Theories of Growth and Development
Theories of Growth and Development
Growth involves physical changes in height and weight and appearance of the body, while development refers to a change in functional ability, such as cognitive, motor, and psychological aspects of the client.
Growth and development start from the time of conception and progress until a person dies. Growth and development theories provide a framework to understand this wide array of changes, and they help healthcare providers plan individualized care for clients based on their stage of development, and to provide anticipatory guidance for parents and caregivers.
Major growth and development theories include biophysical developmental theory by Gesell, psychosocial development theory by Erikson; cognitive development theory by Piaget; moral development theory by Kohlberg; and finally, the psychoanalytic development theory by Freud.
Theories of Growth and Development
Theories associated with growth and development include:
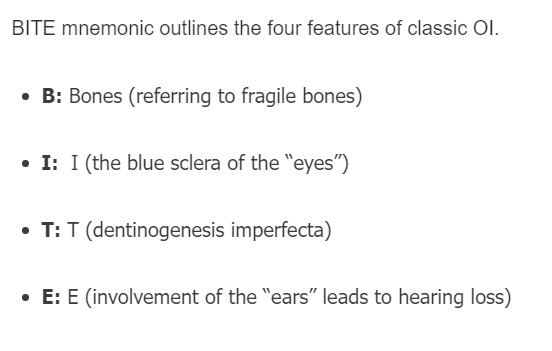
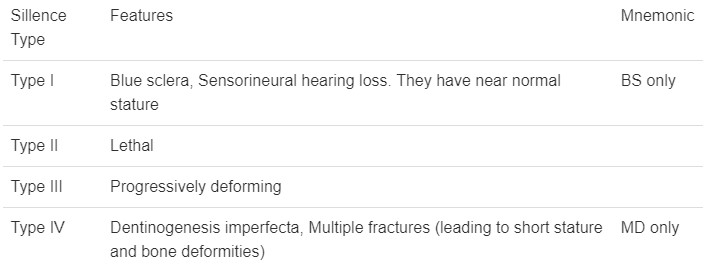
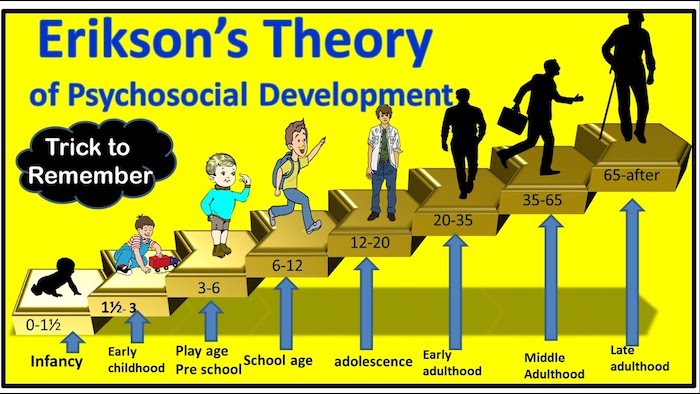
Erikson Theory of Development
The theory describes the major developmental issues or problems Erikson identified for each of the stages of development.
The major psychosocial and intellectual issues involved:
- Infancy: Basic trust versus mistrust
- Central task is to establish a sense of basic trust in predominance to mistrust.
- Infants who find that their needs for food and comfort are constantly and effectively met, learn that the world is a safe and predictable place and that they can trust others.
- In contrast, a sense of mistrust may predominate in infants who do not receive constant care and those who experience long spells of discomfort.
- Mistrust creates formation barriers to interpersonal bond.
- Mistrust interferes with the development of confidence, security, and assertiveness.
2. Toddlerhood: Autonomy versus shame and doubt
- A child must establish a sense of autonomy in this phase rather than shame & doubt.
- Autonomy – a kind of self-trust, a growing awareness that their behavior is under their control. This is the desired, and outcomes are usually like “I can do it”.
- Shame “I can do it but that is not nice”.
- Doubt “I cannot do it”.
- It is hazardous when self-mistrust is carried on from infancy onwards.
3. Pre-school years: initiative versus guilt
- Central task is to develop a sense of initiative in predominance to the sense of guilt.
- Explore what they can create and do with the motor, language, interpersonal and social world.
- Behavior is characterized by intrusiveness manifested in endless questions, noise, physical and intellectual exploration.
- Guilt is a major developmental hazard because what they try to do is difficult or unacceptable to people they wish to please.
4. The school age period: Industry versus inferiority
- Central task is a sense of industry in predominance to a sense of inferiority.
- Industry – the child uses physical, cognitive (intellectual), and social skills and turns his attention to learning what he must know in preparation for success in the adult world.
- Learns self-worth as workers and producers.
- Inferiority – Negative self-concept comes when children have difficulty in school, interpersonal relationships, or other expectations. They get discouraged and consider themselves inadequate.
5. Adolescence: Identity versus role confusion
- Central task is developing a sense of identity with the undesirable alternative being role confusion.
- Attachment of identity is a process of young people coming to feel that they are consistent with others, in terms of views (own views in relation to other people’s views).
- The major hazard is role confusion. Arises from rapid changes in the experience of self and from sometimes overwhelming numbers of possible ways to behave and roles to select.

2. Freud: Stages of Psychosexual Development
- Freud’s theory revolves around sexual pleasure and has five stages: oral, anal, phallic, latency, and genital.
Oral Stage: This starts from birth to until 1 year. During this stage, the primary source of pleasure and gratification is through the mouth, such as sucking and feeding. Freud believed that unresolved conflicts during this stage, such as weaning issues or oral fixation, could lead to oral-related behaviors in adulthood, such as overeating, smoking, or excessive talking.
Anal Stage: The anal stage occurs between the ages of 1 and 3 years. This stage focuses on the child’s pleasure and control over their bowel movements. Freud believed that conflicts related to toilet training during this stage could lead to fixation, resulting in anal-retentive behaviors (being overly neat, organized, and controlling) or anal-expulsive behaviors (being messy, disorganized, and rebellious).
Phallic Stage: The phallic stage takes place between the ages of 3 and 6. During this stage, children develop a strong attachment to their opposite-sex parent (Oedipus complex for boys and Electra complex for girls). Freud believed that unresolved conflicts during this stage could lead to sexual and gender identity issues or difficulties with relationships in adulthood.
Latent Stage: The latent stage occurs from around 6 years old until the onset of puberty. During this stage, sexual desires and impulses are repressed, and the focus of the child’s energy is on developing social and intellectual skills. Freud believed that this stage is relatively calm and that there are no significant conflicts or fixations.
Genital Stage: The genital stage begins at the onset of puberty and continues into adulthood. This stage marks the reawakening of sexual desires and the development of mature sexual relationships. Freud believed that successful resolution of previous stages’ conflicts leads to healthy sexual development and the ability to form intimate relationships.
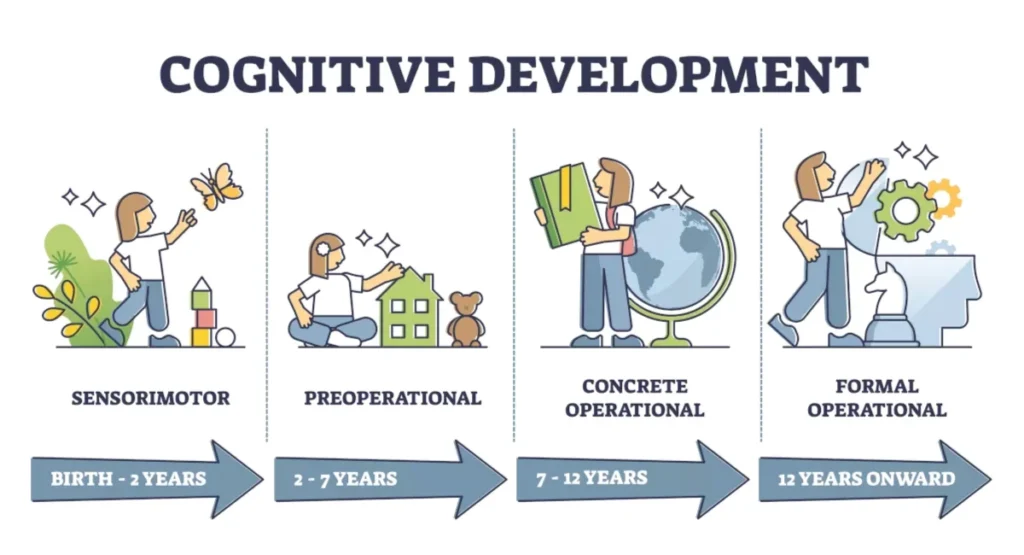
3. Piaget: Periods of Cognitive Development
- Piaget’s theory focuses on cognitive development and stages, including sensorimotor, preoperational thought, concrete operation, and formal operation.
Sensorimotor Stage: The sensorimotor stage occurs from birth to around 2 years of age. During this stage, infants primarily learn about the world through their senses and motor actions. They develop object permanence, the understanding that objects continue to exist even when they are out of sight. Infants also engage in trial-and-error experimentation and begin to demonstrate intentional actions.
Preoperational Stage: The preoperational stage typically occurs between the ages of 2 and 7. During this stage, children become more adept at using symbols, such as words and images, to represent objects and events. They engage in pretend play and develop language skills. However, children in this stage often struggle with logical reasoning and exhibit egocentrism, where they have difficulty understanding other people’s perspectives.
Concrete Operational Stage: The concrete operational stage takes place between the ages of 7 and 11. During this stage, children become capable of concrete, logical thinking. They can understand conservation, the idea that certain properties of objects remain the same despite changes in appearance. Children also develop the ability to classify objects into different categories and engage in more systematic problem-solving.
Formal Operational Stage: The formal operational stage begins around the age of 11 and extends into adulthood. During this stage, individuals develop abstract thinking and can reason hypothetically. They can engage in deductive reasoning, logical thinking, and hypothetical-deductive reasoning. They can also think about multiple possibilities and engage in more complex problem-solving.
Piaget believed that individuals progress through these stages in a fixed sequence, with each stage building upon the previous one. He proposed that cognitive development occurs through a process of assimilation and accommodation, where individuals assimilate new information into their existing mental structures (schemas) and accommodate their schemas to fit new information.
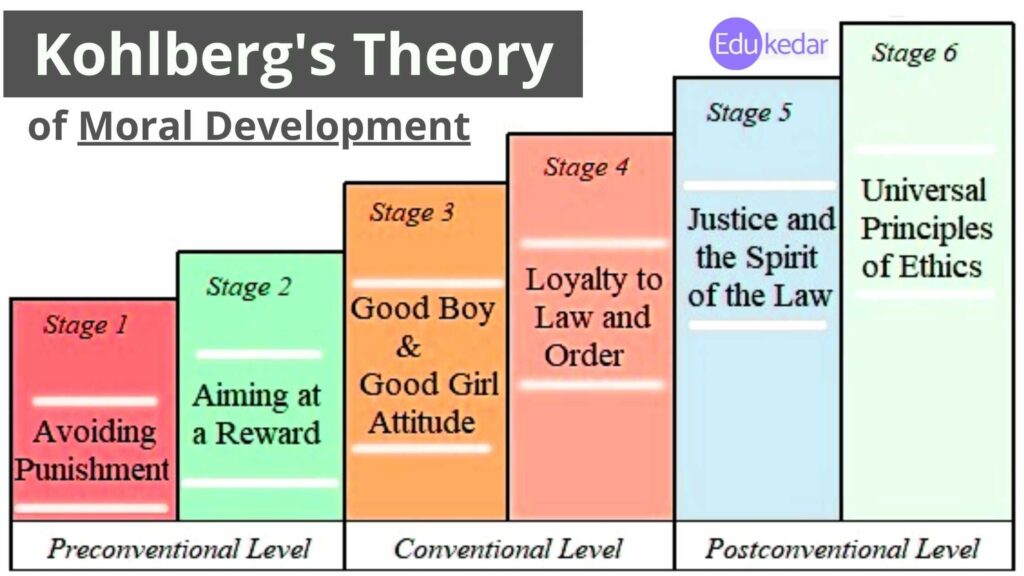
4. Kohlberg: Theories of Moral Development
- Kohlberg’s theory explores moral development through stages of moral reasoning.
Level 1: Preconventional Morality
Stage 1: Obedience and Punishment Orientation: At this stage, individuals focus on avoiding punishment and obeying authority figures. They make moral decisions based on the fear of being punished and seek to satisfy their own needs.
Stage 2: Individualism and Exchange: In this stage, individuals start to consider their own interests and begin to understand that others have their own needs and desires. Moral decisions are driven by self-interest and the expectation of receiving something in return.
Level 2: Conventional Morality
Stage 3: Interpersonal Relationships: At this stage, individuals value social harmony and seek approval from others. They make moral decisions based on the desire to be seen as a good person and to maintain positive relationships with others.
Stage 4: Maintaining Social Order: In this stage, individuals focus on following rules and maintaining social order. They make moral decisions based on a sense of duty, respect for authority, and the need to uphold societal norms and laws.
Level 3: Postconventional Morality
Stage 5: Social Contract and Individual Rights: At this stage, individuals recognize that different societies may have different moral standards, and they begin to question and evaluate these standards. Moral decisions are based on principles of fairness, justice, and the protection of individual rights.
Stage 6: Universal Principles: In this final stage, individuals develop their own set of moral principles that are based on universal ethical principles, such as justice, equality, and respect for human dignity. Moral decisions are guided by these principles, even if they conflict with societal norms or laws.
Growth Monitoring and Promotion
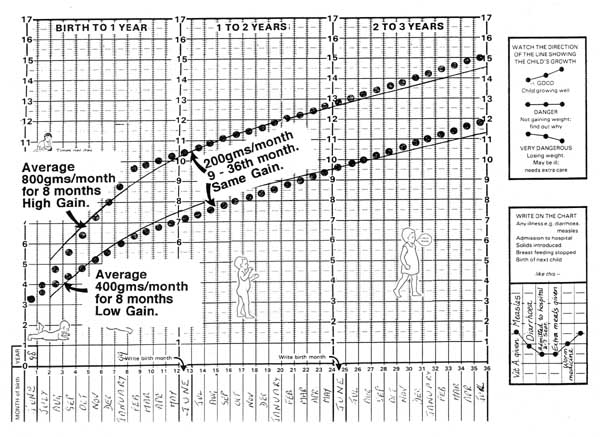
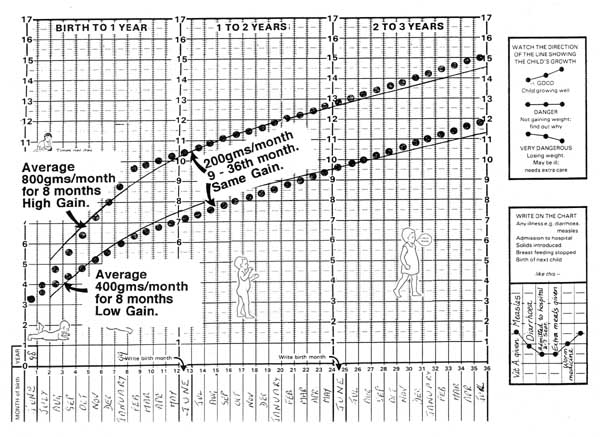
Growth Monitoring
- Growth monitoring involves regularly weighing a child, plotting the weight on a child health card, interpreting the results, and counseling parents or caregivers.
- Monitoring includes height for age, weight for age, head circumference, body mass index (BMI), and skinfold thickness.
- Height for age.
- Weight for age.
- Head circumference.
- Body mass index (BMI).
- Skin fold thickness.
Importance of Growth Monitoring
- Children whose growth is abnormal are easily recognized from the growth chart.
- Helps in the identification of chronic disorders.
- Helps in the attainment of the nutrition status and improvement of nutrition.
- It supports research.
- It helps the parents to get nutritional knowledge and reduce anxiety and be reassured about child’s health.
- Helps to find out if there are influential, psychological, social factors that may affect the growth of the child and address them. E.g. parent neglect or separation, orphans, etc.
- Helps parents determine if children are naturally short stature.
- Helps to prevent illness, malnutrition, and death.
- Helps to evaluate health or nutritional interpretation, e.g. breastfeeding.
- Helps to determine if the child is failing to thrive.
To combat growth problems, we need growth promotion. This includes the following:
- Antenatal care.
- Prevent, detect and treat pregnancy-related complications.
- Provide advice on breastfeeding to the mothers.
- Provide health education on dangers of smoking, alcohol consumption, and drug abuse.
- Health education on good baby care.
- Identify parents who may need extra support in caring for the children, e.g. parents with learning disorders or mental problems.
- Health education on good nutrition.
- Provide preventive treatment – IPT, iron supplements, deworming tablets, etc.
- Monitor the progress of pregnancy.
- Health education on hygiene.
- Encourage the mothers to deliver in the hospital.
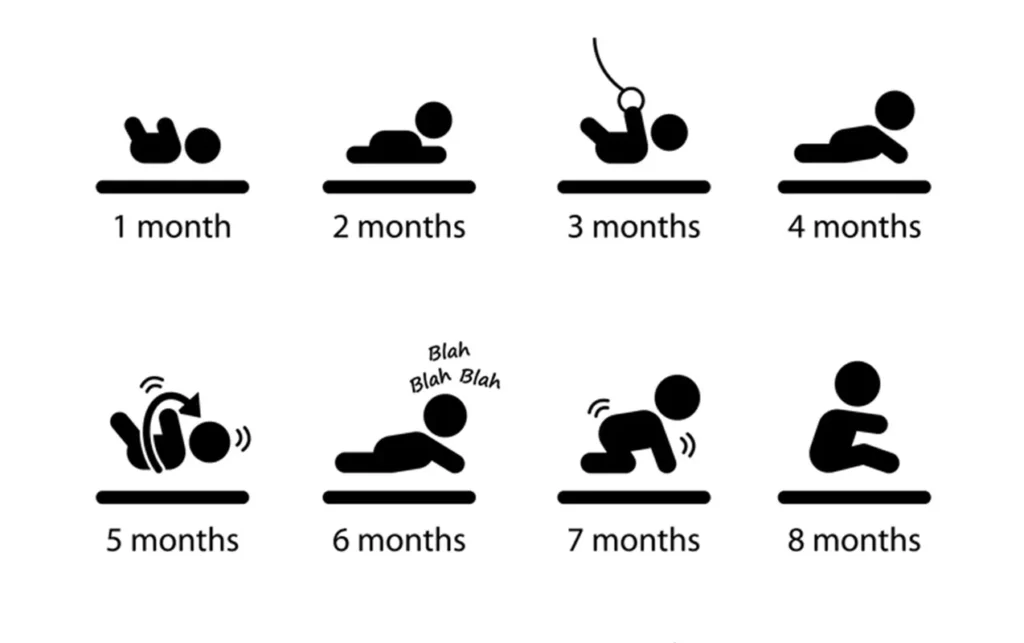
Less than 6 weeks
- Physical/medical examination of the child.
- Immunization, e.g. polio 0, BCG.
- Exclusive breastfeeding.
- Hygiene-cord care.
- Growth monitoring, weighing.
- Early detection of disease, e.g. fever, diarrhea.
At 6 weeks
- Physical examination.
- Immunization.
- Care safety.
- Growth monitoring.
- Proper nutrition.
- Hygiene.
- Early detection of disease.
At 2, 3, 4 months of age
- Immunization.
- At 10 weeks, polio 2, Hib, Hep b 2DPT2.
- At 14 weeks, polio3, Hib, Hep b3, DPT3.
- Check weight.
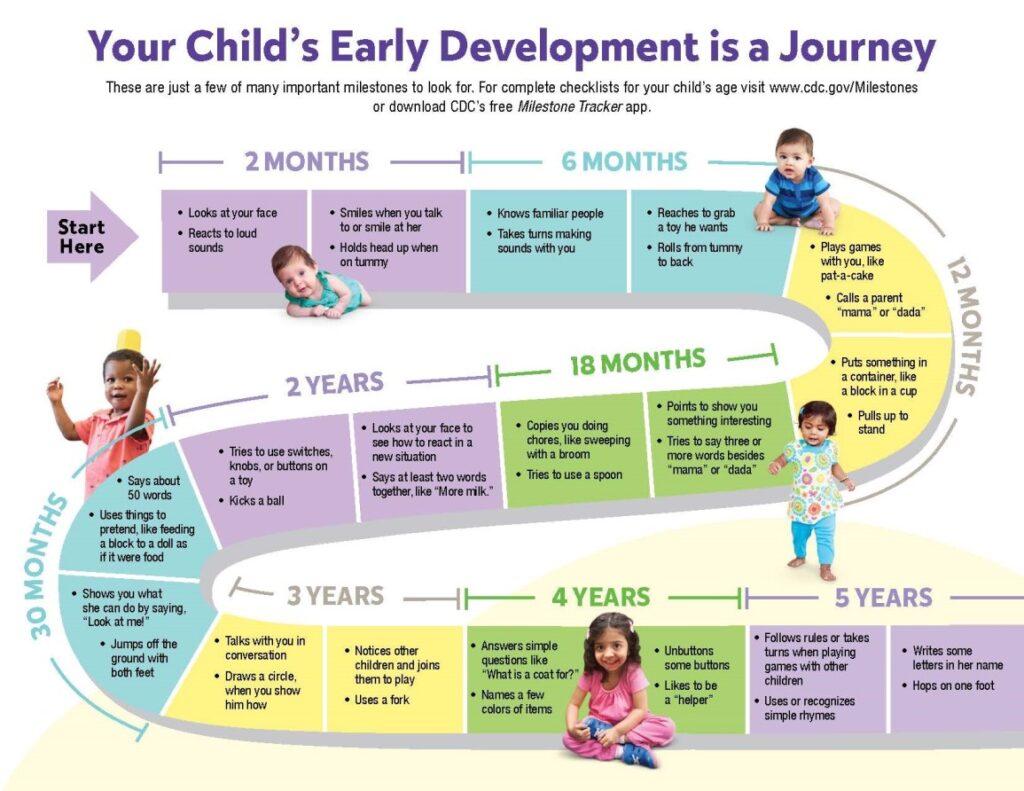
8 months, 2 years, 3 years
- Immunization: At 9 months, measles vaccine.
- Respond to mothers who have concerns about their children’s development.
- Prevent, detect and treat illnesses.
- Monitor growth.
- Hygiene.
- Good nutrition.
At 4-5 years
- A review at school entry provides an opportunity to check that:
- Immunization is up-to-date.
- Children have access to immunization and dental care.
- Appropriate assessment and intervention for any physical, social, emotional, problems.
- Provide children, parents, and school staff with information about specific health issues.
- Check the child’s weight and height.
School entry – 5 years
School nurse checks:
- Weight and height.
- Reviews immunization status.
Child Health Card
The child health card is a clinical tool used to monitor the health of children from birth to 5 years.
It is a clinical tool designed by the Ministry of Health (MoH) Uganda to assist in monitoring the general health of children from birth up to 5 years of age.
Components of the Child Health Card
- Family Information: Includes child demographics, parents’ details, and address.
- Immunization Schedule: Lists the recommended immunizations.
- Interpretation Section: Guides for interpreting growth trends.
- Growth Chart: Tracks weight growth.
- Vitamin A Supplementation: Records doses for both the child and mother.
- Special Care Categories: Flags children with specific needs.
- Remarks and Referrals: Notes for additional comments and referrals.
- Child demographics include: child’s name, birth weight, sex, date of birth, birth order, mother’s occupation, father’s name and occupation, where child lives.
Counseling the mother After Weighing the Child
0-6 Months (Gained Weight)
- Show the mother the growth curve and congratulate her for the child’s weight gain.
- Find out what the mother knows or believes about exclusive breastfeeding.
- Find out if the mother has sickness or problems.
- Find out how the mother is feeding her child and reinforce breastfeeding.
0-6 Months (Did Not Gain Adequate Weight)
- Create rapport.
- Show the mother the growth curve and explain that the baby did not gain weight as expected.
- Find out if the baby is sick or has problems.
- Find out if the baby is fed on other foods.
- Find out if mother’s nutrition is appropriate and adequate.
- Find out if the baby has problems with sucking.
- Find out if the mother has problems with attaching the baby to the breast during breastfeeding.
Ask:
- How many times a day and night does the baby breastfeed?
- Does the baby breastfeed long enough to empty the breast?
- Is the child fed on other liquids or foods?
- Does the mother stay away from the baby any time during the day?
- Information to the mother
- Breastfeed for at least 8-10 times per day.
- Encourage the mother to feed long enough to empty one breast before moving to the other breast.
- Help the mother to know the correct position and attachment of the baby to the breast.
- Encourage exclusive breastfeeding unless there are other reasons.
- Check child’s immunization status.
- Check and give vitamin A.
6-12 Months (Gained Weight)
- Repeat the counseling steps.
- Ask about additional foods besides breast milk.
6-12 Months (Did Not Gain Adequate Weight)
- Show the mother the card and explain that the baby did not gain weight as expected.
- Ask about the child’s health; if sick, refer.
- Find out how the mother is feeding the child and discuss with her the improvements she can make.
- Find out if the mother’s nutrition is appropriate and adequate.
- Praise all good practice.
- Birth weight less than 2.5kg.
- Birth defects.
- Fifth and above child.
- Birth less than 2 years after the last birth.
- Sibling under-nourished.
- Mother or father dead.
- Three or more children dead in the family.
- Twin child.
Theories of Growth and Development Read More »