Fractures Lecture Notes
A fracture is a medical condition in which there is a break in the continuity of the bone.
This disruption can range from a fine crack to a complete break, involving one or multiple pieces of bone.
Fractures typically occur when the bone is subjected to excessive force or stress that it cannot withstand, often due to trauma (e.g., falls, accidents, sports injuries) or, in some cases, repetitive stress or underlying bone pathology.
Common Childhood Fractures
- Arm bones are fractured more often than other bones.
- Collarbone or shoulder fractures
- Elbow fractures
- forearm, wrist, or hand fracture
- Leg, foot, or ankle fracture.
Causes of Fractures
- Direct Force: in which the fracture occurs at the point of contact.
- Torsion: in which the fracture occurs at the point opposite the location of the force, e.g. twisting of the foot may lead to break of bones of the leg.
- Violent Contractions: e.g. forcibly throwing an object produces powerful muscle contractions which can fracture the humerus. Also in strong contractions in tetanus.
- Disease Processes: cause weakening of the bone structure; osteoporosis, malnutrition, bone tumors

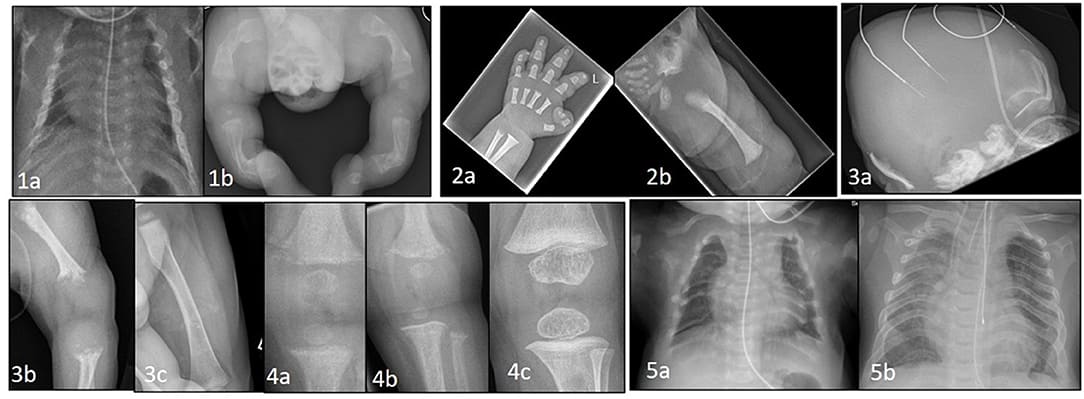
II. Classification of Fractures
Fractures are classified based on several characteristics. Understanding these classifications is crucial for diagnosis and treatment planning.
A. By Communication with the External Environment:
- Closed (Simple) Fracture: The skin overlying the fractured bone is intact. There is no open wound that communicates with the fracture site. Example: A hairline crack in a tibia with no skin break.
- Open (Compound) Fracture: The skin and soft tissues overlying the fracture are disrupted, creating an open wound that connects to the fracture site. The bone may protrude through the skin. Example: A forearm bone breaks and pierces through the skin.
B. By Completeness of the Break:
- Complete Fracture: The bone is broken all the way through, separating it into two or more distinct fragments.
- Incomplete (Partial) Fracture: The bone is not broken all the way through.
- Examples:
- Greenstick Fracture: An incomplete fracture where the bone bends and cracks, but doesn't break completely. Common in children whose bones are more flexible.
- Hairline Fracture: A very fine crack in the bone that may not extend through the entire width of the bone. Often due to repetitive stress.
C. By Displacement (Relationship of Bone Ends):
- Displaced Fracture: The bone fragments are no longer in proper alignment. They have shifted out of their normal anatomical position. Example: The two ends of a broken femur are significantly offset from each other.
- Non-Displaced Fracture: The bone is broken, but the fragments remain in their anatomical alignment. Example: A hairline fracture of a rib where the bone segments are still touching and lined up.
D. By Anatomical Site
- Potts Fracture: Type of fracture that occurs at the ankle joint.
- Colles fracture (distal radius fracture): a fracture that occurs at the wrist joint.
D. By Fracture Pattern (Shape/Direction of the Break):
These describe how the bone breaks:
- Transverse Fracture: The break is in a straight line across the bone, perpendicular to the long axis of the bone.
- Cause: Direct trauma or angulation forces.
- Oblique Fracture: The break occurs at an angle to the long axis of the bone.
- Cause: Angulation and rotational forces.
- Spiral Fracture: The break spirals around the bone, resembling a corkscrew.
- Cause: Twisting force, common in sports injuries. Often associated with abuse in children.
- Comminuted Fracture: The bone is shattered into three or more fragments.
- Cause: High-energy trauma (e.g., car accidents, falls from height).
- Impacted Fracture: One end of the fractured bone is driven into the other end or into another bone.
- Cause: Compression force (e.g., a fall landing on the feet, compressing the tibia into the femur).
- Avulsion Fracture: A fragment of bone is pulled away by a tendon or ligament at its attachment site.
- Cause: Sudden, forceful contraction of a muscle or stretching of a ligament.
- Compression Fracture: The bone is crushed or flattened, typically seen in the vertebrae (e.g., due to osteoporosis or severe trauma).
- Complicated fracture: that which is associated with many structures destroyed such as nerves, blood vessels, joints, muscles

E. By Location (Specific Anatomical Features):
- Diaphyseal Fracture: Occurs in the shaft (diaphysis) of the long bone.
- Metaphyseal Fracture: Occurs in the metaphysis, the wider part of the long bone, adjacent to the growth plate.
- Epiphyseal Fracture: Occurs in the epiphysis, the end of the long bone, often involving the joint surface.
- Intra-articular Fracture: The fracture line extends into the joint surface. These are more challenging and can lead to long-term joint dysfunction.
F. By Cause (Etiology):
- Traumatic Fracture: Caused by a sudden, forceful injury (e.g., fall, sports injury, car accident). This is the most common type.
- Stress Fracture: Caused by repetitive, submaximal stress (e.g., marching, running) that gradually weakens the bone. Often seen in athletes.
- Pathologic Fracture: Occurs in a bone that is already weakened by an underlying disease process (e.g., osteoporosis, bone tumor, osteomyelitis, Paget's disease). The force that caused the fracture would not normally break a healthy bone.
G. Specific Pediatric Fractures:
- Growth Plate (Physeal) Fracture: Involves the epiphyseal plate (growth plate) in children, which is weaker than the surrounding bone or ligaments. Classified by Salter-Harris system (Types I-V). Can affect future bone growth.
Pathophysiology of a Fracture
When a bone fractures, several immediate events occur:
- Trauma and Energy Dissipation: The external force applied to the bone exceeds its tensile or compressive strength, leading to a break in its continuity. The energy of the trauma is absorbed by the bone, causing the fracture.
- Vascular Disruption: Blood vessels within the bone (in the Haversian canals and medullary cavity) and surrounding soft tissues are torn. This leads to bleeding at the fracture site.
- Hematoma Formation: The blood quickly collects at the fracture site, forming a fracture hematoma. This hematoma fills the gap between the broken bone ends and surrounds the fracture. It typically clots within hours of the injury.
- Tissue Necrosis and Inflammation: Cells at the fracture edges that lose their blood supply die (avascular necrosis). This tissue damage, combined with the blood extravasation, triggers an acute inflammatory response. Inflammatory mediators are released, attracting phagocytic cells (e.g., neutrophils, macrophages) to the site to clear debris and dead tissue. This initial inflammatory phase is crucial for initiating the healing cascade.
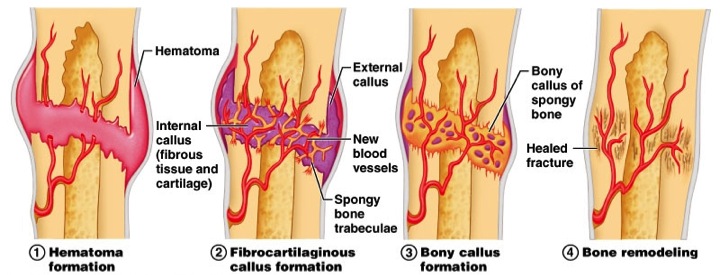
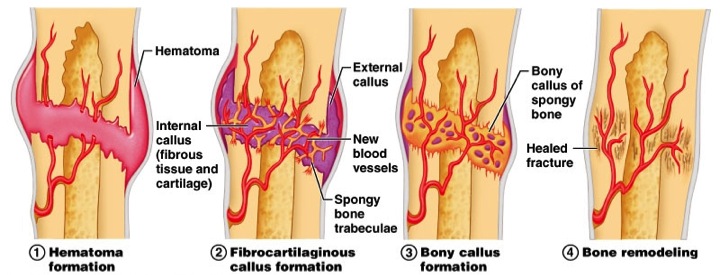
Stages of Bone Healing
Bone healing generally proceeds through four overlapping but distinct stages:
Stage 1: Hematoma Formation (Inflammatory Phase)
Timeframe: Immediately after injury, lasting up to several days.
Key Events:
- After tissue destruction, torn blood vessels result to hematoma formation (which is a collection of clotted blood between the ends of the bones and in surrounding soft tissues. Fibrin, red blood cells, debris and inflammatory exudates come together and form a fibrin clot.
- Inflammatory cells (neutrophils, macrophages) infiltrate the area to remove necrotic tissue and debris.
- Growth factors (e.g., platelet-derived growth factor, transforming growth factor-beta) and cytokines are released from platelets and inflammatory cells, initiating the healing process.
- Fibroblasts, mesenchymal stem cells, and osteoprogenitor cells migrate to the area.
Stage 2: Fibrocartilaginous Callus Formation (Reparative Phase - Soft Callus)
Timeframe: Days 3-14 after injury, lasting several weeks.
Key Events:
- The fracture hematoma is gradually replaced by a soft callus.
- Angiogenesis: New blood vessels begin to grow into the hematoma, restoring blood supply.
- Fibroblasts: Produce collagen fibers, forming a soft fibrous tissue network.
- Chondroblasts: Differentiate from mesenchymal stem cells and produce hyaline cartilage, forming a soft cartilaginous matrix around the fracture ends.
- This combination of fibrous tissue and cartilage creates the "soft callus," which provides initial mechanical stability to the fracture, although it is not yet strong enough to bear weight. The ends of the bone become "sticky" but are still flexible.
Stage 3: Bony Callus Formation (Reparative Phase - Hard Callus)
Timeframe: Weeks 3-4 after injury, lasting 3-4 months.
Key Events:
- The soft callus is gradually converted into a hard, bony callus.
- Osteoblasts: Migrate into the area and begin to deposit woven bone (immature, disorganized bone) within the cartilaginous matrix.
- Endochondral Ossification: In areas of cartilage, the cartilage calcifies and is then replaced by woven bone, similar to how long bones develop.
- Intramembranous Ossification: In areas where oxygen supply is sufficient and there is less movement, osteoblasts directly lay down woven bone.
- The bony callus bridges the fracture gap, providing increasing mechanical stability. Clinically, this is when the fracture becomes "united" and often can be seen on X-ray. The bone ends are firmly joined, but the callus is often larger and unorganized compared to the original bone.
Stage 4: Bone Remodeling
Timeframe: Months to years (can last for many years).
Key Events:
- The woven bone of the hard callus is gradually replaced by stronger, more organized lamellar bone.
- Osteoclasts: Resorb excess bone tissue from the outer surface of the callus and the medullary cavity, reducing the size of the callus.
- Osteoblasts: Continuously lay down new lamellar bone along the lines of mechanical stress.
- The bone reshapes itself according to Wolff's Law (bone remodels in response to mechanical stress), eventually restoring its original cortical and medullary architecture, strength, and shape.
- This stage can continue long after clinical healing is complete, often for several years, perfecting the bone's structure.
Factors Influencing Bone Healing:
Several factors can positively or negatively affect the rate and quality of bone healing:
Positive Factors:
- Adequate Blood Supply: Essential for delivering nutrients, oxygen, and cells.
- Good Immobilization/Stability: Appropriate alignment and limited movement at the fracture site.
- Adequate Nutrition: Calcium, Vitamin D, protein, Vitamin C, etc.
- Age: Younger individuals generally heal faster.
- Overall Health: Healthy individuals with no underlying conditions.
- Growth Factors: Locally and systemically available.
Negative Factors:
- Inadequate Blood Supply: Can lead to avascular necrosis or nonunion.
- Excessive Motion/Instability: Disrupts callus formation.
- Infection: Impedes healing and can lead to osteomyelitis.
- Malnutrition: Deficiency in essential nutrients.
- Systemic Diseases: Diabetes, osteoporosis, chronic kidney disease.
- Medications: Corticosteroids, NSAIDs (especially early in healing).
- Smoking: Nicotine impairs blood flow and osteoblast activity.
- Extensive Soft Tissue Damage: Reduces blood supply and delays healing.
- Large Fracture Gap/Bone Loss: More difficult for callus to bridge.
(a). Systemic factors
- -Age ( healing is almost twice as fast in children as in adults )
- -Activity level.( immobilization)
- -Nutritional status.
- -Hormonal factors (GH, corticosteroids )
- -Diseases e.g. DM, anaemia, neuropathies
- -Vitamin deficiencies e.g. A C D K
- -Drugs e.g. anti coagulants, anti inflammatory.
(b). Local factors.
- -type of bone( cancellous heals faster than cortical bone)
- -type of fracture. Spiral is better than transverse.
- -blood supply ( poor circulation-poor healing.)
- -reduction- faster when there’s perfect reduction.
- -infection
- -soft tissue interposition
- -mobilization. Early vs late mobilization.
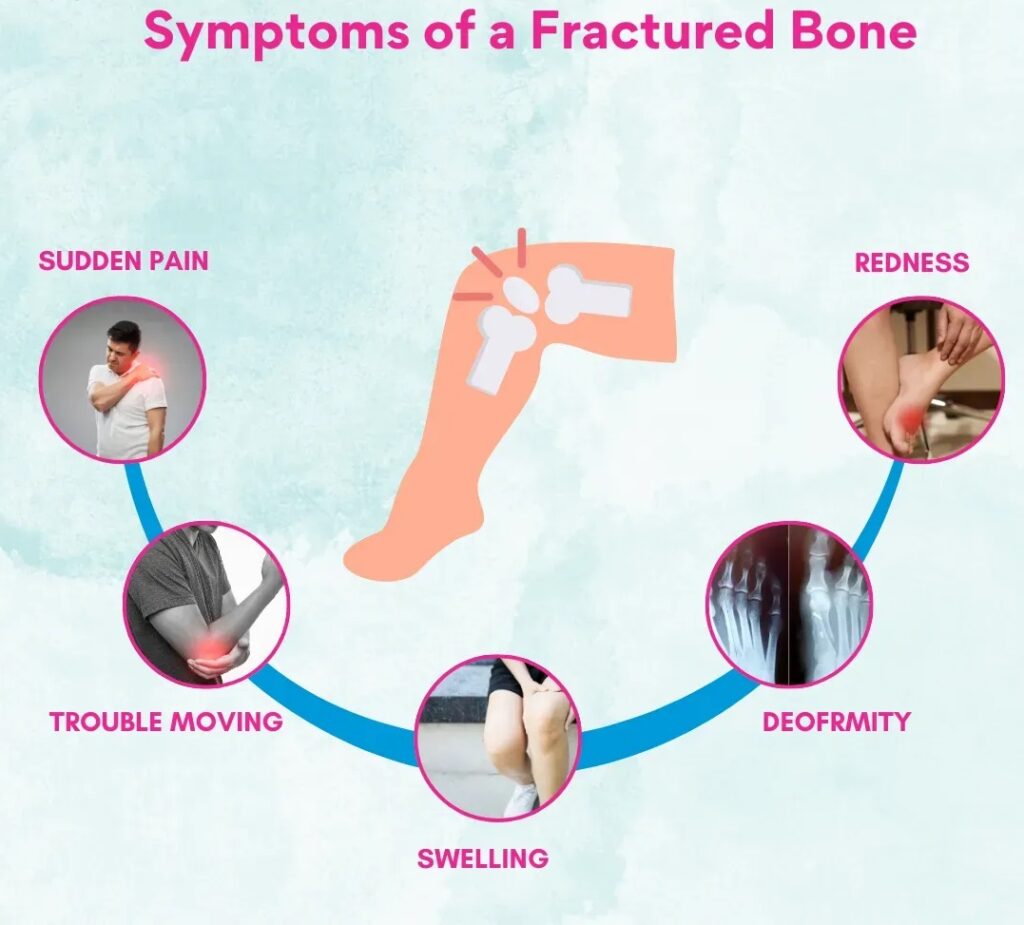
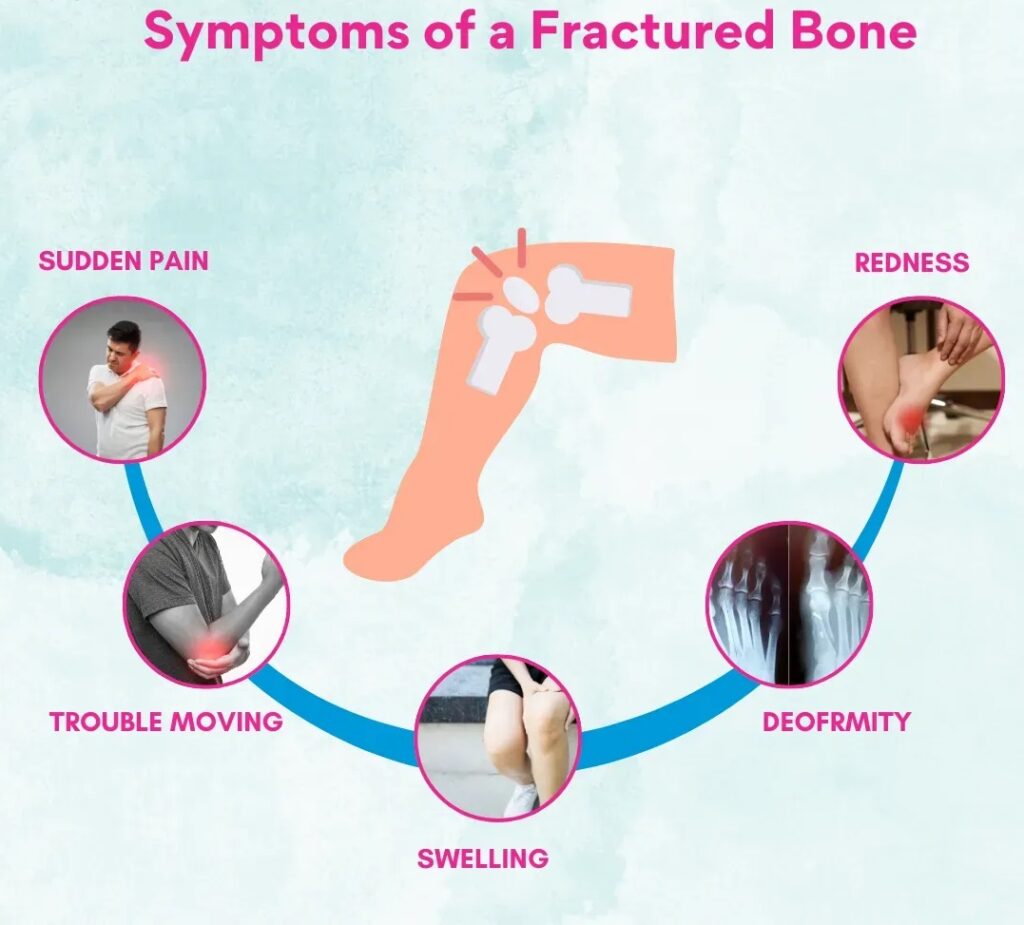
Clinical Manifestations of Fractures (Signs and Symptoms)
The signs and symptoms of a fracture can vary depending on the location, type, and severity of the injury.
- Pain: Which can be acute/chronic, worsening with movement or pressure on the injured area.
- Tenderness: Localized pain upon palpation over the fracture site.
- Swelling (Edema): Accumulation of fluid and blood in the soft tissues surrounding the fracture due to inflammation and hemorrhage. Can develop rapidly and obscure underlying deformities.
- Deformity: An abnormal position, shape, or alignment of the limb or body part. This can include angulation, rotation, shortening, or displacement.
- Loss of Function/Inability to Bear Weight: The patient is usually unable to move the injured part or bear weight due to pain, instability, and disruption of bone integrity.
- Crepitus: A grating or crackling sound or sensation when the bone fragments rub against each other. This should not be deliberately elicited as it can cause further damage and pain.
- Ecchymosis (Bruising): Discoloration of the skin due to extravasated blood into the soft tissues. May appear hours to days after the injury and can spread distally.
- Muscle Spasm: Muscles surrounding the fracture site may involuntarily contract in an attempt to splint the injured part, contributing to pain and deformity.
- Numbness or Tingling (Paresthesia): May indicate nerve damage or compression, especially in the presence of severe swelling or compartment syndrome.
- Open Wound (for Open Fractures): Visible break in the skin, with potential protrusion of bone fragments. This is a critical finding due to the high risk of infection.
- Shock: In cases of severe trauma, especially with large bone fractures (e.g., femur, pelvis), significant blood loss can lead to hypovolemic shock. Signs include pallor, clammy skin, rapid pulse, and hypotension.
Diagnostic Methods for Fractures
Confirming a fracture requires a combination of clinical assessment and imaging studies.
A. Patient History:
Gathering information about the mechanism of injury (how it happened), the forces involved, and the onset and nature of symptoms is crucial. This helps determine the potential type of fracture and associated injuries.
B. Physical Examination:
Inspection: Observe for swelling, deformity, ecchymosis, and open wounds.
Palpation: Gently palpate for localized tenderness and crepitus (without attempting to elicit it). Assess for warmth or coolness of the skin.
Neurovascular Assessment: This is critical and must be performed promptly and repeatedly.
- Circulation: Check pulses distal to the injury, capillary refill, skin color, and temperature.
- Sensation: Assess for numbness, tingling, or decreased sensation in the affected limb.
- Movement: Ask the patient to gently move fingers or toes distal to the injury (if possible without causing further pain or injury).
Comparison: Compare the injured limb to the uninjured limb for symmetry and baseline assessment.
C. Imaging Studies (Radiological Assessment):
X-rays (Radiographs): X-rays are the most common and initial imaging modality for suspected fractures. Its the primary diagnostic tool.
- What they show: They visualize bone structures and can identify the presence, location, type, and alignment of most fractures.
- Views: At least two views (anteroposterior (AP) and lateral) are taken at 90-degree angles to each other to accurately depict the fracture configuration and displacement. Sometimes oblique views are also necessary.
- Limitations: May not detect hairline, stress, or some occult fractures immediately. Soft tissue injuries are not well visualized.
Computed Tomography (CT) Scan: Useful for complex fractures, especially those involving joints (intra-articular fractures), spine, pelvis, or when X-rays are inconclusive.
- What it shows: Provides detailed 3D images of bone, allowing for better visualization of fracture fragments, displacement, and articular surface involvement.
- Limitations: Higher radiation exposure than X-rays.
Magnetic Resonance Imaging (MRI): Excellent for visualizing soft tissues (ligaments, tendons, cartilage, muscles, nerves) and bone marrow. It is particularly useful for detecting occult fractures (not visible on X-ray), stress fractures, bone bruises, and assessing associated soft tissue injuries.
- What it shows: Detailed images of bone marrow edema, soft tissue tears, and subtle fractures.
- Limitations: More expensive and time-consuming, not always readily available for acute trauma.
Bone Scan (Nuclear Medicine Scan):
- When used: Can detect increased metabolic activity in bone, making it sensitive for identifying stress fractures or occult fractures that are not visible on X-ray for several days or weeks.
- What it shows: Areas of increased bone turnover.
- Limitations: Non-specific (doesn't tell you the cause of increased activity), higher radiation.
Ultrasound: Increasingly used in pediatric emergency departments for preliminary assessment of long bone fractures, especially to reduce radiation exposure. Can identify cortical disruption. Also used for soft tissue assessment.
Principles of Fracture Management
(Reduction, Immobilization, Rehabilitation).
The primary goals of fracture management are to:
- Achieve and maintain anatomical alignment (reduction).
- Stabilize the fracture site to allow for bone healing (immobilization).
- Restore optimal function of the injured limb or body part (rehabilitation).
- Prevent complications.
These goals are achieved through a combination of reduction, immobilization, and a structured rehabilitation program.
I. Reduction (Realigning the Bone Fragments):
Reduction is the process of restoring the bone fragments to their anatomical alignment and apposition. This is often the first step in fracture management. This is accomplished by open or closed manipulation of the affected area, referred to as open reduction and closed reduction.
A. Types of Reduction:
- Closed Reduction: Closed reduction is accomplished by bringing the bone ends into alignment by manipulation and manual traction. X-rays are taken to determine the position of the bones. A cast is normally applied to immobilize the extremity and maintain the reduction.
- Definition: Manipulation of the bone fragments without surgical incision to bring them into alignment.
- Method: Performed manually by external manipulation. The fracture site is not surgically exposed.
- When used: Preferred method for most stable fractures, non-displaced or minimally displaced fractures, and when soft tissue damage is minimal.
- Anesthesia: Often requires local anesthesia, conscious sedation, or general anesthesia to relax muscles and minimize pain.
- Confirmation: Alignment is typically confirmed with X-rays or fluoroscopy during the procedure.
- Open Reduction: In open reduction, a surgical opening is made, allowing the bones to be reduced manually under direct visualization. Frequently, internal fixation devices will be used to maintain the bone fragments in reduction.
- Definition: Surgical incision is made to expose the fracture site and directly visualize the bone fragments for alignment.
- When used:
- When closed reduction is unsuccessful or impossible (e.g., bone fragments are trapped in soft tissue).
- For intra-articular fractures (to restore joint congruity).
- For open fractures (which require surgical debridement anyway).
- When internal fixation is required (see below).
- For certain unstable fractures or those with significant displacement.
- Procedure: Once reduced, the fracture is usually stabilized with internal fixation devices.
II. Immobilization (Maintaining Alignment to Allow Healing)
After reduction, the fracture fragments must be held stable and in alignment to allow the bone healing process to occur without disruption.
A. Methods of Immobilization:
- Casting/Splinting:
- Casts: Rigid, circumferential dressing (plaster of Paris or fiberglass) that provides strong immobilization. Applied after swelling has subsided.
- Splints: Non-circumferential devices (e.g., plaster, pre-fabricated materials) that provide less rigid support than casts but allow for swelling. Often used initially for acute injuries or unstable fractures.
- Principle: Holds the joint above and below the fracture to prevent movement at the fracture site.
- Nursing Implications: Neurovascular checks are paramount to ensure the cast/splint is not too tight. Cast care education.
- Traction:
- Definition: Application of a pulling force to an injured body part or extremity.
- Purpose: To reduce muscle spasm, reduce, align, and immobilize fractures, and prevent or reduce deformities.
- Types:
- Skin Traction: Short-term use (48-72 hours). Tapes, boots, or splints are applied to the skin and soft tissues, and weights are attached (e.g., Buck's traction, Russell's traction). Weight limits (usually 5-10 lbs) to prevent skin damage.
- Skeletal Traction: Longer-term use. A pin or wire is inserted into the bone, and weights are attached to the pin. Allows for heavier weights (e.g., 5-45 lbs). Higher risk of infection at pin sites.
- Nursing Implications: Meticulous skin care for skin traction, meticulous pin care for skeletal traction, neurovascular checks, proper alignment of weights and pulleys, prevention of complications of immobility.
- Open Reduction Internal Fixation (ORIF):
- Definition: A surgical procedure where the fracture is opened (open reduction) and bone fragments are stabilized with internal fixation devices (implants) permanently placed inside the body.
- Implants: Plates, screws, rods (intramedullary nails), wires.
- Advantages: Allows for earlier mobilization and weight-bearing in some cases, often provides more rigid fixation.
- Disadvantages: Risk of infection, anesthesia risks, implant failure.
- Nursing Implications: Post-operative care, pain management, wound care, early mobilization, neurovascular checks.
- External Fixation:
- Definition: Pins or wires are inserted into the bone fragments through the skin and connected to an external frame or device.
- When used: Often for complex open fractures with extensive soft tissue damage, highly comminuted or unstable fractures, limb lengthening, or when internal fixation is contraindicated (e.g., severe infection).
- Advantages: Allows access to the soft tissues, minimal blood loss compared to ORIF, allows for early patient mobilization.
- Disadvantages: Risk of pin site infection, bulkiness for the patient, patient discomfort.
- Nursing Implications: Meticulous pin site care to prevent infection, neurovascular checks, education on device management.
III. Rehabilitation (Restoring Function)
Rehabilitation is an integral part of fracture management, beginning early in the recovery process and continuing until the patient achieves maximum functional recovery.
- Pain Management: Adequate pain control is essential to allow for participation in therapy and to improve comfort.
- Physical Therapy (PT): To restore strength, range of motion, endurance, and function to the injured limb and surrounding joints.
- Activities:
- Early Mobilization: As soon as safely possible, to prevent stiffness, muscle atrophy, and complications of immobility. This may start with gentle passive or active range-of-motion exercises for non-injured joints.
- Strengthening Exercises: Progressive resistance exercises for muscles.
- Weight-Bearing Progression: Gradual increase in weight-bearing as per physician's orders and healing status.
- Gait Training: If lower extremity fracture.
- Modalities: Heat, cold, electrical stimulation, massage.
- Occupational Therapy (OT): To help patients regain the ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Training in dressing, bathing, eating, writing, cooking, etc., often using adaptive equipment as needed.
- Patient Education: Ongoing education about the healing process, activity restrictions, exercises, warning signs of complications, and return-to-activity guidelines.
First Aid and Emergency Management for Fractures
This objective focuses on the immediate, critical actions taken at the scene of injury and during the initial transport and presentation to a healthcare facility. These actions are vital for stabilizing the patient, preventing further injury, and potentially saving lives.
I. General First Aid Principles (ABCDE)
The foundational principles of emergency first aid, particularly in trauma, follow the ABCDE approach, where "D" becomes highly relevant for fractures:
A - Airway: Ensure the patient's airway is clear and open. Remove any obstructions.
B - Breathing: Check if the patient is breathing effectively. Provide rescue breaths if necessary.
C - Circulation & Hemorrhage Control:
- Check for a pulse.
- Control bleeding: Apply direct pressure to any open wounds. Elevate the injured limb if possible.
D - Deformity / Disability (Immobilization):
- Immobilize the deformed limb before moving the patient, if possible and safe to do so.
- The goal is to avoid more harm and pain by using splints.
E - Exposure / Environment: Expose the injured area to properly assess, but ensure the patient is kept warm to prevent hypothermia.
II. Emergency Management of Suspected Fractures (On-Scene/Pre-Hospital)
The immediate goal is to stabilize the injury and prepare for safe transport.
- Immobilize Before Moving: If a fracture is suspected, the body part should be immobilized before the patient is moved.
- If the patient must be moved (e.g., from a vehicle) before splinting, the extremity should be carefully supported above and below the fracture site to prevent rotation and angular motion.
- Adequate Splinting:
- Purpose: To prevent movement of fracture fragments, which causes additional pain, soft tissue damage, and bleeding.
- Technique:
- Use temporary, well-padded splints. These can be improvised from available materials (e.g., rolled newspapers, magazines, pieces of wood) and firmly bandaged over clothing.
- Ensure the splint immobilizes the joint above and the joint below the fracture site.
- For long bones of the lower extremities, the unaffected leg can be used as a splint by bandaging the legs together.
- For upper extremity injuries, the arm can be bandaged to the chest, or a sling can be used for forearm injuries.
- Neurovascular Assessment:
- Crucial Step: Always assess the neurovascular status (circulation, sensation, movement) distal to the injury before and after splinting.
- Why: To determine the adequacy of peripheral tissue perfusion and nerve function and to identify any compromise caused or worsened by the injury or splinting.
- Managing Open Fractures:
- If there is an open wound (bone protruding or skin broken):
- Cover the wound with a clean (preferably sterile) dressing to prevent contamination of deeper tissues.
- DO NOT attempt to reduce the fracture or push any protruding bone back into the wound. This can introduce infection or cause further damage.
- Apply splints for immobilization over the dressing.
- Preparation for Transport: Once stabilized and splinted, the patient is ready for transport to a medical facility.
III. Emergency Department Evaluation
Upon arrival at the hospital:
- Complete Patient Evaluation: A thorough assessment of the patient's overall condition.
- Clothing Removal: Gently remove clothing, starting from the uninjured side, then the injured side. Clothing may need to be cut to avoid unnecessary movement of the fractured extremity.
- Minimal Movement: The fractured extremity should be moved as little as possible to prevent further damage and pain.
Hospital Management and Nursing Care for Fractures
This objective focuses on the comprehensive care provided to patients with fractures within the hospital setting, encompassing medical interventions, pain management, infection prevention, nutritional support, and the crucial role of nursing care in facilitating healing and recovery.
I. Hospital Management Principles
Hospital management of fractures builds upon the initial emergency care and is tailored to the specific class and type of fracture.
- Definitive Reduction and Immobilization: As discussed, this involves either closed reduction (manual manipulation) or open reduction (surgical exposure) followed by appropriate immobilization using methods such as:
- Casting/Splinting
- Traction (skin or skeletal)
- Open Reduction Internal Fixation (ORIF)
- External Fixation
- Pain Relief: Administer analgesics (e.g., NSAIDs, opioids) as prescribed to manage pain effectively. Pain control allows for participation in physical therapy and reduces patient distress.
- Antibiotics: Prophylactic antibiotics are administered promptly for open fractures to prevent infection (osteomyelitis), which is a severe complication.
- Supportive Treatment:
- Nutritional Supplements: Prescribe iron (FeSO4), folic acid (FA), and multivitamins to support healing and overall patient health.
- Calcium and Vitamin D: Crucial for bone formation and mineralization.
- Fluid Resuscitation: For patients who have experienced significant blood loss (e.g., from severe trauma or large bone fractures like femur/pelvis), fluid resuscitation is critical to maintain hemodynamic stability and prevent shock.
- Diagnostic Imaging:
- Bone X-rays: Used to confirm diagnosis, monitor reduction, assess healing progress, and evaluate alignment.
- Other imaging (CT, MRI) may be used as needed for complex cases (as discussed in Objective 3).
- Infection Prevention:
- Beyond antibiotics, strict adherence to aseptic techniques during wound care (especially for open fractures or pin sites with external fixators), surgical procedures, and overall patient care.
- Nutrition: Ensure adequate caloric, protein, and micronutrient intake to support the metabolic demands of bone healing. Hydration is also important.
- Exercises/Physiotherapy: Early introduction of prescribed exercises and physical therapy is vital to prevent complications of immobility and promote functional recovery.
II. Nursing Care
Nursing care is comprehensive and plays a pivotal role throughout the patient's hospital stay and during discharge planning.
- Encourage Early Activity: Encourage patients with closed (simple) fractures to return to their usual activities as rapidly as possible, within the limits of fracture immobilization. This helps prevent stiffness, muscle atrophy, and secondary complications.
- Patient Education for Self-Management:
- Swelling and Pain Control: Teach patients how to manage swelling (e.g., elevation, ice packs if appropriate) and administer pain medication.
- Activity Limits: Clearly explain the allowed and restricted activities based on the fracture type and stage of healing.
- Exercises: Teach exercises to maintain the health of unaffected muscles and to increase the strength of muscles needed for transfers and using assistive devices (e.g., crutches, walker, special utensils).
- Assistive Devices: Teach patients how to use assistive devices safely and correctly. Collaborate with physical and occupational therapists to ensure proper fitting and training.
- Home Environment Modification and Support: Assist with planning for necessary home environment modifications (e.g., removing tripping hazards, installing grab bars). Help secure personal assistance if needed for post-discharge care.
- Comprehensive Patient Teaching:
- Self-Care: Instructions on cast care, pin site care, wound care, hygiene.
- Medication Information: Dosage, frequency, side effects of prescribed medications.
- Monitoring for Complications: Educate on warning signs of complications (e.g., increased pain, swelling, numbness, fever, foul odor from cast/wound) and when to seek medical attention.
- Continuing Health Care Supervision: Emphasize the importance of follow-up appointments and ongoing rehabilitation.
- Neurovascular Assessment: Regularly assess the neurovascular status distal to the fracture site, especially when a cast, splint, or traction is applied. Report any changes immediately.
- Complication Prevention: Implement measures to prevent complications associated with immobility, such as:
- Deep Vein Thrombosis (DVT): Early mobilization, ankle pumps, antiembolism stockings, prophylactic anticoagulants.
- Pressure Ulcers: Regular repositioning, skin assessment, proper padding.
- Pneumonia/Atelectasis: Deep breathing exercises, incentive spirometry.
- Constipation: Adequate fluid intake, dietary fiber, stool softeners.
- Psychological Support: Provide emotional support and reassurance, as a fracture can be a frightening and debilitating experience.
Management Strategies for Fractures at Specific Anatomical Sites
The management of a fracture is significantly influenced by its location due to unique anatomical considerations, biomechanical forces, and potential for specific complications.
I. Upper Extremity Fractures
- Clavicle (Collar Bone) Fracture:
- Mechanism: Common injury from a fall or direct blow to the shoulder.
- Key Nursing Action:
- Neurovascular Monitoring: Monitor circulation and nerve function of the affected arm, comparing with the unaffected side. Disturbances can indicate neurovascular compromise.
- Activity Restrictions: Caution patient not to elevate the arm above shoulder level for about 6 weeks (until healed). Vigorous activity is limited for 3 months.
- Early Mobilization: Encourage exercises for the elbow, wrist, and fingers as soon as possible. Shoulder exercises as prescribed.
- Humeral Neck Fracture:
- Mechanism: Most frequent in older women after a fall on an outstretched arm.
- Key Nursing Action:
- Neurovascular Assessment: Evaluate the extent of injury and potential involvement of nerves and blood vessels of the arm.
- Immobilization: Teach patient to support the arm and immobilize it with a sling and swathe, securing the supported arm to the trunk.
- Early Motion: Begin pendulum exercises as soon as tolerated. Avoid vigorous activity for an additional 10-14 weeks.
- Patient Education: Inform about potential residual stiffness, aching, and limited range of motion for 6+ months. If displaced and fixed, exercises start post-immobilization.
- Humeral Shaft Fracture:
- Mechanism: Nerves and brachial blood vessels may be injured.
- Key Nursing Action:
- Neurovascular Assessment: Essential to monitor nerve and blood vessel status.
- Immobilization:
- Initially, well-padded splints to immobilize the upper arm.
- Support arm in 90 degrees of elbow flexion with a sling or collar and cuff.
- External fixators for open fractures.
- Functional bracing may also be used.
- Exercises: Teach and encourage pendulum shoulder exercises and isometric exercises as prescribed.
- Elbow Fracture (Distal Humerus):
- Mechanism: May injure median, radial, or ulnar nerves.
- Key Nursing Action:
- Neurovascular Assessment: Evaluate for paresthesia and signs of compromised circulation in the forearm and hand.
- Complication Monitoring: Monitor closely for Volkmann’s ischemic contracture (acute compartment syndrome) and hemarthrosis (blood in joint).
- Patient Education: Reinforce information regarding reduction, fixation, and planned active motion once swelling subsides and healing begins. Explain cast/splint care, and encourage active finger exercises.
- Early Motion: Gentle range-of-motion exercises for the injured joint about 1 week after internal fixation, if prescribed.
- Radial Head Fracture:
- Mechanism: Usually by a fall on an outstretched hand with the elbow extended.
- Key Nursing Action:
- Immobilization: Instruct patient in the use of a splint.
- Post-Op Care: For displaced fractures requiring surgery, reinforce the need for postoperative immobilization in a posterior plaster splint and sling.
- Early Motion: Encourage a program of active motion of the elbow and forearm when prescribed.
- Wrist Fracture (Distal Radius - Colles' Fracture):
- Mechanism: Usually from a fall on an open, dorsiflexed hand, common in elderly women with osteoporosis.
- Key Nursing Action:
- Cast/Incision Care: Reinforce care of the cast or, with wire insertion, teach incision care.
- Elevation: Instruct patient to keep the wrist and forearm elevated for 48 hours after reduction.
- Active Motion: Begin active motion of fingers and shoulder promptly to reduce swelling and prevent stiffness:
- Hold hand at heart level. Move fingers from full extension to flexion (10+ times/hour when awake).
- Use the hand in functional activities.
- Actively exercise shoulder and elbow (complete ROM).
- Neurovascular Assessment: Assess sensory function of median nerve (pricking distal index finger) and motor function (ability to touch thumb to little finger). Treat diminished circulation/nerve function promptly.
- Hand and Fingers Fractures:
- Management Goal: Regain maximum function of the hand.
- Key Nursing Action:
- Immobilization: Non-displaced fractures: finger splinted for 3-4 weeks. Displaced/open fractures: may require ORIF with wires/pins.
- Functional Use: Encourage functional use of uninvolved hand portions.
- Neurovascular Assessment: Evaluate neurovascular status of the injured hand.
- Swelling Control: Teach patient to control swelling by elevating the hand.
II. Lower Extremity and Trunk Fractures
- Pelvis Fracture:
- Mechanism: Falls, motor vehicle crashes, crush injuries. Often associated with multiple other severe injuries.
- Key Nursing Action:
- Symptom Monitoring: Monitor for ecchymosis, tenderness (pubis, iliac spines, crest, sacrum, coccyx), edema, numbness/tingling (pubis, genitals, thighs), inability to bear weight.
- Neurovascular Assessment: Complete neurovascular assessment of lower extremities to detect injury to pelvic blood vessels and nerves.
- Hemodynamic Stability & Mobility: Promote hemodynamic stability and comfort. Encourage early mobilization as pain resolves, using assistive devices for protected weight-bearing. Unstable fractures may require external fixation or ORIF.
- Complication Monitoring:
- Urinary Tract: Examine urine for blood. In males, do not insert a catheter until urethral status is known.
- Abdominal: Monitor for diffuse abdominal pain, altered bowel sounds, rigidity, resonance/dullness (suggesting intestinal injury/bleeding).
- Hemorrhage/Shock: Monitor for signs of shock. Palpate lower extremities for absence of peripheral pulses (torn iliac artery).
- Bladder, Rectum, Intestines, Vessels, Nerves: Assess for injuries to these structures.
- Stable Pelvic Fractures: Bed rest for a few days, symptom management. Provide fluids, dietary fiber, ankle/leg exercises, antiembolism stockings, logrolling, deep breathing, skin care. Monitor bowel sounds.
- Coccyx Fracture: For pain with sitting/defecation, assist with sitz baths, administer stool softeners.
- Femur and Hip Fractures (Femoral Shaft):
- Mechanism: Most often young adults in MVCs or falls from heights. Frequently associated with multiple trauma and significant blood loss (2-3 units).
- Key Nursing Action:
- Neurovascular Assessment: Assess neurovascular status of the extremity, especially circulatory perfusion of the lower leg and foot (popliteal, posterior tibial, pedal pulses, capillary refill, Doppler).
- Complication Monitoring: Note signs of hip and knee dislocation, knee effusion (suggesting ligament damage/instability).
- Immobilization/Fixation: Apply and maintain skeletal traction or splint to achieve muscle relaxation and alignment before ORIF. Later, a cast brace.
- Weight Bearing: Assist with minimal partial weight-bearing when indicated, progressing to full as tolerated. Cast brace worn for 12-14 weeks.
- Exercises: Instruct and encourage regular exercises of lower leg, foot, and toes. Assist with active/passive knee exercises as soon as possible, depending on stability.
- Tibia and Fibula Fractures:
- Mechanism: Direct blow, falls with foot flexed, violent twisting motion. Most common fractures below the knee.
- Key Nursing Action:
- Cast/Brace Care: Instruction on care of long leg walking cast, patellar-tendon-bearing cast, or short leg cast/brace (for knee motion after 3-4 weeks).
- Weight Bearing: Instruct and assist with partial weight-bearing (usually 7-10 days), progressing to full weight-bearing (4-8 weeks).
- Skeletal Traction: Instruction on care if applicable.
- Exercises: Encourage hip, foot, and knee exercises within device limits.
- Elevation: Instruct patient to elevate extremity to control edema.
- Neurovascular Evaluation: Perform continuous neurovascular evaluation.
- Rib Fracture:
- Mechanism: Occur frequently in adults, usually from blunt trauma.
- Key Nursing Action:
- Pain Management & Respiratory Support: Assist patient to cough and deep breath by splinting the chest with hands or a pillow. Reassure that pain diminishes in 3-4 days and heals in 6 weeks.
- Complication Monitoring: Monitor for atelectasis, pneumonia, flail chest, pneumothorax, and hemothorax.
Manage Fracture Complications
1. Shock
A life-threatening condition characterized by inadequate tissue perfusion. Can result from significant blood loss associated with severe fractures (e.g., pelvis, femur) or trauma.
Manifestations: Hypotension, tachycardia, pallor, cool clammy skin, altered mental status.
Management:
- Stabilizing the fracture: To prevent further hemorrhage.
- Restoring blood volume and circulation: IV fluids, blood transfusions.
- Relieving pain: Analgesics.
- Proper immobilization: To reduce further injury.
- Protection from further injury and complications.
2. Fat Embolism Syndrome (FES)
Blockage of small blood vessels in organs (brain, lungs, kidneys) by fat globules, typically originating from bone marrow after long bone fractures (especially femur, pelvis).
Manifestations:
- Onset: Sudden, usually within 12-48 hours (can be up to 10 days).
- Respiratory: Hypoxia, tachypnea, tachycardia, dyspnea, crackles, wheezes, precordial chest pain, cough, large amounts of thick white sputum.
- Neurological: Changes in mental status (confusion, restlessness), headache, visual disturbances.
- Cutaneous: Petechial rash (classic, but not always present) on chest, neck, axillae.
- Other: Pyrexia (fever).
Management: Primarily supportive and preventative.
- Immediate immobilization: Of fractures.
- Adequate support: For fractured bones during turning and positioning.
- Fluid and electrolyte balance maintenance.
- Prompt respiratory support: Oxygen therapy, ventilation if severe. Prevention of respiratory and metabolic acidosis.
- Medications: Corticosteroids (reduce inflammation), vasopressor medications (maintain BP).
3. Compartment Syndrome
A serious condition where increased pressure within a confined muscle compartment compromises circulation and nerve function. Can be acute (traumatic injury) or chronic (overuse).
Causes: Tight casts/dressings, increased muscle compartment contents due to edema or hemorrhage.
Manifestations (The "6 Ps" - not all may be present initially):
- Pain: Deep, throbbing, unrelenting pain not controlled by opioids; pain with passive stretching of the muscles in the compartment.
- Pallor: Pale or dusky fingers/toes.
- Paresthesia: Numbness, tingling.
- Pulselessness: Diminished or absent pulse (a late and ominous sign).
- Paralysis: Motor weakness or inability to move the extremity (late sign).
- Poikilothermia: Cool extremity.
- Other signs: Cyanotic nail beds, prolonged capillary refill (>3 seconds).
Management:
- Control swelling: Elevate extremity to heart level (not above, as this can reduce arterial inflow).
- Release restrictive devices: Loosen or remove dressings, bivalve (cut along both sides) or remove casts.
- Fasciotomy: Surgical decompression with excision of the fascia to relieve pressure. The wound remains open and covered with moist sterile saline dressings for 3-5 days.
- Post-fasciotomy: Limb is splinted and elevated. Prescribed passive range-of-motion exercises every 4-6 hours.
4. Venous Thromboembolism (VTE)
Includes Deep Vein Thrombosis (DVT - blood clot in deep vein, usually leg) and Pulmonary Embolism (PE - DVT dislodges and travels to lungs). High risk due to immobility, trauma, surgery.
Manifestations:
- DVT: Swelling, pain, tenderness, warmth, redness in the affected extremity (often calf).
- PE: Sudden shortness of breath, chest pain, cough, tachycardia, anxiety, feeling of impending doom.
Management:
- Prevention: Early ambulation/mobilization, compression stockings, sequential compression devices (SCDs), prophylactic anticoagulants (heparin, enoxaparin, fondaparinux).
- Treatment (DVT): Anticoagulation.
- Treatment (PE): Anticoagulation, oxygen, thrombolytics, embolectomy in severe cases.
5. Disseminated Intravascular Coagulation (DIC)
A serious disorder where widespread activation of the clotting cascade leads to simultaneous widespread clotting and bleeding. Often triggered by severe trauma, sepsis, or shock.
Manifestations:
- Unexpected bleeding: From surgical sites, mucous membranes, venipuncture sites, GI and urinary tracts.
- Signs of clotting (less common in trauma-induced DIC, but possible): purpura, petechiae, ecchymoses.
Management: Treat the underlying cause (e.g., trauma, sepsis). Support organ function. Blood product transfusions (platelets, FFP) to replace clotting factors. Anticoagulants (heparin) in specific circumstances.
6. Infection
Bacterial contamination of the fracture site, especially common with open fractures or surgical interventions. Can lead to osteomyelitis.
Manifestations: Tenderness, pain, redness, swelling, local warmth, elevated temperature (fever), purulent drainage.
Management:
- Prevention: Strict aseptic technique during wound care and surgery. Prophylactic antibiotics for open fractures.
- Treatment: Antibiotics (often long-term, IV), debridement (surgical removal of infected tissue), wound irrigation, possible removal of infected internal fixation devices.
Other Complications:
- Delayed Union: Healing of the fracture takes longer than the expected time frame.
- Manifestations: Persistent pain and tenderness at the fracture site beyond the normal healing period. X-rays show incomplete bridging callus.
- Management: Continued immobilization, often with non-weight-bearing. May involve electrical bone stimulation, low-intensity pulsed ultrasound, or revision surgery if severe.
- Malunion: The fracture heals in an unacceptable anatomical position, leading to deformity or functional impairment.
- Management: May require osteotomy (surgical cutting and realignment of bone) to correct the deformity.
- Nonunion: Failure of the bone ends to unite at all, even after an extended period (typically 6-9 months).
- Manifestations: Persistent discomfort and abnormal movement at the fracture site. X-rays show no evidence of healing and a persistent fracture line.
- Risk Factors: Infection, interposition of tissue between bone ends, inadequate immobilization, manipulation that disrupts callus formation.
- Management:
- Internal fixation: With or without bone grafting.
- Bone grafting: Autograft (from patient) or allograft (from donor) to provide osteogenic cells and structural support.
- Electrical bone stimulation: To promote bone growth.
- Combination of these approaches.
- Avascular Necrosis (AVN) of Bone: Death of bone tissue due to interruption of blood supply. Common in fractures involving the femoral head, scaphoid, and talus.
- Manifestations: Pain, functional limitation, eventual collapse of the bone.
- Management: Non-weight-bearing, medications, core decompression, bone grafting, joint replacement (if severe).
- Reaction to Internal Fixation Devices: Pain, infection, loosening, or corrosion of plates, screws, rods.
- Management: Removal of hardware, revision surgery.
- Complex Regional Pain Syndrome (CRPS, formerly RSD): Chronic condition of severe burning pain, swelling, and changes in skin color/temperature, affecting an extremity after trauma (not necessarily severe).
- Management: Pain management (nerve blocks, medications), physical therapy, occupational therapy, psychological support.
- Heterotopic Ossification: Presence of bone in soft tissue where bone normally does not exist. Can lead to joint stiffness and pain.
- Management: Range of motion exercises, NSAIDs, radiation therapy (prophylactic), surgical excision.
Nursing Diagnoses for Fracture Patients
- Acute Pain related to muscle spasms, trauma, edema, and immobilization.
- Impaired Physical Mobility related to skeletal injury, pain, cast/splint/traction, activity restrictions.
- Risk for Ineffective Peripheral Tissue Perfusion related to vascular compromise, edema, tight immobilization device, or immobility.
- Risk for Impaired Skin Integrity related to immobilization devices (casts, splints), pressure, surgical incisions, or altered sensation.
- Risk for Infection related to open fracture, surgical wound, or presence of external fixation devices.
- Excessive Anxiety related to injury, pain, potential for permanent disability, prolonged recovery, or financial concerns.
- Inadequate health Knowledge related to fracture care, immobilization device care, medication regimen, activity restrictions, and signs of complications.
- Self-Care Deficit (specify: bathing, dressing, toileting, feeding) related to pain, impaired mobility, or immobilization device.
- Risk for Constipation related to immobility, pain medication side effects (opioids), and decreased fluid/fiber intake.
- Risk for Ineffective Breathing Pattern / Impaired Gas Exchange related to pain (especially rib fractures), immobility, or prolonged supine positioning.
NURSING INTERVENTIONS
These interventions are applicable across various fracture types and aim to address the identified nursing diagnoses.
A. Pain Management:
| Intervention |
Detail/Rationale |
| Assessment |
- Regularly assess pain using a standardized pain scale (e.g., 0-10).
- Note characteristics: location, intensity, quality, duration, precipitating factors.
- Evaluate effectiveness of pain interventions.
|
| Medication Administration |
Administer prescribed analgesics (opioids, NSAIDs, muscle relaxants) on a scheduled basis or PRN, ensuring timely delivery. |
| Elevation |
Elevate the injured extremity to reduce swelling and pressure (ensure it's not elevated above heart level if compartment syndrome is suspected). |
| Cold Therapy |
Apply cold packs (if appropriate and not contraindicated by cast/dressing) to reduce swelling and numb the area. |
| Immobilization |
Ensure proper alignment and immobilization of the fracture site. |
| Comfort Measures |
Provide comfort measures: repositioning, back rubs, distraction, guided imagery, relaxation techniques. |
| Education |
Educate patient on reporting increased or unrelieved pain, especially if different in quality (e.g., "throbbing," "burning"). |
B. Mobility and Functional Independence:
| Intervention |
Detail/Rationale |
| Assessment |
- Assess pre-injury mobility level and current functional limitations.
- Evaluate ability to perform ADLs and use assistive devices.
|
| Early Mobilization |
Encourage and assist with early mobilization within prescribed limits (e.g., bed exercises, transfers, ambulation with assistive devices). |
| Therapy Collaboration |
Collaborate with physical and occupational therapy for specific exercise programs, ambulation training, and adaptive equipment. |
| Repositioning |
Assist with repositioning in bed, emphasizing proper body mechanics and protection of the injured limb. |
| Transfer Training |
Teach techniques for safe transfers (bed to chair, chair to toilet). |
| Exercise |
Encourage active range-of-motion exercises for unaffected joints to prevent stiffness and muscle atrophy. |
| Assistive Devices |
Provide assistive devices (crutches, walker, cane) and ensure proper fit and patient education on their safe use. |
C. Neurovascular Monitoring:
| Intervention |
Detail/Rationale |
| Assessment (The 6 Ps) |
- Pain: Any new, increasing, or unrelieved pain, especially with passive stretch.
- Pallor: Skin color distal to the injury (pale, dusky, cyanotic).
- Paresthesia: Numbness, tingling, burning sensations.
- Pulselessness: Presence and quality of peripheral pulses. Compare bilaterally. (Use Doppler if necessary).
- Paralysis: Ability to move digits/joints distal to the injury.
- Poikilothermia: Temperature of the skin distal to the injury (coolness).
- Assess capillary refill time (<3 seconds is normal).
- Monitor for edema and swelling.
|
| Immediate Action |
Immediately report any changes or worsening neurovascular status to the physician. |
| Elevation/Positioning |
Elevate the affected extremity to heart level (unless compartment syndrome is suspected, then do not elevate above heart level). |
| Device Management |
Loosen restrictive dressings or casts as indicated and ordered. Do NOT apply ice if neurovascular compromise is suspected. |
D. Skin and Wound Care:
| Intervention |
Detail/Rationale |
| Assessment |
- Inspect skin under and around casts/splints for redness, pressure points, blisters, or irritation.
- For open fractures or surgical sites, assess wounds for signs of infection (redness, swelling, warmth, pain, purulent drainage).
- Monitor pin sites for external fixators for signs of infection or loosening.
|
| Cast/Splint Care |
Maintain cleanliness and dryness of skin under casts/splints. Do not insert objects into casts. |
| Wound Care |
Provide meticulous wound care, dressing changes, and pin site care using aseptic technique as prescribed. |
| Repositioning |
Reposition patient frequently to relieve pressure on bony prominences and promote circulation. Provide padding where skin is at risk. |
| Education |
Educate patient/family on proper skin and wound care, and signs to report. |
E. Infection Prevention:
| Intervention |
Detail/Rationale |
| Assessment |
Monitor temperature, WBC count, and wound/pin site appearance for signs of infection. |
| Antibiotics |
Administer prophylactic and therapeutic antibiotics as prescribed. |
| Asepsis |
Maintain strict aseptic technique during all wound and pin site care. |
| Hygiene |
Ensure proper hand hygiene. |
| Systemic Monitoring |
Monitor for systemic signs of infection (fever, chills, malaise). |
F. Patient Education and Psychological Support:
| Intervention |
Detail/Rationale |
| Assessment |
Assess patient's understanding of their injury, treatment plan, and self-care needs. Evaluate coping mechanisms. |
| Education Topics |
Provide clear education on: Care of immobilization devices, Activity restrictions, Medication regimen, Signs of complications, Nutritional requirements, Use of assistive devices, Follow-up plan. |
| Emotional Support |
Allow patient to express fears, concerns, and frustrations. Provide reassurance. Connect with social services if needed. |
G. Elimination:
| Intervention |
Detail/Rationale |
| Assessment |
Monitor bowel movements, listen for bowel sounds. Assess for abdominal distention. |
| Diet/Fluids |
Encourage adequate fluid intake and dietary fiber to prevent constipation. |
| Medications |
Administer stool softeners or laxatives as prescribed. |
| Mobility |
Encourage mobility as tolerated to stimulate bowel function. |
| Comfort |
Provide privacy and comfortable positioning for elimination. |
H. Respiratory Support (especially for rib fractures or prolonged immobility):
| Intervention |
Detail/Rationale |
| Assessment |
Monitor respiratory rate, depth, and effort. Auscultate lung sounds. Assess for pain with breathing. |
| Pulmonary Hygiene |
Encourage deep breathing exercises and incentive spirometry every 1-2 hours while awake. |
| Splinting |
Assist with coughing, splinting the chest for rib fractures. |
| Positioning |
Reposition frequently to promote lung expansion and prevent atelectasis. |
| Pain Control |
Administer pain medication to facilitate respiratory effort. |