Topic: Structures and functions of various body systems - Lymphatic System (PEX 1.8.2)
I. Introduction
The human body is home to a vast number of bacterial cells, estimated to be at least 10 times more than human cells.
Some of these bacteria are beneficial for health (e.g., aiding digestion).
Others are potentially disease-causing (pathogenic).
The Immune System is a functional system rather than a distinct organ system. It consists of a cell population that inhabits all organs and defends the body from agents of disease.
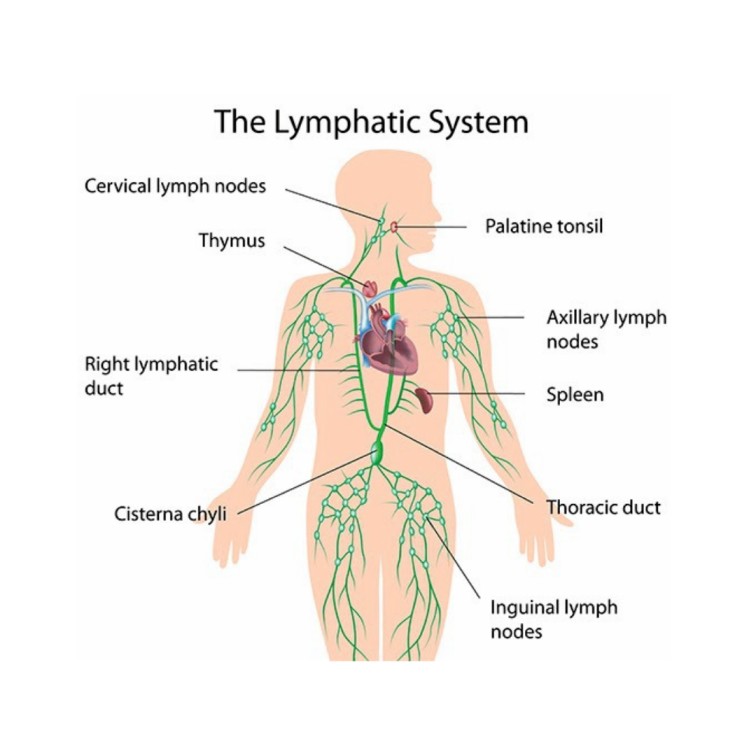
Immune cells are especially concentrated in a true organ system called the Lymphatic System.
Functions of the Lymphatic System:
- Fluid Recovery: Recovers excess tissue fluid.
- Immunity: Inspects the recovered fluid for disease agents and activates immune responses.
- Lipid Absorption: Absorbs dietary lipids from the small intestine.
Fluid Recovery in Detail:
Fluid continually filters out of blood capillaries into the surrounding tissue spaces.
About 85% of this fluid is reabsorbed by blood capillaries.
The remaining 15% (amounting to 2-4 liters per day) and approximately half of the plasma proteins enter the lymphatic system and are eventually returned to the blood. This prevents edema (tissue swelling).

Immunity:
As the lymphatic system recovers fluid, it also picks up foreign cells, chemicals, and pathogens that may be present in the tissues.
This fluid passes through lymph nodes, where immune cells (lymphocytes and macrophages) monitor for foreign matter.
Detection of pathogens triggers a protective immune response.
Lipid Absorption:
Specialized lymphatic capillaries called lacteals within the small intestine are responsible for absorbing dietary lipids that cannot be absorbed directly into blood capillaries.
The fatty lymph in these vessels is called chyle.
Components of the Lymphatic System:
- Lymph: The recovered fluid.
- Lymphatic Vessels: Transport the lymph.
- Lymphatic Tissues: Aggregations of lymphocytes and macrophages within connective tissues.
- Lymphatic Organs: Structures with concentrated immune cells, separated from surrounding tissues by a connective tissue capsule.
Lymph:
Clear, colorless fluid, similar to plasma but with much less protein.
Originates as extracellular fluid drawn into lymphatic capillaries.
Chemical composition varies depending on location (e.g., fatty chyle from intestines, lymph rich in lymphocytes after passing through lymph nodes).
Lymphatic Capillaries (Terminal Lymphatics):
Microscopic vessels that penetrate nearly every tissue (absent from CNS, cartilage, cornea, bone, bone marrow).
Closed at one end.
Walls are single layer of endothelial cells with overlapping edges like roof shingles.
Endothelial cells are tethered to surrounding tissue by protein filaments.
Overlapping cells form valve-like flaps that open when interstitial fluid pressure is high (allowing fluid and large particles in) and close when it is low (preventing backflow).

Lymphatic Vessels (Structure and Organization):
Larger vessels are composed of three layers (tunics), similar to veins:
- Tunica interna: Endothelium and valves.
- Tunica media: Elastic fibers, smooth muscle (for rhythmic contraction).
- Tunica externa: Thin outer layer.
Converge into larger and larger vessels (collecting vessels, trunks, ducts).
Collecting vessels course through many lymph nodes.

Lymphatic Trunks and Collecting Ducts:
Six lymphatic trunks drain major portions of the body: Jugular, subclavian, bronchomediastinal, intercostal, intestinal (unpaired), and lumbar trunks.
These trunks merge into two collecting ducts:
- Right lymphatic duct: Receives lymph from the right arm, right side of head and thorax; empties into the right subclavian vein.
- Thoracic duct: Larger and longer; begins as the cisterna chyli in the abdomen (receives lymph from below diaphragm, intestinal, and lumbar trunks); ascends through the thorax receiving lymph from the left arm, left side of head, neck, and thorax; empties into the left subclavian vein.
Lymph is returned to the blood circulation via the Subclavian veins.


Major Lymphatic Vessels
Flow of Lymph:
Lymph flows under forces similar to those governing venous return, but there is no pump like the heart.
Flow is at low pressure and slower speed than venous blood.
Moved along by:
- Rhythmic contractions of the lymphatic vessels themselves (stretching stimulates contraction).
- Skeletal muscle pump.
- Arterial pulsation rhythmically squeezing lymphatic vessels.
- Thoracic pump (pressure changes during breathing) aids flow from abdominal to thoracic cavity.
- Valves prevent backward flow.
- Rapidly flowing blood in subclavian veins draws lymph into them.
Exercise significantly increases lymphatic return.
III. Lymphatic Cells
Major Lymphatic Cells:
- Natural killer (NK) cells
- T lymphocytes (T cells)
- B lymphocytes (B cells)
- Macrophages
- Dendritic cells
- Reticular cells
Natural Killer (NK) Cells:
Large lymphocytes that continually patrol the body for pathogens and diseased host cells.
Attack and destroy bacteria, transplanted cells, virus-infected cells, and cancer cells.
Recognize enemy cell and bind to it.
Release proteins called perforins (polymerize to create a hole in the plasma membrane).
Secrete protein-degrading enzymes called granzymes (enter through pore and induce apoptosis/programmed cell death).

T lymphocytes (T cells):
Mature in the thymus. Involved in cellular immunity and coordination. (Detailed development and function discussed later).
B lymphocytes (B cells):
Mature in bone marrow. Activation causes proliferation and differentiation into plasma cells that produce antibodies. Involved in humoral immunity. (Detailed development and function discussed later).
Macrophages:
Large, avidly phagocytic cells of connective tissue.
Develop from monocytes that emigrate from blood.
Phagocytize tissue debris, dead neutrophils, bacteria, and other foreign matter.
Process foreign matter and display antigenic fragments to T cells, acting as Antigen-Presenting Cells (APCs).

Dendritic cells:
Branched, mobile APCs found in epidermis, mucous membranes, and lymphatic organs.
Alert immune system to pathogens that have breached the body surface.
Reticular cells:
Branched stationary cells that contribute to the stroma (structural framework) of a lymphatic organ.
IV. Lymphatic Tissues
Lymphatic (lymphoid) tissue: Aggregations of lymphocytes in the connective tissues of mucous membranes and various organs.
Diffuse lymphatic tissue:
Simplest form; lymphocytes scattered (not clustered).
Prevalent in body passages open to the exterior (respiratory, digestive, urinary, reproductive tracts).
Collectively called Mucosa-associated lymphatic tissue (MALT).
Lymphatic nodules (follicles):
Dense masses of lymphocytes and macrophages that congregate in response to pathogens.
Constant feature of lymph nodes, tonsils, and appendix.
Peyer patches: Dense clusters in the ileum (distal portion of the small intestine).

V. Lymphatic Organs
Lymphatic organs: Anatomically well-defined structures containing lymphatic tissue.
Have a connective tissue capsule that separates lymphatic tissue from neighboring tissues.
Primary lymphatic organs:
Sites where T and B cells become immunocompetent (able to recognize and respond to antigens).
Secondary lymphatic organs:
Immunocompetent cells populate these tissues; sites where immune responses are initiated.
- Lymph nodes
- Tonsils
- Spleen
Red Bone Marrow:
Involved in hemopoiesis (blood formation) and immunity (B cell maturation).
Soft, loosely organized, highly vascular material.
Separated from osseous tissue by endosteum.
As blood cells mature, they push through reticular and endothelial cells to enter sinusoids and flow into the bloodstream.

Thymus:
Member of endocrine, lymphatic, and immune systems.
Houses developing T lymphocytes (thymocytes).
Secretes hormones regulating T cell activity (thymosin, thymopoietin, etc.).
Bilobed organ in superior mediastinum.
Undergoes degeneration (involution) with age.
Fibrous capsule gives off trabeculae (septa) dividing the gland into lobes (cortex and medulla).
Reticular epithelial cells form the blood–thymus barrier (seals off cortex from medulla), preventing antigens from reaching developing T cells.

Lymph Nodes:
Most numerous lymphatic organs (about 450 in a young adult).
Serve two functions: Cleanse the lymph and act as a site of T and B cell activation.
Elongated, bean-shaped structure with a hilum (where vessels exit/enter).
Enclosed by a fibrous capsule with trabeculae dividing the interior into compartments.
Stroma of reticular fibers and reticular cells provides framework.
Parenchyma divided into cortex (with germinal centers where B cells multiply) and medulla.
Lymph enters through several afferent lymphatic vessels along the convex surface.
Lymph leaves through one to three efferent lymphatic vessels at the hilum.
Regional Concentrations:
Cervical (neck), Axillary (armpit), Thoracic (mediastinum), Abdominal (abdominopelvic wall), Intestinal and mesenteric (mesenteries), Inguinal (groin), Popliteal (back of knee).

Lymph Node Conditions:
- Lymphadenitis: Swollen, painful node responding to foreign antigen.
- Lymphadenopathy: Collective term for all lymph node diseases.
Lymph Nodes and Metastatic Cancer:
Metastasis: Cancerous cells break free from original tumor, travel to other sites, and establish new tumors.
Metastasizing cells easily enter lymphatic vessels.
Tend to lodge in the first lymph node they encounter (sentinel node).
Multiply there, eventually destroying the node; typically swollen, firm, and usually painless.
Tend to spread to the next node downstream.
Treatment (e.g., breast cancer) often involves removal of nearby lymph nodes to check for metastasis.
Tonsils:
Patches of lymphatic tissue at the entrance to the pharynx.
Guard against ingested or inhaled pathogens.
Covered with epithelium that forms deep pits: tonsillar crypts lined with lymphatic nodules. Pathogens get into crypts and encounter lymphocytes.
Inflammation is tonsillitis; surgical removal is tonsillectomy.
Three main sets: Palatine tonsils (posterior oral cavity margin, most infected), Lingual tonsils (root of tongue), Pharyngeal tonsil (adenoids, wall of nasopharynx).

Spleen:
The body’s largest lymphatic organ.
Parenchyma exhibits two types of tissue:
- Red pulp: Sinusoids filled with erythrocytes; filters old RBCs.
- White pulp: Lymphocytes, macrophages surrounding splenic artery branches; immune surveillance of blood.

Spleen Functions:
- Filters old, fragile RBCs ("erythrocyte graveyard").
- Blood cell production in fetus (minor in anemic adults).
- Monitors blood for foreign antigens (white pulp).
- Stabilizes blood volume (plasma transfers to lymphatic system).
Vulnerability: Highly vascular and vulnerable to trauma and infection.
Ruptured spleen requires splenectomy, which leaves the person susceptible to future infections, premature death.
VI. Nonspecific Resistance (Innate Immunity)
Body's Lines of Defense:
- First line: Skin and mucous membranes (external barriers).
- Second line: Several nonspecific defense mechanisms (leukocytes, antimicrobial proteins, inflammation, fever).
- Third line: The immune system (adaptive immunity) - specific, with memory.
Nonspecific defenses: Guard equally against a broad range of pathogens.
Lack capacity to remember pathogens.
Include protective proteins, protective cells, and protective processes.
Specific or adaptive immunity: Body must develop separate immunity to each pathogen.
Body adapts to a pathogen and wards it off more easily upon future exposure (memory).
External Barriers:
- Skin: Mechanically difficult for microbes to enter. Toughness of keratin, dry, nutrient-poor. Acid mantle (lactic/fatty acids) inhibits bacterial growth. Contains antimicrobial peptides (dermicidin, defensins, cathelicidins).
- Mucous membranes: Line passages open to exterior. Protected by mucus (physically traps microbes) and lysozyme (destroys bacterial cell walls).
- Subepithelial areolar tissue: Viscous barrier of hyaluronic acid. Hyaluronidase (enzyme used by pathogens) makes it less viscous.
Leukocytes and Macrophages:
(See Section III above for cell types)
- Neutrophils: Wander connective tissue killing bacteria. Kill using phagocytosis/digestion or producing bactericidal chemicals (respiratory burst, killing zone).
- Eosinophils: Found in mucous membranes. Guard against parasites, allergens, other pathogens. Kill large parasites (superoxide, toxic proteins). Promote basophil/mast cell action. Phagocytize antigen–antibody complexes. Limit histamine/inflammatory chemicals.
- Basophils: Secrete chemicals aiding mobility/action of other leukocytes. Leukotrienes (activate/attract neutrophils/eosinophils). Histamine (vasodilator, increases blood flow). Heparin (inhibits clot formation, prevents impeding leukocyte mobility).
- Mast cells: Connective tissue cells similar to basophils; secrete similar substances.
- Lymphocytes: T, B, NK cells. (See Section III above for types; detailed adaptive roles later).
- Monocytes: Emigrate from blood into connective tissues and transform into macrophages.
- Macrophage system: All avidly phagocytic cells (except circulating leukocytes). Wandering macrophages (actively seek pathogens). Fixed macrophages (phagocytize what comes to them) e.g., Microglia (CNS), Alveolar macrophages (lungs), Hepatic macrophages (liver).
Antimicrobial Proteins:
Inhibit microbial reproduction, provide short-term, nonspecific resistance.
- Interferons: Secreted by virus-infected cells. Alert neighboring cells (bind to receptors, activate second messengers). Alerted cells synthesize antiviral proteins. Also activate NK cells and macrophages. Activated NK cells destroy infected/malignant cells.
- Complement system: Group of 30+ globular proteins synthesized mainly by liver. Circulate in inactive form, activated by pathogen presence. Powerful contributions to nonspecific resistance and adaptive immunity.
Complement System Activation Pathways:
- Classical pathway: Requires antibody bound to antigen (part of adaptive immunity). Ag-Ab complex changes antibody shape, exposing complement-binding sites. C1 binding sets off cascade (complement fixation).
- Alternative pathway: Nonspecific, does not require antibody. C3 breaks down to C3a/C3b; C3b binds directly to targets (tumor cells, viruses, bacteria, yeasts). Triggers autocatalytic cascade forming more C3.
- Lectin pathway: Nonspecific. Lectins (plasma proteins) bind to carbohydrates on microbial surface. Sets off C3 production cascade.
Mechanisms of Action of Complement Proteins:
- Inflammation: C3a (and C5a) stimulate mast cells/basophils to secrete histamine/inflammatory chemicals. Activate and attract neutrophils/macrophages. Speeds pathogen destruction in inflammation.
- Immune clearance: C3b binds Ag-Ab complexes; RBCs transport complexes to liver/spleen. Macrophages strip/destroy complexes. Principal means of clearing foreign antigens from bloodstream.
- Phagocytosis: C3b assists by opsonization (coats microbial cells, serves as binding sites for phagocytes, makes foreign cell more appetizing).
- Cytolysis: C3b splits C5 to C5a/C5b; C5b binds enemy cell. Attracts more complement proteins forming membrane attack complex (MAC). MAC forms a hole in target cell; electrolytes leak, water flows in, cell ruptures.
Fever:
Abnormal elevation of body temperature (pyrexia, febrile).
Results from trauma, infections, drug reactions, tumors, etc.
Adaptive defense (in moderation): Promotes interferon activity, elevates metabolic rate/tissue repair, inhibits reproduction of bacteria/viruses.
Antipyretics (aspirin, ibuprofen) inhibit Prostaglandin E2 synthesis.
Triggered by exogenous pyrogens (from pathogens) and endogenous pyrogens (secreted by neutrophils/macrophages, stimulate hypothalamus to raise set point via PGE2).
Stages: Onset, Stadium, Defervescence.
Reye Syndrome: Serious disorder in children after viral infection (chickenpox/flu). Swelling brain neurons, fatty liver infiltration, pressure leads to nausea, vomiting, disorientation, seizures, coma (30% die). Triggered by aspirin use for fever. Never give aspirin to children with chickenpox or flu-like symptoms.
Inflammation:
Local defensive response to tissue injury (trauma, infection).
General purposes: Limits spread of pathogens, destroys them, removes debris, initiates tissue repair.
Four cardinal signs: Redness, swelling, heat, pain. (Suffix -itis denotes inflammation).
Cytokines (small proteins) regulate inflammation/immunity: Secreted by leukocytes; alter receiving cell physiology; act at short range (paracrines/autocrines); include interferon, interleukins, TNF, chemotactic factors.
Three Major Processes of Inflammation:
- Mobilization of body defenses: Get defensive leukocytes to site quickly. Achieved by local hyperemia (increased blood flow via vasodilation due to vasoactive chemicals like histamine, leukotrienes, cytokines). Hyperemia also washes toxins. Vasoactive chemicals increase capillary permeability (widens gaps). Selectins (cell-adhesion molecules) make endothelium sticky (margination). Leukocytes crawl through gaps (diapedesis/emigration). Cells/chemicals that left blood are extravasated. Basis for cardinal signs (Heat=hyperemia; Redness=hyperemia+extravasated RBCs; Swelling=increased fluid filtration; Pain=nerve injury/pressure/prostaglandins/bradykinin).
- Containment and destruction of pathogens: Prevent pathogens from spreading. Fibrinogen filters into tissue fluid, forms fibrin clot (sticky mesh walls off microbes). Heparin prevents clotting at site. Pathogens contained in fluid pocket, attacked by antibodies/phagocytes/defenses. Neutrophils (chief enemy of bacteria) accumulate within an hour, exhibit chemotaxis (attraction to chemicals like bradykinin/leukotrienes). Neutrophils phagocytize, respiratory burst. Macrophages/T cells secrete colony-stimulating factor (stimulates leukopoiesis, raising WBC counts). Neutrophilia (bacterial infection), Eosinophilia (allergy/parasitic).
- Tissue cleanup and repair: Monocytes (primary agents) arrive later (8-12 hrs), become macrophages. Engulf/destroy bacteria, damaged cells, dead neutrophils. Edema contributes: Swelling compresses veins (reduces venous drainage), forces open lymphatic capillary valves (promotes lymphatic drainage). Lymphatics collect/remove bacteria, debris, proteins better than blood capillaries. Pus (yellow accumulation of dead neutrophils, bacteria, debris, fluid). Abscess (accumulation of pus in tissue cavity). Platelet-derived growth factor (secreted by platelets/endothelial cells) stimulates fibroblasts to multiply/synthesize collagen. Hyperemia delivers oxygen, amino acids for protein synthesis. Increased heat increases metabolic rate, speeds mitosis/tissue repair. Pain limits use of body part, allows chance to rest/heal.
VII. General Aspects of Adaptive Immunity (Specific Immunity)
Immune system: Large population of widely distributed cells that recognize foreign substances and neutralize/destroy them.
Distinguished from nonspecific resistance by:
- Specificity: Immunity directed against a particular pathogen.
- Memory: Reacts quickly with no noticeable illness upon reexposure to same pathogen.
Forms of Immunity:
- Cellular (cell-mediated) immunity: Lymphocytes (T cells) directly attack/destroy foreign cells or diseased host cells. Rids body of pathogens inside human cells (inaccessible to antibodies). Kills cells that harbor them.
- Humoral (antibody-mediated) immunity: Mediated by antibodies. Antibodies do not directly destroy pathogen but tag it for destruction. Many antibodies dissolved in body fluids ("humors"). Works against extracellular stages of infections by microorganisms.
- Natural active immunity: Production of one's own antibodies/T cells from infection or natural exposure to antigen.
- Artificial active immunity: Production of one's own antibodies/T cells from vaccination. Vaccine (dead/attenuated pathogens) stimulates immune response without causing disease. Booster shots (periodic immunizations) stimulate memory.
- Natural passive immunity: Temporary immunity from antibodies produced by another person (fetus from mother via placenta/milk).
- Artificial passive immunity: Temporary immunity from injection of immune serum (antibodies) from another person/animal (treatment for snakebite, botulism, rabies, tetanus).
Antigens:
Any molecule that triggers an immune response.
Large molecular weights (>10,000 amu), complex structures unique to individual.
Proteins, polysaccharides, glycoproteins, glycolipids.
Enable body to distinguish "self" from foreign molecules.
Epitopes (antigenic determinants): Certain regions of an antigen molecule that stimulate immune responses; binding site for antibodies/lymphocyte receptors.
Haptens: Too small to be antigenic themselves. Can trigger response by combining with a host macromolecule. Subsequently, haptens alone may trigger response (cosmetics, detergents, poison ivy, animal dander, penicillin).
Lymphocytes (Major Cells of the Immune System):
Lymphocytes, Macrophages, Dendritic cells.
Especially concentrated in strategic places (lymphatic organs, skin, mucous membranes).
Three categories: Natural killer (NK) cells, T lymphocytes (T cells), B lymphocytes (B cells).
T Lymphocytes (T Cells):
Born in bone marrow, educated in thymus, deployed for immune function.
Within the thymus: Reticular epithelial (RE) cells secrete chemicals stimulating T cells to develop surface antigen receptors (become immunocompetent). RE cells test T cells by presenting self-antigens. T cells fail by being unable to recognize RE cells or reacting to self-antigen. Failing T cells eliminated by negative selection (clonal deletion - die, or anergy - unresponsive). Negative selection ensures self-tolerance. Surviving T cells undergo positive selection (multiply, form clones programmed to respond to specific antigen). Naive lymphocyte pool (immunocompetent, not yet encountered foreign antigens). Deployment (leave thymus, colonize lymphatic tissues everywhere).
Four classes:
- Cytotoxic T (TC) cells: Killer T cells (T8, CD8+). "Effectors" of cellular immunity, attack enemy cells.
- Helper T (TH) cells: (T4, CD4+). Help promote TC cell and B cell action, nonspecific resistance. Central role in coordinating immunity.
- Regulatory T (TR) cells: (T-regs, CD4+). Inhibit multiplication/cytokine secretion by other T cells; limit immune response.
- Memory T (TM) cells: Descend from TC cells; responsible for memory in cellular immunity.
B Lymphocytes (B Cells):
Develop in bone marrow. Fetal stem cells remain in bone marrow, differentiate into B cells.
B cells reacting to self-antigens undergo anergy or clonal deletion (same as T cell selection). Self-tolerant B cells synthesize antigen surface receptors, divide rapidly, produce immunocompetent clones.
Leave bone marrow and colonize secondary lymphatic tissues/organs as T cells.
Antigen-Presenting Cells (APCs):
T cells cannot recognize antigens on their own. APCs are required. (Dendritic cells, macrophages, reticular cells, B cells function as APCs).
Function depends on major histocompatibility (MHC) complex proteins. Act as cell "identification tags." Structurally unique for each individual (except twins).
Antigen processing: APC encounters antigen, internalizes by endocytosis, digests into fragments (epitopes), displays relevant fragments (epitopes) in grooves of MHC protein.
Antigen presenting: Wandering T cells inspect APCs for displayed antigens. If self-antigen displayed, T cell disregards. If nonself-antigen displayed, T cell initiates immune attack. APCs alert immune system. Key to defense is mobilizing immune cells. Requires chemical messengers to coordinate activities - interleukins (cytokines).
- MHC-I proteins: Constantly produced by nucleated cells, inserted on plasma membrane. Present self-antigens (ignored by T cells) or viral proteins/cancer antigens (elicit T cell response). TC cells respond only to MHC-I + foreign antigen; destroy presenting cell.
- MHC-II proteins: Occur only on APCs. Display only foreign antigens from extracellular environment. TH cells respond only to MHC-II + foreign antigen; initiate immune response coordination.
Comparison of Cellular and Humoral Immunity: (See Table 21.5)
VIII. Cellular Immunity (In Detail)
Three Stages (The Three Rs): Recognition, Attack, Memory. (Applies to both Cellular and Humoral Immunity).
Recognize, React, Remember.
Recognition:
Antigen presentation by APCs to T cells in lymph nodes.
T cell activation:
Begins when TC or TH cell binds to MHCP displaying matching epitope (Signal 1).
T cell must also bind to another APC protein (Signal 2 - costimulation).
Costimulation ensures attack is against foreign antigen, prevents autoimmunity.
Successful costimulation triggers clonal selection.
Activated T cell undergoes repeated mitosis (gives rise to clone of identical T cells).
Some become effector cells (carry out attack).
Others become memory T cells.
Attack (Cellular Immunity):
Helper T (TH) cells and Cytotoxic T (TC) cells play different roles.
TH cells play central role in coordinating both cellular and humoral immunity.
When TH cell recognizes Ag-MHCP complex on APC, secretes interleukins (exert 3 effects): Attract neutrophils/NK cells, Attract/activate macrophages, Stimulate T and B cell mitosis/maturation.
Cytotoxic T (TC) cells are the only T cells that directly attack other cells.
When TC cell recognizes complex of antigen and MHC-I protein on diseased/foreign cell, it "docks" on that cell.
After docking, TC cells deliver a lethal hit of chemicals:
- Perforin and granzymes (kill cells like NK cells).
- Interferons (inhibit viral replication, recruit/activate macrophages).
- Tumor necrosis factor (TNF) (aids macrophage activation, kills cancer cells).
TC cells then search for another enemy cell (serial killing).
Memory (Cellular Immunity):
Immune memory follows primary response in cellular immunity.
Following clonal selection, some TC and TH cells become memory cells.
Long-lived, more numerous than naive T cells, require fewer steps to be activated. Respond more rapidly.
T cell recall response: Upon re-exposure to same pathogen, memory cells launch quick attack so no noticeable illness occurs. The person is immune.
IX. Humoral Immunity (In Detail)
More indirect method of defense than cellular immunity.
B lymphocytes produce antibodies that bind to antigens and tag them for destruction by other means.
Works in three stages: Recognition, Attack, Memory.
Recognition (Humoral Immunity):
Immunocompetent B cell has thousands of surface receptors for one antigen.
Activation begins when antigen binds to several receptors (cross-linking); antigen taken into cell by receptor-mediated endocytosis. (Small molecules not antigenic unless cross-link).
B cell processes (digests) antigen into epitopes. Links some epitopes to its MHC-II proteins. Displays these on cell surface.
Usually B cell response requires help from a helper T cell binding to the Ag–MHCP complex on the B cell.
Bound TH cell secretes interleukins activating the B cell.
Triggers clonal selection: Activated B cell mitosis gives rise to clone of identical B cells.
Most differentiate into plasma cells (secrete antibodies at high rate, have abundance of rough ER).
First exposure: IgM antibodies first, then IgG. Later exposures: IgG primarily. Antibodies travel through body fluids.
Some become memory B cells.
Attack (Antibody Structure):
Immunoglobulin (Ig) - an antibody. Defensive gamma globulin in blood plasma, tissue fluids, secretions.
Antibody monomer (basic structural unit): Composed of 4 polypeptide chains linked by disulfide bonds (2 heavy, 2 light). Heavy chains ~400 aa, light chains ~half. Hinge region allows bending.
Variable (V) region: Tips of arms, unique amino acid sequence; gives antibody uniqueness.
Antigen-binding site: Formed from V regions of heavy/light chains on each arm; attaches to epitope of antigen. (Each monomer has 2 identical sites).
Constant (C) region: Rest of chain, same sequence for given class in one person; determines mechanism of action.
Attack (Antibody Classes and Diversity):
Antibody classes named for C region structure:
- IgA: Monomer (plasma), dimer (secretions). Mucus, saliva, tears, milk, secretions. Prevents pathogen adherence/penetration of epithelia. Passive immunity to newborns.
- IgD: Monomer. B cell transmembrane antigen receptor. Thought to function in B cell activation by antigens.
- IgE: Monomer. Binds to basophils/mast cells. Stimulates histamine/inflammatory chemical release. Attracts eosinophils to parasites. Produces immediate hypersensitivity reactions (allergy).
- IgG: Monomer. 80% of circulating antibodies. Crosses placenta. Secreted in secondary immune response. Complement fixation.
- IgM: Pentamer (plasma/lymph). Secreted in primary immune response. Agglutination, complement fixation.
Human immune system capable of ~1 trillion different antibodies, from ~20,000 genes. Achieved by:
- Somatic recombination: DNA segments shuffled to form new combinations of base sequences for antibody genes.
- Somatic hypermutation: B cells in lymph nodules rapidly mutate creating new sequences in antibody genes (affinity maturation).
Attack (Antibody Mechanisms):
Antibodies have four mechanisms of attack against antigens:
- Neutralization: Antibodies mask pathogenic region of antigen.
- Complement fixation: IgM or IgG bind antigen, change shape, initiate complement binding cascade (inflammation, phagocytosis, immune clearance, cytolysis). Primary defense against foreign cells, mismatched RBCs.
- Agglutination: Antibody has 2-10 binding sites; binds multiple enemy cells, immobilizing them from spreading.
- Precipitation: Antibody binds antigen molecules (not cells); creates Ag-Ab complex that precipitates, allowing removal by immune clearance or phagocytosis by eosinophils.
Memory (Humoral Immunity):
Primary immune response: Immune reaction by first exposure. Appearance of protective antibodies delayed (3-6 days) while naive B cells multiply/differentiate. Antibody titer (level) rises. IgM appears first (peaks ~10 days), then declines. IgG rises as IgM declines, drops to low level within month.
Primary response leaves immune memory of antigen.
During clonal selection, some cells become memory B cells.
Found mainly in germinal centers of lymph nodes.
Secondary (anamnestic) response: If reexposed to same antigen. Plasma cells form within hours. IgG titer rises sharply, peaks in few days (much higher). Response so rapid, antigen little chance to exert effect (no illness results). Low IgM also secreted, quickly decline. IgG remain elevated for weeks/years (conferring long-lasting protection).
Memory may not last as long as cellular immunity for some pathogens.
Comparison of Cellular and Humoral Immunity: (See Table 21.5)
X. Immune System Disorders
Immune response may be: Too vigorous, Too weak, Misdirected against wrong targets.
Hypersensitivity:
Excessive immune reaction against antigens most people tolerate. Includes:
- Alloimmunity: Reaction to transplanted tissue from another person.
- Autoimmunity: Abnormal reactions to one’s own tissues.
- Allergies: Reactions to environmental antigens (allergens - dust, pollen, venom, foods, drugs, etc.).
Four kinds of hypersensitivity: Based on immune agents (antibodies/T cells) and method/speed of attack.
- Type I acute (immediate): Very rapid response (seconds). Antibody-mediated (IgE). Usually subsides 30 min, can be fatal. Allergens bind IgE on basophils/mast cells -> secrete histamine/vasoactive chemicals. Triggers glandular secretion, vasodilation, increased permeability, smooth muscle spasms. Clinical signs: local edema, mucus secretion/congestion, watery eyes/runny nose, hives, cramps/diarrhea/vomiting. Examples: food allergies, allergic asthma.
- Type II and Type III subacute: Slower onset (1-3 hours), last longer (10-15 hours). Antibody-mediated (IgG/IgM).
- Type II (antibody-dependent cytotoxic): IgG/IgM attack antigens bound to cell surfaces. Reaction leads to complement activation (lysis) or opsonization (phagocytosis). Damages platelets, erythrocytes, other cells. Examples: blood transfusion reaction, pemphigus vulgaris, some drug reactions.
- Type III (immune complex): IgG/IgM form Ag-Ab complexes in plasma. Precipitate beneath endothelium/in tissues. Activate complement, trigger intense inflammation. Examples: acute glomerulonephritis, systemic lupus erythematosus.
- Type IV (delayed cell-mediated): Cell-mediated reaction (T cells). Signs appear 12-72 hours after exposure. Begins when APCs display antigens to helper T cells. T cells secrete interferon/cytokines activating cytotoxic T cells and macrophages. Result is mixture of nonspecific/immune responses. Examples: haptens in cosmetics/poison ivy, graft rejection, TB skin test, type 1 diabetes mellitus (beta cell destruction).
Anaphylaxis:
Immediate, severe Type I reaction. Local anaphylaxis relieved with antihistamines.
Anaphylactic shock: Severe, widespread acute hypersensitivity. Allergen into bloodstream/rapid absorption. Bronchoconstriction/dyspnea, widespread vasodilation/circulatory shock, sometimes death. Antihistamines inadequate. Epinephrine relieves symptoms (dilates bronchioles, increases cardiac output/BP). Fluid therapy/respiratory support sometimes required.
Asthma:
Most common chronic illness in children.
- Allergic (extrinsic): Triggered by inhaled allergens. IgE-mediated, mast cells release inflammatory chemicals, intense airway inflammation. Severe coughing, wheezing, suffocation. Second crisis 6-8 hours later. Eosinophils paralyze cilia. Damage epithelium, scarring. Bronchioles edematous, plugged with mucus.
- Nonallergic (intrinsic): Triggered by infections, drugs, pollutants, cold air, exercise, emotions. Effects similar to allergic asthma.
Treatment: β-adrenergic stimulants (dilate airway), inhaled corticosteroids (minimize inflammation/damage).
Autoimmune Diseases:
Failures of self-tolerance. Immune system does not correctly distinguish self from foreign, attacks own tissues (produces autoantibodies/self-reactive T cells).
Reasons for failure:
- Cross-reactivity: Antibodies against foreign antigens react to similar self-antigens (e.g., Rheumatic fever - strep antibodies react with heart valves).
- Abnormal exposure of self-antigens in the blood (e.g., sperm antigens normally isolated by blood-testes barrier).
- Changes in structure of self-antigens (viruses/drugs change structure, perceived as foreign).
- Self-reactive T cells: Not all eliminated in thymus, normally kept in check by regulatory T cells.
Immunodeficiency Diseases:
Immune system fails to react vigorously enough.
- Severe combined immunodeficiency disease (SCID): Hereditary lack of T and B cells. Vulnerability to opportunistic infection. Must live in protective enclosures.
Acquired immunodeficiency syndrome (AIDS):
Nonhereditary, contracted after birth.
Group of conditions severely depressing immune response.
Caused by infection with human immunodeficiency virus (HIV) (retrovirus).
Invades helper T cells, macrophages, dendritic cells ("tricking" internalization via receptor-mediated endocytosis).
HIV uses reverse transcriptase (viral RNA -> DNA). New DNA inserted into host DNA (dormant months/years). Activated host cell produces viral RNA, capsid/matrix proteins. Coated with host plasma membrane bits, adhere to new host cells, repeat.
By destroying TH cells, HIV strikes at central coordinating agent of nonspecific defense, humoral, and cellular immunity.
Incubation period ranges from months to 12+ years.
Signs and symptoms: Early flu-like. Progresses to night sweats, fatigue, weight loss, lymphadenitis. Normal TH count 600-1200 cells/µL; AIDS <200 cells/µL.
Susceptible to opportunistic infections (Toxoplasma, Pneumocystis, herpes, CMV, TB).
Candida (thrush - white patches). Kaposi sarcoma (cancer from endothelial cells, purple lesions).
HIV is transmitted through blood, semen, vaginal secretions, breast milk, across placenta. Most common means: sexual intercourse, contaminated blood products/needles. Not transmitted by casual contact. Undamaged latex condom effective barrier.
Strategies to combat AIDS: Prevent binding to CD4. Disrupt reverse transcriptase/assembly (medications). None eliminate HIV, all have serious side effects. HIV develops drug resistance (medicines used in combination - ART). AZT (first anti-HIV, inhibits reverse transcriptase). Protease inhibitors (inhibit enzymes HIV needs). >24 anti-HIV drugs on market.
Underpinning knowledge/ theory for Lymphatic System:
(This is covered within the sections above, extracting relevant concepts from the provided notes.)
- Detailed diagrammatic description of the circulatory and lymphatic system.
- Components and functions of the lymphatic system.
- Structure and organization of lymphatic vessels, trunks, and ducts.
- Flow of lymph.
- Types and functions of lymphatic cells.
- Structure and function of lymphatic tissues and organs (lymph nodes, thymus, spleen, tonsils, red bone marrow).
- Overview of nonspecific resistance (innate immunity).
- Overview of adaptive immunity (specific immunity).
- Types of immune system disorders.
Revision Questions for Lymphatic System:
1. List the three main functions of the lymphatic system.
2. How does the lymphatic system contribute to fluid recovery and prevent edema?
3. What are lymphatic capillaries, and how do they differ from blood capillaries in structure?
4. Name the two main collecting ducts of the lymphatic system and state where each empties into the blood circulation.
5. Describe two mechanisms that help the flow of lymph.
6. Name three major types of lymphatic cells and briefly state the primary function of each.
7. What are lymph nodes, and what are their two main functions?
8. Name two primary lymphatic organs and their significance.
9. Name three secondary lymphatic organs.
10. Briefly explain the difference between nonspecific resistance and adaptive immunity.
11. Define autoimmunity and give one example of an autoimmune disease.
12. What causes AIDS, and how does it affect the immune system?







![[Full anterior and posterior views of the human skeleton with major bones and key joints labeled.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Full-anterior-and-posterior-views-of-the-human-skeleton-with-major-bones-and-key-joints-labeled.jpg)
![[Diagram showing the human skeleton with the axial skeleton highlighted or color-coded differently from the appendicular skeleton.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/axial-skeleton-highlighted-or-color-coded-differently-from-the-appendicular-skeleton.jpg)
![[Cross-section diagram of a bone showing the outer layer of compact bone surrounding the inner network of spongy bone. Maybe show a flat bone cross-section (diploe) as well.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/ClassificationofBonesontheBasisofShape-e1751439762811.jpg)
![[Detailed, labeled diagram of a long bone showing all key anatomical features: diaphysis, epiphysis, metaphysis, epiphyseal line/plate, articular cartilage, periosteum, endosteum, medullary cavity, compact bone, spongy bone.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/603_Anatomy_of_Long_Bone-1.jpg)
![[Cross-section diagram of a bone showing the outer layer of compact bone surrounding the inner network of spongy bone. Maybe show a flat bone cross-section (diploe) as well.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Cross-section-diagram-of-a-bone-showing-the-outer-layer-of-compact-bone.jpg)
![[Diagram showing the different types of bone cells (osteogenic cell, osteoblast, osteocyte, osteoclast) and their location/role in bone tissue.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/types-of-bone-cells-osteogenic-cell-osteoblast-osteocyte-osteoclast.jpg)
![[Diagram illustrating the process of endochondral ossification, showing the hyaline cartilage model being progressively replaced by bone tissue from primary and secondary ossification centers.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/endochondral-ossification.jpg)
![[Diagram illustrating both longitudinal growth at the epiphyseal plate and appositional growth (growth in width) occurring simultaneously in a long bone.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/longitudinal-growth-at-the-epiphyseal-plate-and-appositional-growth-1.jpg)
![[Diagram or table illustrating common types of fractures (e.g., transverse, oblique, spiral, comminuted, compression, greenstick, open/closed).]](https://nursesrevisionuganda.com/wp-content/uploads/2023/05/ezgif.com-webp-to-jpg-11-1.jpg)
![[Diagram illustrating the four stages of fracture healing: 1. Hematoma formation, 2. Fibrocartilaginous callus formation, 3. Bony callus formation, 4. Bone remodeling.]](https://nursesrevisionuganda.com/wp-content/uploads/2023/03/Illustration-of-stages-in-bone-healing-after-a-fracture.jpg)
![[Diagram illustrating the three main structural classifications of joints: Fibrous joint (suture), Cartilaginous joint (symphysis or synchondrosis), and Synovial joint. Clearly label the components of a synovial joint (articular cartilage, joint capsule, synovial membrane, synovial fluid, joint cavity, ligaments).]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Classification-of-Joints.png)
![[Diagrams illustrating the six different types of synovial joints (Plane, Hinge, Pivot, Condyloid, Saddle, Ball-and-Socket) with a small illustration of the bone shapes and arrows indicating the types of movement allowed for each, and examples of where they are found in the body.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/cartilagenous-joints.jpg)
![[Diagram illustrating the three main structural classifications of joints: Fibrous joint (suture), Cartilaginous joint (symphysis or synchondrosis), and Synovial joint. Clearly label the components of a synovial joint (articular cartilage, joint capsule, synovial membrane, synovial fluid, joint cavity, ligaments).]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/types-of-synovial-joints-1.jpg)
![[Images illustrating common joint disorders: Osteoarthritis (showing cartilage erosion), Rheumatoid Arthritis (showing joint deformity), Gout (inflamed joint), diagram of a sprained ankle, diagram of a joint dislocation.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/common-joint-disorders.webp)
![[An overview diagram showing the major muscles of the human body, anterior and posterior views. Label main muscle groups.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/1105_Anterior_and_Posterior_Views_of_Muscles2-1024x631-1.jpg)
![[Microscopic view of skeletal muscle tissue, showing its long, cylindrical fibers, striations, and multiple nuclei located peripherally.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/microscopic-skeletal-muscle-e1751345586323.webp) Smooth Muscle:
Smooth Muscle:
![[Microscopic view of smooth muscle tissue, highlighting its spindle shape, single central nucleus, and lack of striations.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Smooth-musclet-tissue-1-1-e1751389483746.png) Cardiac Muscle:
Cardiac Muscle:
![[Microscopic view of cardiac muscle tissue, showing striations, branching cells, central nuclei, and prominent intercalated discs connecting the cells.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Microscopic-view-of-cardiac-muscle-tissue.jpg)
![[Diagram showing the hierarchical structure of a skeletal muscle, starting from the entire muscle organ, down to a fascicle, a single muscle fiber (cell), and finally a myofibril, illustrating the connective tissue coverings at each level.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Diagram-showing-the-hierarchical-structure-of-a-skeletal-muscle.jpg)
![[Detailed diagram illustrating the structure of thick (myosin) and thin (actin, tropomyosin, troponin, elastic/titin) filaments and showing their arrangement within a sarcomere.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Structure-of-Sarcomere.webp)
![[Diagram of a motor unit, showing a motor neuron originating from the spinal cord, its axon branching out, and each axon branch forming a neuromuscular junction with a different skeletal muscle fiber within the muscle.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Diagram-of-a-motor-unit.jpg)
![[Diagram of a motor unit, showing a motor neuron originating from the spinal cord, its axon branching out, and each axon branch forming a neuromuscular junction with a different skeletal muscle fiber within the muscle.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/nueromuscular-junction.png)
![[Detailed diagram of the neuromuscular junction, clearly labeling the presynaptic axon terminal, synaptic vesicles containing ACh, the synaptic cleft, the motor end-plate with junctional folds, and acetylcholine receptors on the muscle fiber membrane.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Detailed-diagram-of-the-neuromuscular-junction-clearly-labeling-the-presynaptic-axon-terminal.jpg)
![[Series of detailed diagrams illustrating the step-by-step process of neuromuscular transmission at the NMJ, from arrival of action potential to ACh release, binding, EPP generation, and initiation of muscle action potential.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Step-by-step-process-of-neuromuscular-transmission-at-the-NMJ-1.jpg)
![[Diagram clearly illustrating the difference between a relaxed sarcomere and a contracted sarcomere, showing how the thin filaments move inwards and the Z-discs get closer while the thick and thin filaments retain their original length.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Diagram-clearly-illustrating-the-difference-between-a-relaxed-sarcomere-and-a-contracted-sarcomere.jpg)
![[Series of detailed diagrams illustrating the steps of the sliding filament theory and cross-bridge cycling: 1. Calcium binding to troponin/tropomyosin movement, 2. Cross-bridge formation, 3. Power stroke, 4. ATP binding and detachment, 5. ATP hydrolysis and re-cocking of myosin head.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/steps-of-the-sliding-filament-theory-and-cross-bridge-cycling.jpg)
![[Flowchart or diagram comparing the three main metabolic pathways for ATP production in muscle cells: Creatine Phosphate System (Direct Phosphorylation), Anaerobic Glycolysis, and Aerobic Respiration. Show inputs, outputs, speed, duration supported, and location.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/Flowchart-or-diagram-comparing-the-three-main-metabolic-pathways-for-ATP-production-in-muscle-cells-1.jpg)
![[Diagram clearly illustrating the concepts of muscle origin and insertion using a specific muscle (e.g., Biceps Brachii or Gastrocnemius) and showing how contraction pulls the insertion towards the origin.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/concepts-of-muscle-origin-and-insertion-using-a-specific-muscle.jpg)
![[Diagram illustrating the roles of different muscles (agonist, antagonist, synergist, fixator) during a specific movement, such as elbow flexion or forearm pronation/supination.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/roles-of-different-muscles-agonist-antagonist-synergist-fixator.jpg)
![[Diagram illustrating isotonic (concentric and eccentric) and isometric contractions with simple examples like lifting and holding a weight.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/isotonic-concentric-and-eccentric-and-isometric-contractions.jpg)
![[Illustrations showing various common body movements (flexion, extension, abduction, adduction, rotation, circumduction) at different joints.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/common-body-movements-flexion-extension-abduction.webp)
![[Illustrations showing movements of the ankle and foot (dorsiflexion, plantar flexion, inversion, eversion) and movements of the forearm/wrist (supination, pronation, opposition of the thumb).]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/common-body-movements-flexion-extension-abduction-adduction-rotation-circumduction-at-different-joints.jpg)
![[Diagrams illustrating the concept of muscle origin and insertion, and showing how muscles act on joints as levers (maybe show a simple example like the elbow joint).]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/concept-of-muscle-origin-and-insertion-and-showing-how-muscles-act-on-joints-as-levers-1.png)
![[Images illustrating common muscular disorders: muscle strain, tendinitis, muscular dystrophy (showing muscle wasting), myasthenia gravis (e.g., drooping eyelid), diagram of compartment syndrome, image of an inguinal hernia.]](https://nursesrevisionuganda.com/wp-content/uploads/2025/07/common-muscular-disorders.jpg)