overproduction), and has been shown to reduce airway injury resulting in lower levels of exfoliated mucus in tracheobronchial cells. It is the single most effective intervention to slow disease progression.
- Pulmonary rehabilitation: An important and comprehensive part of treatment for chronic bronchitis and COPD, which consists of:
- Education: On disease management, medications, self-care, and warning signs of exacerbations.
- Lifestyle modification: Including nutrition, stress management, and avoidance of triggers.
- Regular physical activity: Tailored exercise programs to improve exercise tolerance, muscle strength, and reduce dyspnea.
- Breathing techniques: Such as pursed-lip breathing and diaphragmatic breathing to optimize lung function.
- Avoidance of exposure to known pollutants: Either at work or in the living environment (e.g., air pollution, secondhand smoke, occupational dusts).
- Nutritional support: Patients with chronic bronchitis/COPD may experience weight loss or malnutrition due to increased energy expenditure for breathing or difficulty eating, so nutritional counseling is important.
- Psychological support: Addressing anxiety and depression, which are common in chronic respiratory conditions.
Nursing management
Nursing management for bronchitis involves a holistic approach, focusing on assessment, symptom management, patient education, and prevention of complications. While some interventions refer to general principles, specific applications for bronchitis are highlighted below.
- a. Refer to the notes of general assessment nursing interventions, but specifically for bronchitis:
- Respiratory Assessment: Auscultate lung fields for adventitious sounds (wheezing, rhonchi, crackles), assess respiratory rate, depth, and effort. Note presence of dyspnea, use of accessory muscles, pursed-lip breathing. Monitor oxygen saturation via pulse oximetry.
- Cough Assessment: Characterize the cough (productive/non-productive, frequency, severity, timing). Assess sputum characteristics (color, consistency, amount, odor). Inquire about any triggers for the cough.
- Vital Signs: Monitor temperature for fever, pulse for tachycardia, and blood pressure.
- Pain Assessment: Evaluate for chest pain or abdominal muscle pain related to coughing, using a pain scale.
- Hydration Status: Assess skin turgor, mucous membranes, and urine output to determine hydration levels.
- Activity Tolerance: Assess the patient's ability to perform activities of daily living (ADLs) and any limitations due to dyspnea or fatigue.
- History: Detailed history of smoking, exposure to irritants, vaccination status, and any underlying lung conditions (e.g., asthma, COPD).
- a. Refer to the notes of general fever nursing interventions, but specifically for bronchitis:
- Administer antipyretics (e.g., acetaminophen, ibuprofen) as prescribed.
- Provide comfort measures: cool compresses, light clothing, and ensuring a comfortable room temperature.
- Encourage increased oral fluid intake to prevent dehydration associated with fever.
- Monitor temperature regularly and assess for signs of worsening infection.
- a. Refer to the nursing interventions of influenza under infection prevention, but specifically for bronchitis:
- Educate on good hand hygiene practices for both the patient and caregivers.
- Advise avoiding close contact with individuals who are sick.
- Encourage annual influenza vaccination and pneumococcal vaccination as recommended, especially for at-risk groups.
- Instruct on proper disposal of tissues and respiratory etiquette (coughing/sneezing into elbow).
- For chronic bronchitis, reinforce adherence to prescribed medications to prevent exacerbations, which can be triggered by infections.
- a. Position head midline with flexion appropriate for age/condition to gain or maintain an open airway. For adults, semi-Fowler's or high-Fowler's position is generally preferred to maximize lung expansion.
- b. Elevate the head of the bed (HOB) to decrease pressure on the diaphragm, promote lung expansion, and facilitate drainage of secretions.
- c. Observe signs of worsening infection or increased secretions to identify an infectious process or exacerbation.
- d. Auscultate breath sounds and assess air movement frequently to ascertain status and note progress or deterioration. Document changes.
- e. Instruct the patient to increase fluid intake (2-3 liters/day unless contraindicated by co-morbidities like heart failure or renal disease) to help liquefy secretions, making them easier to expectorate.
- f. Demonstrate and encourage effective coughing and deep-breathing techniques (e.g., huff cough, diaphragmatic breathing) to maximize effort and facilitate clearance of secretions. Assist with chest physiotherapy (postural drainage, percussion, vibration) if indicated and prescribed.
- g. Keep the patient's back dry and linen clean to prevent skin breakdown and further complications, especially if there is excessive sweating or sputum production.
- h. Turn the patient every 2 hours (for bedridden patients) to prevent pooling of secretions, promote lung expansion, and prevent possible aspirations.
- i. Administer bronchodilators (e.g., nebulizers, metered-dose inhalers) as prescribed, monitoring for effectiveness and side effects (e.g., tachycardia, tremors).
- j. Encourage ambulation and mobilization as tolerated to promote lung expansion and secretion clearance.
- a. Place patient in semi-Fowler's or high-Fowler's position to allow for maximum lung expansion and ease of breathing.
- b. Increase fluid intake as applicable and tolerated to liquefy secretions and improve mucociliary clearance.
- c. Keep patient's back dry and provide frequent linen changes to maintain comfort and prevent skin issues.
- d. Place a pillow when the client is sleeping to provide adequate lung expansion while sleeping, possibly by elevating the head slightly.
- e. Instruct how to splint the chest wall with a pillow or hands for comfort during coughing and to reduce pain. Elevate the head over the body as appropriate to promote physiological ease of maximal inspiration.
- f. Maintain a patent airway; suctioning of secretions may be done as ordered to remove secretions that obstruct the airway, especially in patients with impaired cough reflex or thick secretions.
- g. Provide respiratory support: Oxygen inhalation is provided per doctor’s order to aid in relieving patient from dyspnea and to maintain adequate oxygen saturation levels (e.g., SpO2 >90%). Monitor oxygen flow rate and effectiveness.
- h. Administer prescribed cough suppressants and analgesics. Be cautious, however, because opioids may depress respirations more than desired. Use judiciously to promote patient comfort without compromising respiratory drive.
- i. Educate on pursed-lip breathing and diaphragmatic breathing techniques to improve ventilation and reduce air trapping.
- j. Provide periods of rest between activities to conserve energy and reduce dyspnea.
- k. Monitor for signs of respiratory distress and immediately report any worsening symptoms to the physician.
- Educate patients about their condition, medication regimen (purpose, dose, side effects, proper inhaler technique), and when to seek medical attention (e.g., worsening cough, increased sputum, fever, increased dyspnea).
- Counsel on smoking cessation strategies and provide resources.
- Discuss avoidance of environmental triggers and irritants.
- Teach energy conservation techniques for chronic bronchitis patients.
- Encourage regular exercise within tolerance limits.
Nursing Diagnoses
Nursing diagnoses provide a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. For bronchitis, common nursing diagnoses, based on NANDA International (NANDA-I) classifications, might include:
- Ineffective Airway Clearance related to increased mucus production, thick tenacious secretions, impaired ciliary function, and/or bronchospasm, as evidenced by abnormal breath sounds (e.g., rhonchi, wheezes), ineffective cough, dyspnea, and/or changes in respiratory rate/rhythm.
- Impaired Gas Exchange related to altered oxygen supply (e.g., narrowed airways, mucus plugging) and/or ventilation-perfusion imbalance, as evidenced by dyspnea, abnormal arterial blood gases (e.g., decreased PaO2, increased PaCO2), cyanosis, and/or abnormal breath sounds. (More prevalent in chronic bronchitis/COPD exacerbations).
- Ineffective Breathing Pattern related to inflammatory process, mucus obstruction, anxiety, and/or pain (e.g., from coughing), as evidenced by dyspnea, tachypnea, use of accessory muscles, pursed-lip breathing, and/or altered chest excursion.
- Acute Pain related to persistent coughing, muscle strain (e.g., intercostal, abdominal), and/or chest discomfort secondary to inflammation, as evidenced by patient reports of pain, grimacing, guarding behavior, and/or restlessness.
- Fatigue related to increased work of breathing, persistent coughing, sleep disturbance, and/or systemic infection, as evidenced by patient reports of overwhelming lack of energy, lethargy, decreased activity level, and/or difficulty performing ADLs.
- Activity Intolerance related to imbalance between oxygen supply and demand, dyspnea, and/or fatigue, as evidenced by verbal reports of fatigue/weakness, exertional dyspnea, abnormal heart rate or blood pressure response to activity, and/or decreased ability to perform ADLs. (More common in chronic bronchitis).
- Deficient Knowledge regarding disease process, treatment regimen, symptom management, and/or prevention of recurrence/exacerbations, as evidenced by patient questions, inaccurate follow-through of instructions, and/or development of preventable complications.
- Risk for Infection related to stasis of secretions, impaired ciliary action, and/or compromised immune response. (Applies to both acute bronchitis progressing to pneumonia or chronic bronchitis with increased susceptibility to exacerbations).
- Excessive Anxiety related to dyspnea, fear of suffocation, change in health status, and/or uncertainty about the future, as evidenced by patient reports of nervousness, restlessness, increased respiratory rate, and/or apprehension.
Complications of Bronchitis
While acute bronchitis is usually self-limiting and resolves without complications, chronic bronchitis can lead to significant and often debilitating complications. Complications can also arise from acute bronchitis, especially in vulnerable populations (e.g., very young, elderly, immunocompromised).
Complications of Acute Bronchitis
- Pneumonia: The most common and serious complication. The inflammation and impaired mucociliary clearance can allow bacterial or viral infections to spread from the bronchi to the lung parenchyma, leading to pneumonia. This risk is higher in individuals with weakened immune systems, underlying lung disease, or the very young/elderly.
- Acute Exacerbation of Underlying Chronic Lung Disease: In individuals with pre-existing conditions like asthma or COPD, acute bronchitis can trigger a severe exacerbation of their underlying disease, leading to worsening symptoms, increased airway obstruction, and potentially respiratory failure.
- Persistent Cough: While most coughs resolve within 2-3 weeks, post-infectious cough can linger for several weeks (e.g., 4-8 weeks) due to airway hypersensitivity, even after the infection has cleared. This is often bothersome but not usually serious.
- Bronchiolitis: More common in infants and young children, severe inflammation can extend to the smaller airways (bronchioles), causing significant respiratory distress.
- Dehydration: Especially in infants and elderly, fever and increased respiratory rate can lead to fluid loss if fluid intake is not maintained.
- Ear Infections (Otitis Media) and Sinusitis: Upper respiratory tract infections that lead to bronchitis can also predispose to complications in adjacent structures.
Complications of Chronic Bronchitis
Chronic bronchitis, particularly as part of COPD, can lead to a range of severe and progressive complications affecting various body systems.
- Recurrent Acute Exacerbations of Chronic Bronchitis (AECB): These are acute events characterized by a worsening of respiratory symptoms (increased dyspnea, cough, sputum volume, and/or purulence) beyond day-to-day variations. AECBs are often triggered by bacterial or viral infections, air pollution, or other irritants and can lead to significant morbidity, hospitalizations, and accelerate lung function decline.
- Chronic Obstructive Pulmonary Disease (COPD): Chronic bronchitis is a major component and a clinical diagnosis of COPD. Over time, the persistent inflammation and airway remodeling lead to irreversible airflow limitation, reduced lung function, and progressive dyspnea.
- Emphysema: Often coexists with chronic bronchitis in COPD. Emphysema involves the destruction of the alveolar walls, leading to enlarged air spaces and loss of elastic recoil, further contributing to airflow obstruction and impaired gas exchange.
- Respiratory Failure: As the disease progresses, the lungs become unable to adequately oxygenate the blood and/or remove carbon dioxide, leading to chronic hypoxemia (low oxygen) and hypercapnia (high CO2). This can necessitate supplemental oxygen therapy and, in severe exacerbations, mechanical ventilation.
- Cor Pulmonale (Right-Sided Heart Failure): Chronic hypoxemia leads to pulmonary vasoconstriction, increasing pulmonary artery pressure (pulmonary hypertension). This increased workload on the right ventricle of the heart can eventually lead to its enlargement and failure, resulting in peripheral edema (swelling in the ankles, legs), jugular venous distension, and hepatomegaly.
- Pulmonary Hypertension: Persistently elevated blood pressure in the arteries of the lungs, often a precursor to cor pulmonale.
- Pneumothorax: In severe cases of COPD with emphysema, ruptured bullae (enlarged air sacs) can lead to a collapsed lung.
- Polycythemia: Chronic hypoxemia can stimulate the kidneys to produce erythropoietin, leading to an increase in red blood cell production. This thickens the blood, increasing the risk of blood clots.
- Weight Loss and Malnutrition: Increased energy expenditure for breathing, reduced appetite (due to dyspnea, fatigue, or depression), and systemic inflammation can lead to unintended weight loss and malnutrition.
- Osteoporosis: Chronic inflammation, corticosteroid use, and reduced physical activity in COPD/chronic bronchitis patients contribute to bone density loss and increased fracture risk.
- Muscle Wasting and Dysfunction: Systemic inflammation, hypoxemia, and reduced activity can lead to skeletal muscle weakness and atrophy, further impacting exercise tolerance and quality of life.
- Depression and Anxiety: The chronic nature of the disease, debilitating symptoms, and impact on quality of life often lead to significant psychological distress.
- Increased Susceptibility to Infections: Impaired mucociliary clearance and chronic inflammation make individuals with chronic bronchitis more vulnerable to recurrent respiratory infections.
- Respiratory Acidosis: In advanced stages or during exacerbations, the body's inability to effectively clear CO2 can lead to a build-up of acid in the blood.
LARYNGITIS
LARYNGITIS
Introduction
Laryngitis refers to inflammation of the larynx, commonly known as the voice box. The larynx contains the vocal cords, which vibrate to produce sound. When the vocal cords become inflamed or irritated, they swell, leading to a distorted voice or a complete loss of voice. It can present in both acute and chronic forms.
Types of Laryngitis
Laryngitis can be classified according to its duration:
- Acute Laryngitis: This is a common, often mild, and self-limiting condition that typically lasts for a period of 3 to 7 days, rarely exceeding two weeks. It usually has a sudden onset.
- Chronic Laryngitis: If laryngitis lasts for over 3 weeks, it is termed chronic laryngitis. This form of laryngitis is usually less severe but can be persistent and may indicate an underlying, ongoing irritant or medical condition.
Classification of Laryngitis according to cause
- Infectious Laryngitis: The cause is a pathogen, most commonly viruses, but sometimes bacteria or fungi.
- Non-infectious Laryngitis: Caused by non-pathogens such as vocal overuse, irritants (smoke, allergens), or conditions like gastroesophageal reflux disease (GERD).
Pathophysiology
The pathophysiology of laryngitis involves the inflammatory response of the laryngeal tissues, particularly the vocal cords.
- Acute laryngitis is characterized by inflammation and congestion of the larynx in the early stages. This inflammation can encompass the supra-glottic (above the vocal cords), glottic (vocal cords themselves), or subglottic (below the vocal cords) larynx, or any combination thereof, depending on the inciting agent.
- The inflammation leads to increased vascular permeability and fluid accumulation (edema) in the vocal cord tissues.
- As the inflammatory process progresses, white blood cells and other immune components arrive at the site of infection or irritation to remove pathogens or clear debris.
- This process enhances vocal cord edema, which adversely affects the normal vibration of the vocal folds, changing the amplitude, magnitude, and frequency of their dynamic movement.
- As the edema progresses, the phonation threshold pressure (the minimum subglottal pressure required to initiate vocal fold vibration) can increase. This means it becomes more difficult to generate adequate vocal fold vibration and produce clear sound.
- The patient develops phonatory changes (dysphonia or hoarseness) both as a result of the changing fluid-wave dynamics of the inflamed and edematous tissue, and as a result of both conscious and unconscious adaptation to attempt to mitigate these altered tissue dynamics (e.g., trying to push more air through).
- Sometimes edema is so marked that it becomes impossible to generate adequate phonation pressure, leading to frank aphonia (complete loss of voice). Such maladaptations (e.g., vocal strain) may result in prolonged vocal symptoms after an episode of acute laryngitis that can persist long after the inciting event has resolved.
- Acute laryngitis typically resolves within 2 weeks. Persistent symptoms beyond this timeframe may indicate a super-infection or a transition to chronic laryngitis, suggesting ongoing irritation or an underlying pathology.
Causes of Laryngitis
Acute Laryngitis
Infectious causes
- Viral agents: The most common cause of acute laryngitis. Viruses such as rhinovirus (common cold), parainfluenza virus, respiratory syncytial virus (RSV), coronavirus, adenovirus, and influenza virus are all potential etiologic agents (listed in roughly descending order of frequency). It is possible for bacterial super-infection to occur in the setting of viral laryngitis, which classically occurs approximately seven days after symptoms begin, leading to worsening symptoms.
- Bacterial organisms: Less common as primary causes but can be involved in superinfections. Common bacterial culprits include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Certain exanthematous febrile illnesses such as measles, chickenpox, and pertussis (whooping cough) are also associated with acute laryngitis symptoms, so it is prudent to obtain an accurate immunization history.
- Fungal infection: Laryngitis caused by fungal infections like Candida albicans is very rare in immunocompetent individuals. It is more often seen as chronic laryngitis in immunocompromised patients (e.g., those with HIV/AIDS, cancer patients undergoing chemotherapy) or in patients using inhaled steroid medications (e.g., for asthma or COPD) without proper rinsing of the mouth after use.
Non-infectious causes
Acute non-infectious laryngitis can be due to:
- Vocal trauma/abuse/misuse: Such as excessive shouting, singing, or prolonged talking.
- Allergies: Inhalation of allergens can cause inflammation of the laryngeal mucosa.
- Gastro-esophageal reflux disease (GERD) or Laryngopharyngeal Reflux (LPR): Stomach acid irritating the larynx.
- Asthma: Can sometimes cause irritation or inflammation in the larynx.
- Environmental irritants: Exposure to pollutants, chemical fumes, or dry air.
- Smoking: Direct irritation from tobacco smoke.
- Inhalational injuries: Such as inhaling smoke from fires.
- Functional/conversion disorders: Psychogenic causes where no organic pathology is found.
Chronic Laryngitis
A variety of factors can cause chronic laryngitis, often involving prolonged irritation or damage to the vocal cords:
- Long-term cigarette smoking: A major cause, as smoke directly irritates the vocal cords and can lead to swelling and changes in the laryngeal lining.
- Gastroesophageal reflux (GERD) or Laryngopharyngeal Reflux (LPR): Stomach acid moving up into the esophagus and irritating the larynx over time, often without typical heartburn symptoms.
- Excessive alcohol consumption: Can irritate the vocal cords.
- Chronic exposure to environmental irritants: Such as chemical fumes, dust, or allergens.
- Vocal abuse or overuse: Chronic strain on the voice due to professional use (singers, teachers) or habitual shouting.
- Chronic sinusitis or bronchitis: Postnasal drip can continuously irritate the larynx.
- Vocal cord lesions: Such as polyps, nodules (singer's nodes), cysts, or granulomas that form on the vocal cords due to chronic irritation or overuse.
- Neurological conditions: Affecting vocal cord movement (e.g., vocal cord paralysis).
- Allergies: Persistent allergic reactions.
- Pneumonia: Can sometimes be associated with persistent cough and laryngeal irritation.
- Thyroid dysfunction: Hypothyroidism can sometimes affect vocal cord function.
- Rare causes: Autoimmune diseases (e.g., rheumatoid arthritis affecting laryngeal joints), granulomatous diseases (e.g., sarcoidosis), or even early laryngeal cancer.
Clinical manifestations
Acute Laryngitis
In addition to symptoms of an upper respiratory tract infection (i.e., fever, cough, rhinitis), the patient primarily experiences dysphonia or a hoarse voice. The individual may also experience the following:
- Hoarseness of the voice: The hallmark symptom, ranging from mild to severe.
- Weakened voice or loss of voice (aphonia): Due to the vocal cords being too swollen to vibrate effectively.
- Rough or raspy voice quality.
- Constant tickling sensation or minor throat irritation.
- Dry cough: Often irritating and persistent.
- Odynophonia: Pain when speaking.
- Dysphagia: Difficulty swallowing.
- Odynophagia: Painful swallowing (less common than in pharyngitis).
- Dyspnea: Shortness of breath, especially if there is significant laryngeal swelling (more common in children with croup).
- Rhinorrhea: Runny nose (if associated with a common cold).
- Postnasal discharge: Mucus dripping down the back of the throat.
- Sore throat: May accompany other URI symptoms.
- Congestion: Nasal or chest congestion.
- Fatigue and malaise: General feeling of being unwell.
- Fever: Usually low-grade, if present.
Chronic Laryngitis
Symptoms are usually less acute but persistent:
- Persistent hoarseness: The primary and most common symptom, lasting for weeks or months.
- Loss of voice: May occur intermittently or be constant in severe cases.
- A raw or irritated throat sensation.
- A persistent dry cough.
- Frequent throat clearing.
- Feeling of a lump in the throat (globus sensation).
- Reduced vocal range or fatigue when speaking.
- Difficulty swallowing: Less common, but can occur if there's significant inflammation or associated conditions like GERD.
- Swelling of the lymph nodes in your neck: Not common in isolated chronic laryngitis, but may indicate an underlying infection or more serious condition.
- Fever: Generally absent in non-infectious chronic laryngitis.
Test and Diagnosis
Acute Laryngitis
Diagnosis is primarily clinical, based on patient history and physical examination.
- History: Presence of typical symptoms like hoarseness, often following an upper respiratory infection, and duration of symptoms usually less than 3 weeks.
- Physical examination: Examination of the throat may reveal redness or inflammation. Direct visualization of the larynx is usually not necessary for uncomplicated acute laryngitis.
- Laryngoscopy: Direct visualization of the larynx using a laryngoscope is generally reserved for cases of persistent symptoms, severe symptoms, or if there is concern for a more serious underlying condition. This allows the clinician to see inflamed and edematous vocal cords, sometimes with mucus or slight redness.
Chronic Laryngitis
Diagnosis requires a more thorough investigation to identify the underlying cause, as the symptoms persist for more than 3 weeks.
- History: Detailed history of chronic hoarseness, vocal habits, exposure to irritants (smoking, chemicals), symptoms of GERD, allergies, and any associated systemic conditions.
- Laryngoscopy: This is a crucial diagnostic tool for chronic laryngitis. It allows direct visualization of the vocal cords and surrounding structures. Findings may include:
- Redness and swelling of vocal cords.
- Presence of vocal cord nodules, polyps, cysts, granulomas.
- Changes suggestive of chronic reflux (e.g., posterior laryngeal erythema).
- Signs of Reinke's edema (swelling of the vocal cords due to smoking).
- Suspicious lesions that may indicate malignancy.
- Imaging studies:
- CT scan or MRI of the neck and throat: May be performed to rule out tumors, anatomical abnormalities, or spread of disease, especially if malignancy is suspected or if a mass is palpated.
- Laboratory tests:
- High throat swab for culture and sensitivity: If bacterial or fungal infection is suspected and visualized, a swab can be taken for culture to identify the pathogen and determine appropriate antibiotic/antifungal treatment.
- Full blood count (CBC): Can indicate signs of infection or other systemic issues.
- Allergy testing: If allergies are suspected as a contributing factor.
- pH monitoring: Esophageal pH monitoring (24-hour pH impedance study) can be done to confirm GERD or LPR, especially if symptoms are atypical or unresponsive to treatment.
- Biopsy: If any suspicious lesions are found during laryngoscopy, a biopsy may be taken for histopathological examination to rule out malignancy.
Management
Medical Management
Treatment is often supportive in nature and depends on the severity and underlying cause of laryngitis. The primary goals are to reduce inflammation, alleviate symptoms, and identify/address the root cause.
- Voice rest: This is the single most important factor for acute laryngitis. Use of the voice during laryngitis results in incomplete or delayed recovery and can worsen vocal cord damage. Complete voice rest is recommended, although it is almost impossible to achieve. If the patient needs to speak, they should be instructed to use a "confidential voice" – a normal phonatory voice at low volume without whispering or projecting, as whispering can strain the vocal cords more than soft speaking.
- Humidification: Inhaling humidified air (e.g., from a cool-mist humidifier, steam inhalation from a bowl of hot water, or a steamy shower) enhances moisture of the upper airway and vocal cords, which helps to soothe irritation, reduce swelling, and facilitate the removal of secretions and exudates.
- Avoidance of irritants: Smoking and alcohol should be strictly avoided as they significantly irritate the laryngeal mucosa and delay prompt resolution of the disease process. Exposure to environmental pollutants, dust, and allergens should also be minimized.
- Dietary modification: Dietary restrictions are recommended for patients with gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR). This includes avoiding caffeinated drinks, spicy food items, fatty food, chocolate, peppermint, citrus fruits, and carbonated beverages. Another important lifestyle modification is the avoidance of late meals; the patient should have meals at least 3 hours before sleeping to prevent nocturnal reflux. The patient should drink plenty of water to maintain hydration. While the efficacy of these dietary measures is well-established for classic GERD, their effectiveness in LPR is debated, but they are often still employed.
- Medications:
- Antibiotics: Antibiotic prescription for an otherwise healthy patient with acute viral laryngitis is currently unsupported and ineffective. However, for high-risk patients (e.g., immunocompromised) or patients with severe symptoms and confirmed bacterial infection (e.g., with signs of bacterial superinfection), antibiotics may be given. Some authors recommend narrow-spectrum antibiotics only in the presence of identifiable gram stain and culture.
- Antivirals: Rarely used for laryngitis unless a specific viral cause (e.g., severe influenza or herpes simplex) is identified and treatment is indicated.
- Antifungals: Fungal laryngitis can be treated with the use of oral antifungal agents such as fluconazole. Treatment is usually required for a three-week period and may be repeated if needed. This should be reserved for patients with confirmed fungal infection via laryngeal examination and/or culture.
- Mucolytics: Like guaifenesin, may be used for clearing thick secretions.
- Corticosteroids: May be prescribed in severe cases of acute laryngitis with significant vocal cord swelling causing severe hoarseness or mild airway compromise (e.g., croup in children) to rapidly reduce inflammation. Long-term use is generally avoided due to side effects.
- Anti-reflux medications: In addition to lifestyle and dietary modifications, LPR-related laryngitis is treated with anti-reflux medications. Medications that suppress acid production, such as H2 receptor blockers (e.g., ranitidine, famotidine) and proton pump inhibitors (PPIs) (e.g., omeprazole, lansoprazole, esomeprazole), are effective against gastroesophageal reflux. PPIs are generally found to be most effective for LPR. These may require higher doses or a twice-daily dosing schedule to be effective in this setting, and treatment often needs to be long-term.
- Analgesics/Antipyretics: Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage associated pain and fever.
- Voice Therapy: For chronic laryngitis, particularly that related to vocal abuse/misuse or vocal cord lesions, referral to a speech-language pathologist for voice therapy is crucial. Therapy teaches proper vocal hygiene, efficient voice production techniques, and strategies to prevent further vocal cord injury.
- Surgical Intervention: For chronic laryngitis caused by vocal cord polyps, nodules, cysts, or other lesions that do not resolve with conservative management, surgical removal may be necessary.
Nursing Interventions/Management
1. Assessment of the Patient
- a. Obtain a comprehensive history including the onset, duration, and nature of hoarseness or voice changes. Inquire about associated symptoms like cough, sore throat, difficulty swallowing, fever, and symptoms of upper respiratory infection or reflux.
- b. Assess for potential causes: recent illness, vocal overuse/abuse (e.g., shouting, singing), exposure to irritants (smoking, chemicals), allergies, and history of GERD.
- c. Perform vital sign assessment (Temperature, Pulse, Respiration, Blood Pressure) and a general physical examination. Note any signs of respiratory distress, stridor, or changes in voice quality.
- d. Document the patient's vocal habits, profession (if voice-demanding), and lifestyle (smoking, alcohol use).
- e. Inquire about any past medical history, current medications, and allergies.
2. Promoting Voice Rest and Vocal Hygiene
- a. Educate the patient on the critical importance of absolute voice rest during acute laryngitis. Explain that talking, whispering, and throat clearing can further irritate and damage vocal cords.
- b. Instruct the patient to use non-vocal communication methods (e.g., writing, gestures) as much as possible.
- c. Teach "confidential voice" if speaking is unavoidable: speak softly but not whisper, use natural pitch.
- d. Emphasize avoidance of vocal strain, shouting, screaming, and prolonged singing.
3. Managing Symptoms and Promoting Comfort
- a. Encourage increased fluid intake to keep vocal cords hydrated and thin secretions. Warm fluids (e.g., herbal tea with honey) or cool liquids may be soothing.
- b. Advise the use of a cool-mist humidifier in the patient's room, especially at night, to humidify the air and soothe the larynx.
- c. Instruct on proper steam inhalation techniques (e.g., leaning over a bowl of hot water with a towel over the head for 5-10 minutes, several times a day), ensuring safety to prevent burns.
- d. Administer prescribed analgesics (e.g., acetaminophen, ibuprofen) for pain relief and antipyretics for fever.
- e. Encourage throat lozenges or sprays to relieve irritation and dryness, if appropriate.
- f. Instruct on gargling with warm salt water to reduce throat discomfort.
- g. Advise avoiding irritants such as tobacco smoke (including secondhand smoke), alcohol, and caffeine, which can dry out and irritate the vocal cords.
4. Preventing and Managing Complications
- a. Monitor for signs of respiratory distress (e.g., increased respiratory rate, shortness of breath, stridor, retractions, cyanosis), especially in children, as laryngeal swelling can compromise the airway. Report immediately to the physician.
- b. For chronic laryngitis, educate the patient about the potential long-term effects of persistent inflammation (e.g., vocal cord nodules, polyps, or changes that could mask malignancy).
- c. Ensure the patient completes the full course of antibiotics if prescribed for bacterial laryngitis to prevent recurrence or resistance.
- d. For patients with GERD/LPR, reinforce adherence to dietary and lifestyle modifications (e.g., elevating the head of the bed, avoiding late meals, dietary triggers) and consistent use of anti-reflux medications.
5. Health Education and Patient Teaching
- a. Educate the patient and family about the causes, symptoms, and treatment of laryngitis, distinguishing between acute and chronic forms.
- b. Provide detailed instructions on proper vocal hygiene, including the importance of hydration, avoiding shouting/whispering, and resting the voice.
- c. Teach patients about identifying and avoiding personal triggers for laryngitis (e.g., allergens, irritants, vocal abuse).
- d. For patients with chronic laryngitis due to GERD, provide comprehensive education on anti-reflux measures.
- e. Emphasize the importance of follow-up care, especially if symptoms persist or worsen, or if there is concern for chronic conditions or malignancy.
- f. Advise seeking medical attention immediately for severe symptoms such as difficulty breathing, severe pain, or inability to swallow.
6. Referral and Collaboration
- a. Collaborate with the healthcare team, including physicians, speech-language pathologists (for voice therapy in chronic cases), and allergists or gastroenterologists if underlying conditions like allergies or GERD are present.
- b. Facilitate referrals to specialists as needed (e.g., otolaryngologist for laryngoscopy in chronic or atypical cases).
Complications
While acute laryngitis is usually benign and self-limiting, complications can arise, especially if the underlying cause is not addressed or in specific populations. Chronic laryngitis, due to persistent irritation, can lead to more significant issues.
- Airway Obstruction (especially in children): In infants and young children, significant swelling of the subglottic area (below the vocal cords) can lead to a condition called croup (laryngotracheobronchitis). This causes a characteristic "barking" cough, stridor (a high-pitched crowing sound during inhalation), and difficulty breathing, which can be life-threatening and require immediate medical attention. In adults, severe laryngeal edema can also rarely lead to airway compromise.
- Vocal Cord Lesions: Chronic inflammation, vocal abuse, or irritation can lead to the development of benign lesions on the vocal cords:
- Vocal Nodules (Singer's Nodes): Callus-like growths that result from chronic vocal cord abuse, leading to persistent hoarseness.
- Vocal Polyps: Softer, blister-like growths, often unilateral, that can result from a single traumatic vocal event or chronic irritation.
- Vocal Cysts: Fluid-filled sacs within the vocal cord.
- Granulomas: Inflammatory lesions, often associated with intubation trauma or LPR.
- Reinke's Edema: A severe swelling of the vocal cords, almost exclusively seen in heavy smokers, leading to a deep, husky voice.
- Chronic Hoarseness/Dysphonia: Persistent voice changes that significantly impact communication and quality of life, leading to vocal fatigue, pain, or professional limitations.
- Psychological Impact: Chronic voice problems can lead to frustration, social isolation, anxiety, or depression, especially in individuals whose profession relies on their voice.
- Misdiagnosis of Serious Conditions: Persistent hoarseness, especially in smokers or heavy drinkers, can be a symptom of laryngeal cancer. Untreated chronic laryngitis can delay the diagnosis of malignancy, which is a critical concern.
- Spread of Infection: If infectious laryngitis is not properly managed, especially bacterial cases, the infection can spread to other parts of the respiratory tract, leading to bronchitis, pneumonia, or other more systemic infections.
- Laryngeal Stenosis: In rare cases, chronic inflammation or repeated trauma can lead to scarring and narrowing of the larynx (stenosis), which can severely restrict airflow and may require surgical intervention.
It is crucial for persistent hoarseness (lasting more than 2-3 weeks), especially in adults, to be evaluated by an otolaryngologist (ENT specialist) to rule out serious underlying conditions, including malignancy.
Nursing management
1. Assessment of the patient
- a. Carrying out history of the presenting signs and symptoms e.g. fever, fatigue, throat pain and hoarseness of the voice among others.
- b. Taking vital observation e.g. TPR/BP and general examination to exclude other diseases
- c. Alerting the doctor who will order for investigations and admission, there the nurse will assist the patient throughout the process.
2. Managing fever (patient has 37.6 and above temperature, chills)
- a. Assess the patient’s vital signs at least every 4 hours.
- b. Remove excessive clothing, blankets, and linens. Adjust the room temperature.
- c. Administer and monitor the prescribed antibiotics and anti-pyretics.
- d. Assess the mental status of the patient because elevated temperatures can alter the function of the mind.
- e. Offer a tepid sponge bath.
- f. Elevate the head of the bed
3. To alleviate pain
- a. Assess the patient’s vital signs and characteristics of pain at least 30 minutes after administration of medication.
- b. Elevate the head of the bed and position the patient in semi Fowler’s.
- c. Administer prescribed analgesics
4. Ensuring clear airway
- a. Assess the patient’s vital signs and characteristics of respirations at least every 4 hours. Assess for signs of hypoxia.
- b. Place the patient on a side-lying or prone position.
- c. Suction secretions.
- d. Administer the prescribed medications (e.g. corticosteroids) and antibiotic medications.
5. To prevent infection
- a. Assess vital signs and observe for any signs of infection as well as for any signs of respiratory distress.
- b. Perform a focused assessment on the oropharyngeal region, particularly checking for any collection of abscess.
- c. Teach the patient how to perform proper hand hygiene.
- d. Administer antibiotics as prescribed.
6. Educate the patient about self-management
- a. Use a humidifier or inhale steam to alleviate dryness.
- b. Get vocal therapy to analyze and correct the way you use your voice and any abnormal speech patterns that place stress on your vocal cords and voice box.
- c. Drink lots of fluids.
- d. Gargle with 1/2 tsp. of salt and 1/2 tsp. of baking soda in 8 oz. of warm water.
- e. Rest your voice.
- f. Avoid screaming or talking loudly for long periods of time.
- g. Avoid decongestants, which can dry your throat.
- h. Suck on lozenges to keep your throat lubricated.
- i. Refrain from whispering, which can strain the voice.
Complications
- Epiglositis
- Pneumonia
- Chronic irritation of throat
- Throat cancer
- Chronic hoarseness of the voice
PHARYNGITIS
PHARYNGITIS
Introduction
Pharyngitis is the inflammation of the mucous membranes of the pharynx. In most cases, the cause is an infection, either bacterial or viral. Other less common causes of pharyngitis include allergies, trauma, cancer, reflux, and certain toxins.
Types of Pharyngitis
Pharyngitis can be classified according to the duration i.e. as acute or chronic.
- Acute pharyngitis: has a sudden onset, and it resolves within less than 3 months. It may settle completely and recur in the future.
- Chronic pharyngitis: can last up to more than 3 months or having more than 5 episodes of tonsillitis in a year.
Classification of pharyngitis according to cause
- Infectious Pharyngitis: the cause is a pathogen e.g., commonly viruses, bacteria.
- Non-infectious pharyngitis: Caused by non-pathogens e.g., GERD.
Pathophysiology
Bacteria and viruses can cause direct invasion of the pharyngeal mucosa. Certain viruses like rhinovirus can cause irritation secondary to nasal secretions. In almost all cases, there is a local invasion of the pharyngeal mucosa which also results in excess secretion and edema. The inflammatory response leads to the characteristic symptoms of sore throat, redness, and swelling.
Causes of pharyngitis
- Viral causes: About 50% to 80% of pharyngitis, or sore throat, symptoms are viral in origin and include a variety of viral pathogens. These pathogens are predominantly rhinovirus, influenza, adenovirus, coronavirus, and parainfluenza. Less common viral pathogens include herpes simplex virus (HSV), Epstein-Barr virus (EBV) which causes infectious mononucleosis, human immunodeficiency virus (HIV), and coxsackievirus (causing Hand, Foot, and Mouth Disease). More severe cases tend to be bacterial and may develop after an initial viral infection.
- Bacterial causes: The most common bacterial infection is Group A beta-hemolytic streptococci (GAS), which causes 5% to 36% of cases of acute pharyngitis, particularly in children. Other bacterial etiologies include Group C and G streptococci, Chlamydia pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, Candida albicans (fungal infection, often in immunocompromised individuals), Neisseria meningitidis, Neisseria gonorrhoeae (gonococcal pharyngitis), Arcanobacterium haemolyticum, Fusobacterium necrophorum (associated with Lemierre's syndrome), and Corynebacterium diphtheriae (diphtheria, rare due to vaccination).
- Non-infectious causes: Environmental allergies and chemical exposures (e.g., smoke, pollutants, dry air), gastroesophageal reflux disease (GERD) where stomach acid irritates the throat, excessive voice use, and mouth breathing can also cause acute or chronic pharyngitis.
- Pharyngitis symptoms may also be part of the symptom complexes of other serious illnesses, including peritonsillar abscess, retropharyngeal abscess, epiglottitis (a life-threatening emergency), and Kawasaki disease (in children).
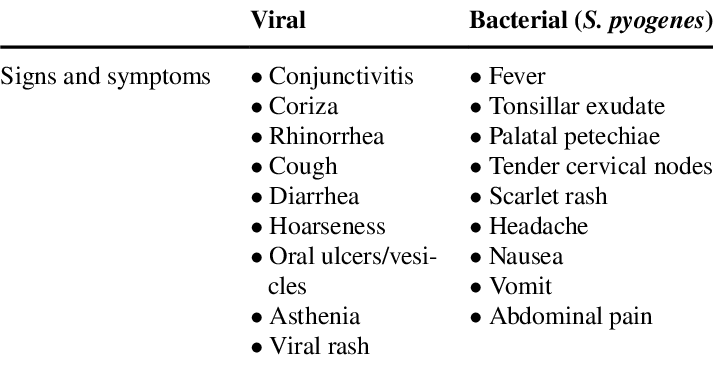
Clinical manifestations
The signs and symptoms of pharyngitis can vary depending on the underlying cause, but common manifestations include:
- Sore throat/Throat pain: Often described as scratchy, burning, or painful, especially when swallowing.
- Dysphagia: Difficulty or pain when swallowing.
- Fever: Common, especially with bacterial or severe viral infections.
- Tonsillar exudates: White patches or streaks of pus on the tonsils (more common in bacterial infections like strep throat).
- Pharyngeal erythema: Redness and inflammation of the throat.
- Fatigue/Malaise: General feeling of being unwell.
- Nasal congestion and rhinorrhea: Runny nose, sneezing (more common in viral pharyngitis).
- Postnasal drip: Mucus dripping down the back of the throat, causing irritation and cough.
- Headache.
- Painful cervical adenopathy: Swollen and tender lymph nodes in the neck.
- Cough: Can be dry or productive.
- Myalgia and arthralgia: Muscle and joint aches (especially with viral infections like influenza).
- Ear pain: Referred pain from the throat.
- Rash: Can occur with certain infections, e.g., scarlatiniform rash with strep throat (scarlet fever), or maculopapular rash with infectious mononucleosis.
NB: Uncomplicated infectious pharyngitis, both viral and bacterial, typically is self-limited to 5 to 7 days, is not progressive, is bilateral, does not have trismus (difficulty opening the mouth), and does not have evidence of airway obstruction (stridor or severe difficulty breathing).
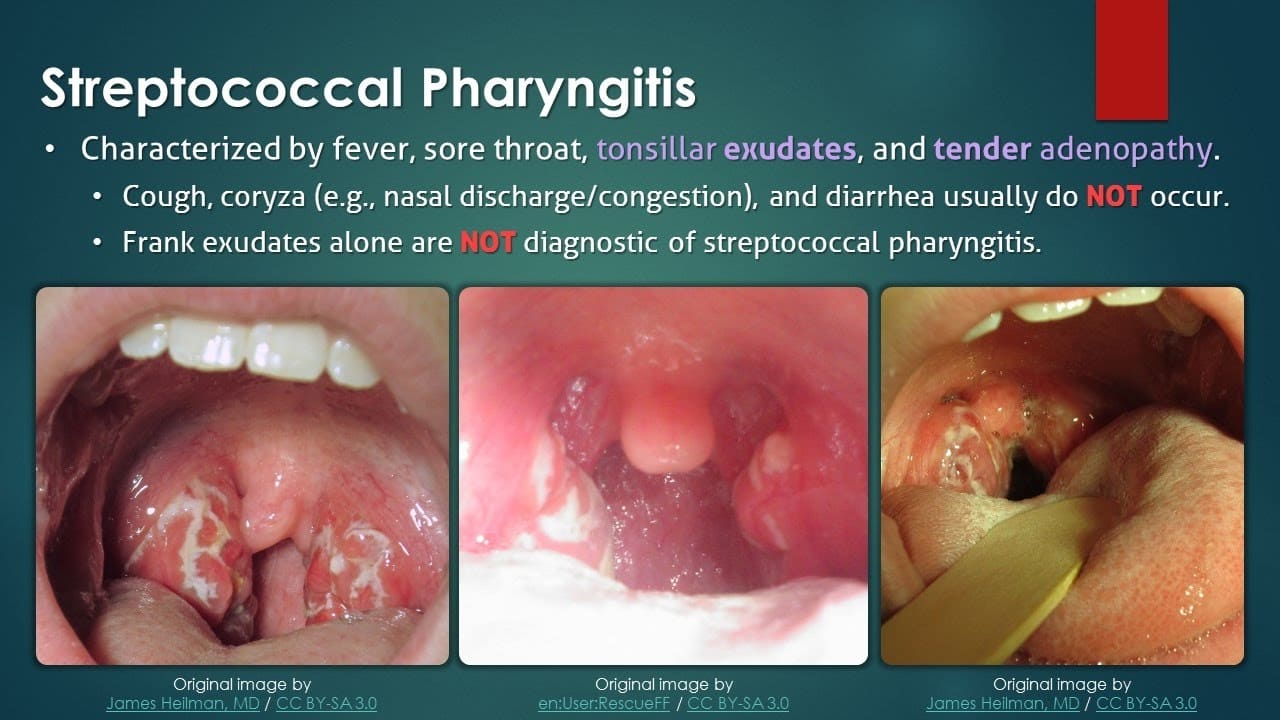
Diagnosis & Differential Diagnosis
Diagnosis
Diagnosis of pharyngitis typically involves a combination of clinical assessment and diagnostic tests.
- Inspection of the throat: Using a light source and tongue depressor to visualize the pharynx and tonsils for redness, swelling, exudates, ulcers, or vesicles.
- Palpation of the neck: To check for swollen and tender lymph nodes (cervical adenopathy).
- Examination of the ears and nose: To check for other possible sites of infection or signs of allergies.
- Skin examination: To check for any rashes (e.g., scarlatiniform rash of scarlet fever).
- Auscultation of lung and heart sounds: To rule out respiratory or cardiac involvement.
- Rapid Antigen Detection Test (RADT): A quick test performed in the clinic to detect Group A Streptococcus (GAS) bacteria. If positive, it suggests strep throat. If negative, a throat culture may still be performed, especially in children, to confirm.
- Throat culture: A sterile swab rubbed over the tonsils and posterior pharynx is sent to the lab to grow and identify bacteria. This is considered the gold standard for diagnosing strep throat.
- Molecular tests (PCR): Highly sensitive and specific tests that detect bacterial or viral DNA/RNA directly from a throat swab, providing rapid and accurate results for various pathogens.
- Complete Blood Count (CBC): May show elevated white blood cell count (leukocytosis) in bacterial infections, or atypical lymphocytes in viral infections like mononucleosis.
- Monospot test (Heterophile Antibody Test): Used to diagnose infectious mononucleosis, especially if EBV is suspected.
- Blood cultures: Rarely needed, but may be considered in severe cases or immunocompromised patients to rule out bloodstream infection.
Differential Diagnosis
It is important to differentiate pharyngitis from other conditions that can present with similar symptoms:
- Common cold: Usually presents with prominent nasal symptoms (runny nose, sneezing) and milder sore throat.
- Influenza: Characterized by abrupt onset of high fever, severe body aches, headache, fatigue, and respiratory symptoms including sore throat.
- Laryngitis: Primarily affects the voice box, leading to hoarseness or loss of voice, with less prominent throat pain.
- Tonsillitis: Often occurs with pharyngitis, but specifically refers to inflammation of the tonsils, which may be swollen, red, and have exudates.
- Allergic rhinitis: Chronic nasal congestion, sneezing, itching, and often clear nasal discharge, but typically without fever or significant throat pain unless due to postnasal drip.
- Gastroesophageal Reflux Disease (GERD): Can cause chronic sore throat, hoarseness, and a sensation of a lump in the throat, especially if untreated.
- Peritonsillar abscess: A collection of pus behind the tonsil, characterized by severe unilateral throat pain, trismus, muffled voice ("hot potato voice"), and deviation of the uvula. This is an emergency.
- Retropharyngeal abscess: A deep neck space infection, presenting with severe sore throat, fever, difficulty swallowing, stiff neck, and sometimes airway compromise. Also an emergency.
- Epiglottitis: Inflammation of the epiglottis, a life-threatening emergency, characterized by rapid onset of severe sore throat, dysphagia, drooling, muffled voice, and inspiratory stridor.
- Oral candidiasis (Thrush): Fungal infection causing white patches on the tongue and oral mucosa, which can extend to the throat, often seen in immunocompromised individuals.
- Sexually transmitted infections (STIs): Gonococcal pharyngitis or primary HIV infection can present with sore throat.
- Kawasaki disease: A rare childhood illness causing inflammation of blood vessels, with symptoms including fever, rash, conjunctivitis, swollen lymph nodes, and red throat.
Management
Treatment goals:
- Relieve symptoms (pain, fever).
- Eradicate infection (if bacterial).
- Prevent complications.
Medical Management
Treatment of pharyngitis is largely supportive for viral cases and focuses on maintaining adequate hydration and caloric intake and controlling pain and fever. For bacterial cases, antibiotics are crucial.
- Hydration: Maintaining adequate oral fluid intake is essential to prevent dehydration, especially with fever and difficulty swallowing. If oral intake is insufficient, intravenous (IV) hydration may be necessary.
- Diet: Soft, easily swallowed foods and cool liquids are often preferred. Avoid irritating foods (acidic, spicy).
- Rest: Adequate rest is important for recovery, especially for children.
- Pharmacologic Management:
- Antibiotics: Prescribed only for bacterial pharyngitis, most commonly for Group A Streptococcus. Penicillin or amoxicillin are first-line agents. For penicillin-allergic patients, azithromycin, cephalexin, or clindamycin may be used. The full course of antibiotics must be completed to prevent complications like rheumatic fever.
- Analgesics and Antipyretics:
- Acetaminophen (paracetamol): For pain and fever relief.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): (e.g., ibuprofen, naproxen) also reduce pain and inflammation.
- Topical Anesthetics: Throat lozenges, sprays (e.g., benzocaine, phenol), or gargles can provide temporary local pain relief.
- Corticosteroids: (e.g., dexamethasone) may be administered in severe cases of pharyngitis (e.g., with significant swelling or in infectious mononucleosis) to reduce inflammation, improve swallowing, and potentially reduce pain.
- Antivirals: Rarely used for viral pharyngitis, except in specific cases like severe influenza (oseltamivir) or herpes simplex virus (acyclovir).
Nursing interventions/management
1. Assessment of the patients
- a. Carrying out a comprehensive history of the presenting signs and symptoms (e.g., fever, ear pain, sore throat, difficulty swallowing, cough, nasal discharge, rash, muscle aches, exposure history).
- b. Taking vital observations (e.g., Temperature, Pulse, Respirations, Blood Pressure) and performing a general physical examination to assess the patient's overall condition and to exclude other serious conditions (e.g., signs of airway compromise, severe dehydration).
- c. Alerting the doctor if signs of severe infection or complications are present, for further investigations and management. The nurse will assist the patient throughout this process.
2. Managing fever
- a. Assess the patient’s vital signs, especially temperature, at least every 4 hours, and more frequently if fever is high.
- b. Remove excessive clothing and blankets. Adjust the room temperature to a comfortable level.
- c. Administer prescribed antipyretics (e.g., acetaminophen, ibuprofen) as ordered.
- d. Offer a tepid sponge bath or cool compresses to the forehead and axillae, if tolerated and effective.
- e. Encourage increased fluid intake to prevent dehydration associated with fever.
- f. Encourage rest.
3. To relieve pain and discomfort
- a. Assess the patient’s pain level using a pain scale and characteristics of pain (location, quality, duration) before and at least 30 minutes after administration of medication to evaluate effectiveness.
- b. Administer prescribed analgesics (e.g., acetaminophen, NSAIDs).
- c. Encourage warm or cool liquids (e.g., warm tea with honey, cold water, popsicles) as preferred by the patient to soothe the throat.
- d. Offer throat lozenges or sprays as ordered or as appropriate.
- e. Encourage gargling with warm salt water several times a day to reduce inflammation and discomfort.
- f. Advise the patient to minimize talking or rest the voice to reduce strain on the throat.
- g. Encourage the patient to verbalize feelings of pain and discomfort.
- h. Elevate the head of the bed or position the patient in semi-Fowler’s to promote comfort and ease breathing.
4. Prevention of complications
- a. Continuously assess the patient’s vital signs and respiratory status (rate, depth, effort, presence of stridor, retractions, oxygen saturation) at least every 4 hours, and more frequently if signs of respiratory distress are noted. Assess for signs of hypoxia (e.g., restlessness, cyanosis).
- b. Monitor for signs of worsening infection or development of complications (e.g., peritonsillar abscess: severe unilateral pain, trismus, muffled voice; rheumatic fever: joint pain, rash, cardiac murmurs; glomerulonephritis: dark urine, swelling).
- c. Ensure completion of the full course of antibiotics for bacterial pharyngitis to prevent complications like acute rheumatic fever and post-streptococcal glomerulonephritis.
- d. Position the patient in a side-lying or prone position if secretions are excessive to prevent aspiration, or elevate the head of the bed.
- e. Suction oral secretions as needed to maintain airway patency.
- f. Advise cessation of smoking or avoiding exposure to secondhand smoke, and minimizing alcohol intake, as these can irritate the throat and impede healing.
- g. Administer prescribed medications (e.g., corticosteroids to reduce swelling, antibiotics for bacterial infections).
5. To prevent infection and to promote good nutrition
- a. Assess vital signs and observe for any signs of worsening infection or secondary infections.
- b. Perform a focused assessment on the oropharyngeal region, particularly checking for any collection of abscess or spreading inflammation.
- c. Teach the patient and family how to perform proper hand hygiene to prevent the spread of infection.
- d. Encourage the patient to take a lot of warm fluids (at least 2-3 liters a day, unless contraindicated) to thin secretions and prevent dehydration.
- e. Encourage the patient to consume soft, easy-to-swallow foods rich in vitamins and nutrients to support the immune system. Avoid foods that may irritate the throat (e.g., very hot, cold, spicy, acidic, crunchy foods).
- f. Administer antibiotics as prescribed and ensure adherence.
6. To relieve the patient’s anxiety and Health educate the patient
- a. Reassure the patient and family, providing clear and honest information about the condition and treatment plan.
- b. Assess the patient’s fears and concerns, and provide emotional support and counselling as needed.
- c. Health educate the patient and family about the disease process, its causes, modes of transmission, and expected course.
- d. Teach the patient and family about proper hand hygiene, cough etiquette, and avoiding close contact with others to prevent the spread of infection.
- e. Explain the importance of completing the full course of antibiotics and the signs of complications that require immediate medical attention.
7. Advice on discharge
- a. Encourage the patient to maintain good hydration by taking plenty of warm fluids.
- b. Emphasize the importance of adhering to prescribed medications, especially completing the full course of antibiotics.
- c. Advise on when to return for follow-up appointments with the healthcare provider.
- d. Educate on lifestyle modifications, such as avoiding irritants (smoking, pollutants), managing underlying conditions like GERD or allergies.
- e. Provide clear instructions on warning signs or symptoms that necessitate seeking immediate medical attention (e.g., difficulty breathing, severe worsening pain, persistent high fever, rash, swelling, inability to swallow).
Complications
If left untreated or inadequately managed, pharyngitis, especially bacterial pharyngitis caused by Group A Streptococcus, can lead to several complications:
- Peritonsillar abscess (Quinsy): A collection of pus behind the tonsil, requiring drainage.
- Retropharyngeal abscess: A deep neck space infection behind the pharynx, a life-threatening emergency.
- Epiglottitis: Inflammation of the epiglottis, which can rapidly lead to airway obstruction.
- Cervical lymphadenitis: Inflammation and enlargement of neck lymph nodes.
- Otitis media: Middle ear infection.
- Sinusitis: Inflammation of the sinuses.
- Mastoiditis: Infection of the mastoid bone behind the ear (rare).
- Acute Rheumatic Fever (ARF): A serious inflammatory disease that can affect the heart (rheumatic heart disease), joints, brain, and skin. It is a preventable complication with appropriate antibiotic treatment of strep throat.
- Post-streptococcal Glomerulonephritis (PSGN): A kidney disorder that can develop after a strep infection, characterized by inflammation of the kidney's filtering units.
- Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS): A controversial condition where strep infections are thought to trigger or exacerbate certain neuropsychiatric disorders in children (e.g., OCD, Tourette's syndrome).