VISUAL IMPAIRMENT
VISUAL IMPAIRMENT
Visual impairment also known as vision impairment or vision loss , is a decreased ability to see to a degree that causes problems not fixable by usual means, such as glasses.
Visual impairment refers to any kind of vision loss, ranging from partial vision loss to complete blindness.
Visual impairment is often defined as a best corrected visual acuity of worse than either 20/40 or 20/60.
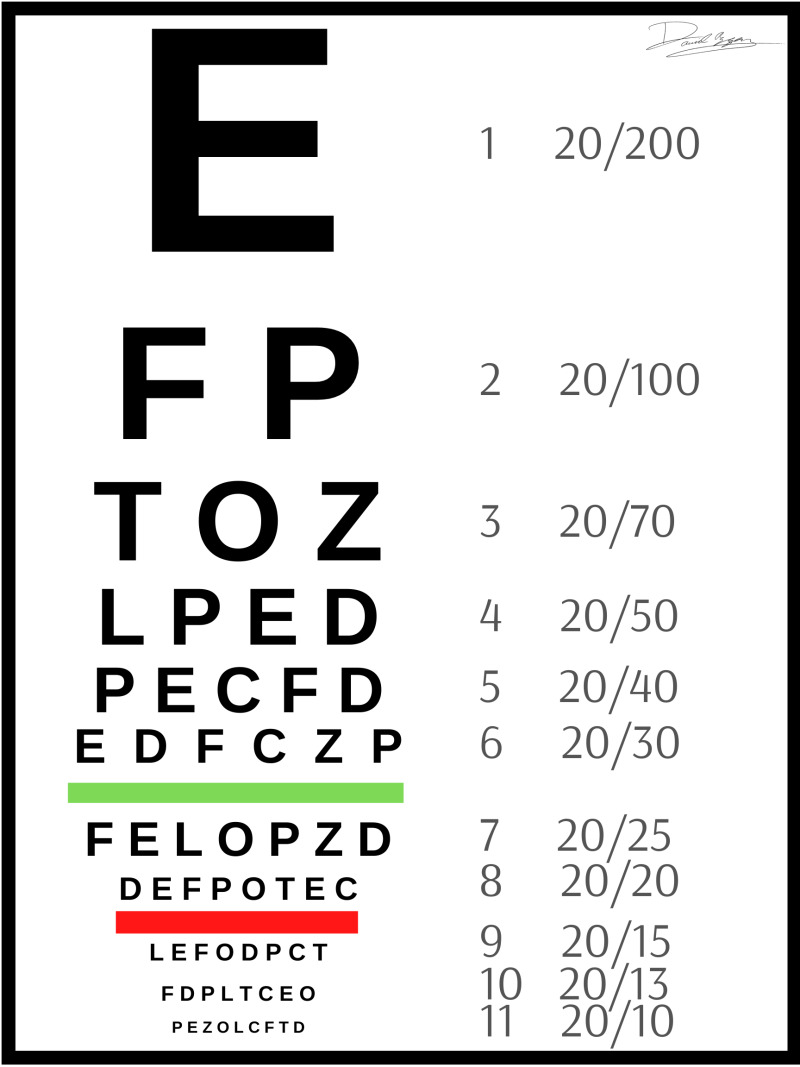
To understand Visual Acuity numbers,
Visual acuity numbers are used to measure the clarity or sharpness of a person’s vision. They are expressed as a fraction, such as 20/20 or 20/40. The interpretation of these numbers is as follows:
- The Top Number: The top number in the visual acuity measurement represents the distance at which the person is standing from the eye chart during the test. For example, if the top number is 20, it means the person is standing 20 feet away from the chart.
- The Bottom Number: The bottom number indicates the distance at which a person with normal vision can read the same line on the chart that the individual being tested can read. For instance, if the bottom number is 20, it means a person with normal vision can read that line from a distance of 20 feet.
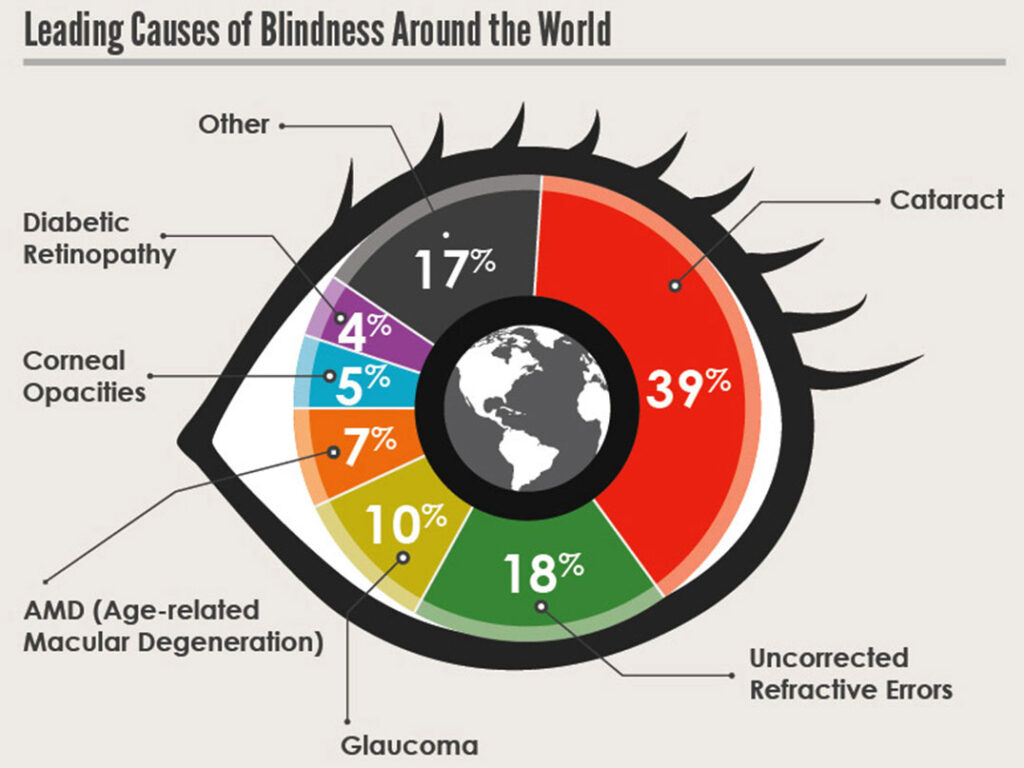
Causes of Visual Impairement
The most common causes of visual impairment globally are uncorrected refractive errors (43%), cataracts (33%), and glaucoma (2%). Visual impairment can be caused by various factors, including genetic conditions, eye injuries, infections, and age-related diseases.
Genetic Conditions:
- Retinitis pigmentosa: A genetic disorder that causes the breakdown and loss of cells in the retina, leading to progressive vision loss.
- Congenital cataracts: Clouding of the lens present at birth, which can cause visual impairment if not treated.
- Glaucoma: A group of eye conditions that damage the optic nerve, often caused by genetic factors.
Eye Injuries:
- Trauma: Injuries to the eye, such as from accidents, sports-related incidents, or workplace hazards, can result in vision loss or impairment.
- Corneal injuries: Damage to the cornea, the clear front part of the eye, can lead to vision problems.
- Corneal Opacification: Corneal opacification, which refers to the clouding or scarring of the cornea, corneal abrasion can be a cause of corneal opacity. In some cases, eye swelling can also cause damage to the cornea that results in opacity.
Infections:
- Ocular infections: Infections of the eye, such as conjunctivitis, uveitis, or keratitis, can cause visual impairment if left untreated.
- Infections during pregnancy: Certain infections, like German measles (rubella), can be transmitted from the mother to the fetus and result in visual impairment in the baby.
- Trachoma: Trachoma is a disease of the eye caused by infection with the bacterium Chlamydia trachomatis. It is a public health problem in 42 countries, and is responsible for the blindness or visual impairment of about 1.9 million people.
Age-Related Diseases:
- Cataracts: Clouding of the lens in the eye, commonly associated with aging, can cause blurry vision and visual impairment.
- Age-related macular degeneration (AMD): A progressive condition that affects the macula, the central part of the retina, leading to loss of central vision.
- Glaucoma: Increased pressure within the eye can damage the optic nerve and result in vision loss.
- Childhood Blindness: Various conditions, including genetic disorders, infections, and developmental abnormalities, can cause visual impairment in children
Other Causes:
- Diabetic retinopathy: Damage to the blood vessels in the retina due to diabetes, which can lead to vision impairment or blindness.
- Amblyopia (lazy eye): Reduced vision in one eye due to abnormal visual development during childhood.
- Medications: Certain medications, such as those used in chemotherapy or for treating autoimmune diseases, can have side effects that affect vision.
- Undercorrected refractive error: Refractive errors, such as nearsightedness, farsightedness, and astigmatism, can cause visual impairment if not corrected with glasses or contact lenses.
- Undetermined: A significant percentage of visual impairment cases were categorized as undetermined, indicating that the cause could not be identified
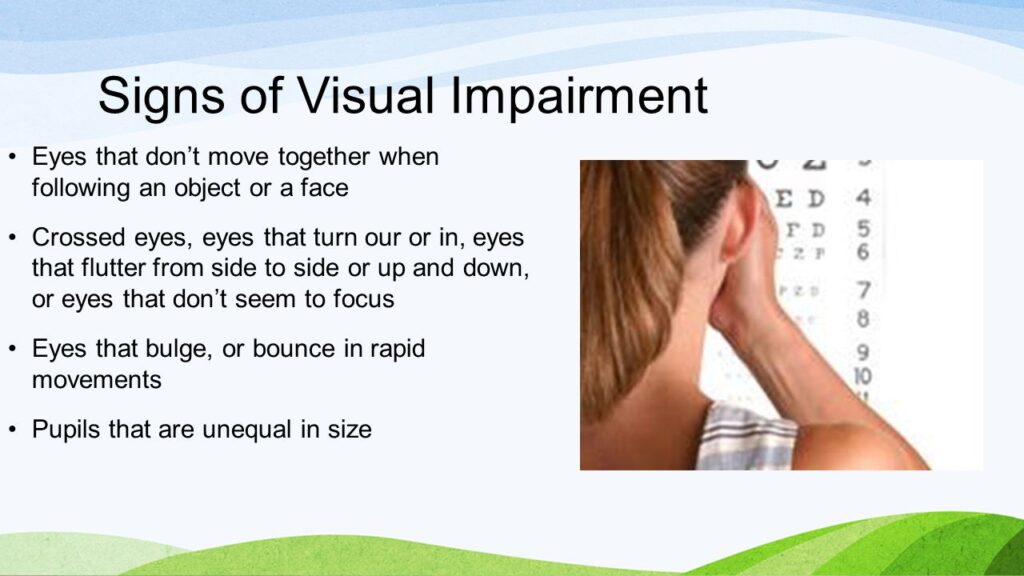
Signs and Symptoms of Visual Impairment
- Blurred Vision: Objects may appear fuzzy or out of focus.
- Double Vision: Seeing two images instead of one.
- Floaters: Seeing spots, specks, or cobweb-like shapes drifting across your field of vision.
- Flashes of Light: Seeing sudden flashes of light, especially in peripheral vision.
- Halos: Seeing circles of light around objects, particularly when looking at bright lights.
- Changes in Iris Color: Noticing a change in the color of the iris, such as a darkening or lightening.
- Eye Pain: Experiencing sudden or recurrent pain in or around the eye.
- Sensitivity to Light: Feeling discomfort or pain when exposed to bright lights.
- Difficulty Seeing at Night: Struggling to see clearly in low-light conditions.
- Loss of Peripheral Vision: Having a reduced ability to see objects or movement in the outer edges of your visual field.
- Inability to see shapes: An inability to see shapes refers to the difficulty in perceiving and recognizing the outlines and forms of objects.
- Cloud vision: Cloudy vision refers to a hazy or blurred visual perception, which can make it difficult to see objects clearly.
- Seeing only shadows: Seeing only shadows means that a person can perceive the presence of light and darkness but cannot distinguish detailed visual information.
- Tunnel vision: Tunnel vision is a condition where a person’s peripheral vision is significantly reduced, resulting in a narrowed field of view.
Visual impairments can also impact daily activities which include:
- Reading: Holding reading material closer to the face, difficulty reading in low light, or experiencing a decrease in reading speed.
- Mobility: Bumping into objects, having trouble navigating stairs or uneven surfaces, or experiencing a loss of depth perception.
- Recognizing Faces and Objects: Difficulty identifying faces or objects, especially from a distance.
- Color Perception: Trouble distinguishing between colors or selecting clothing with appropriate color combinations.
- Eye Strain: Experiencing eye fatigue, headaches, or discomfort after prolonged visual tasks.
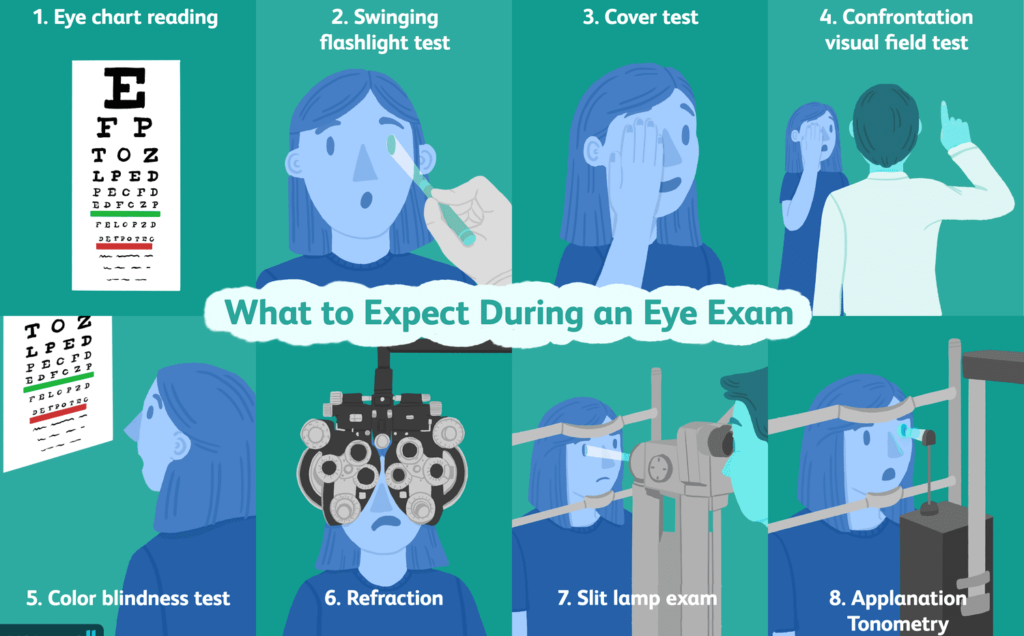
Diagnosis, Tests, and Investigations for Ruling Out Visual Impairment
These assessments help in evaluating the visual functions and identifying any abnormalities or impairments.
History and External Examination:
- A complete history, including family history of visual impairment, is taken.
- External examination of the eye is conducted, which includes assessing the lids, conjunctiva, cornea, iris, lens, etc..
Visual Acuity Test:
- The Snellen test, also known as the visual acuity test, is commonly used.
- The patient reads progressively shortening random letters and numbers from a chart placed at a distance of 6 meters.
- The ability to read the letters at each size determines the visual acuity.
- The test provides a score, represented by two numbers, indicating the patient’s ability to read compared to a person with healthy vision.
Visual Field Test:
- Perimetry and visual field testing are used to assess the integrity of the field of view.
- This test evaluates vision outside the macula and measures the range of peripheral vision.
- The patient’s field of vision is assessed by flashing lights in their peripheral vision, and they are asked to respond when they see the lights.
- Any gaps or abnormalities in the field of vision can be detected through this test.
Tonometry Test:
- Tonometry is performed to evaluate the fluid pressure inside the eye, which helps in detecting glaucoma.
Ocular Motility Assessment:
- This test assesses the movement of the eyeballs and checks for any squint or other problems.
Additional Tests:
- In certain cases, additional tests may be prescribed, such as Visually Evoked Potential (VEP), Electroretinogram (ERG), and Electro-oculogram (EOG).
- These tests evaluate the transmission of signals from the eye to the brain and can be helpful in diagnosing visual impairment, especially in young patients or those with multiple handicaps
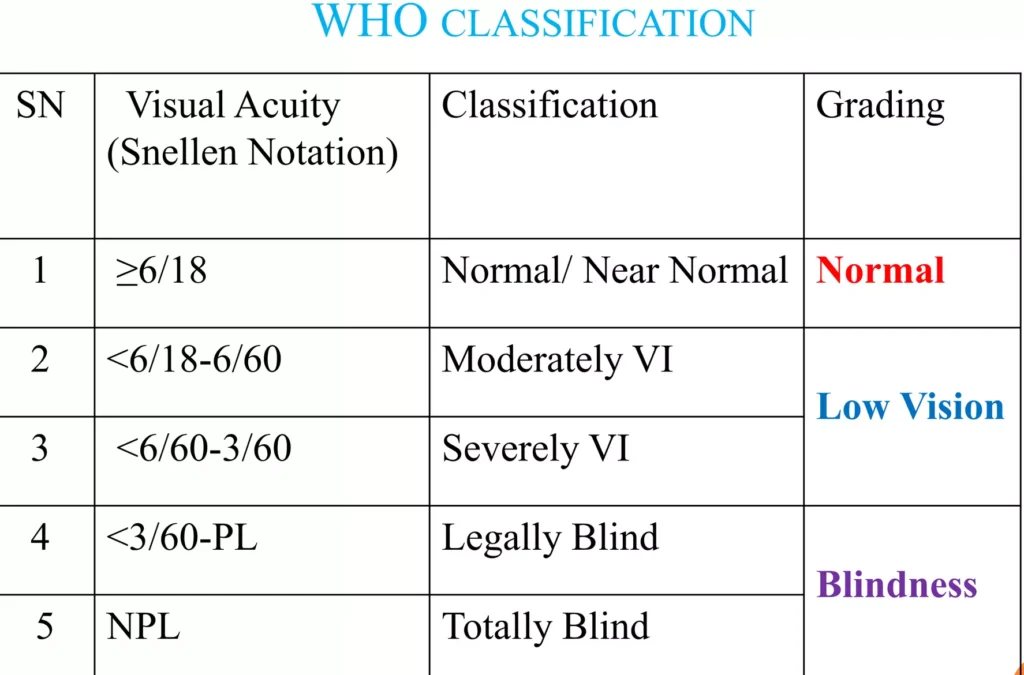
Classification of Visual Impairement
The International Classification of Diseases 11 (2018) provides a classification system for vision impairment, categorizing it into two groups: distance vision impairment and near vision impairment. It is assessed by reading an eye chart from a specific distance.
Distance Vision Impairment:
- Mild: Presenting visual acuity worse than 6/12 – This means that a person with mild distance vision impairment can see at 6 meters what a person with normal vision can see at 12 meters.
- Moderate: Presenting visual acuity worse than 6/18 – Individuals with moderate distance vision impairment can see at 6 meters what a person with normal vision can see at 18 meters.
- Severe: Presenting visual acuity worse than 6/60 – People with severe distance vision impairment can see at 6 meters what a person with normal vision can see at 60 meters.
- Blindness: Presenting visual acuity worse than 3/60 – This category includes individuals with very limited or no ability to perceive visual information.
Near Vision Impairment:
- Presenting near visual acuity worse than N6 or M.08 with existing correction – This refers to difficulties in seeing objects up close, even with corrective measures.
N6: N6 refers to the near visual acuity measurement. It indicates the level of visual clarity or sharpness at a close distance. The “N” stands for “near,” and the number represents the visual acuity scale. N6 refers to the ability to see at a distance of 40 cm (16 inches) with existing correction. In the International Classification of Diseases 11 (2018), N6 is used to classify near vision impairment.
40 cm: 40 cm (or 16 inches) is the standard working distance used to measure near visual acuity. It represents the distance at which a person is tested for their ability to see objects up close. This measurement is commonly used in vision assessments and is considered the standard distance for near vision testing
M.08 refers to presenting near visual acuity worse than N6 or M.08 at 40 cm. This means that individuals with M.08 near vision impairment have difficulty seeing objects clearly at close distances, even with existing correction such as glasses or contact lenses.
Note; Blindness in combination with hearing loss is known as deafblindness .
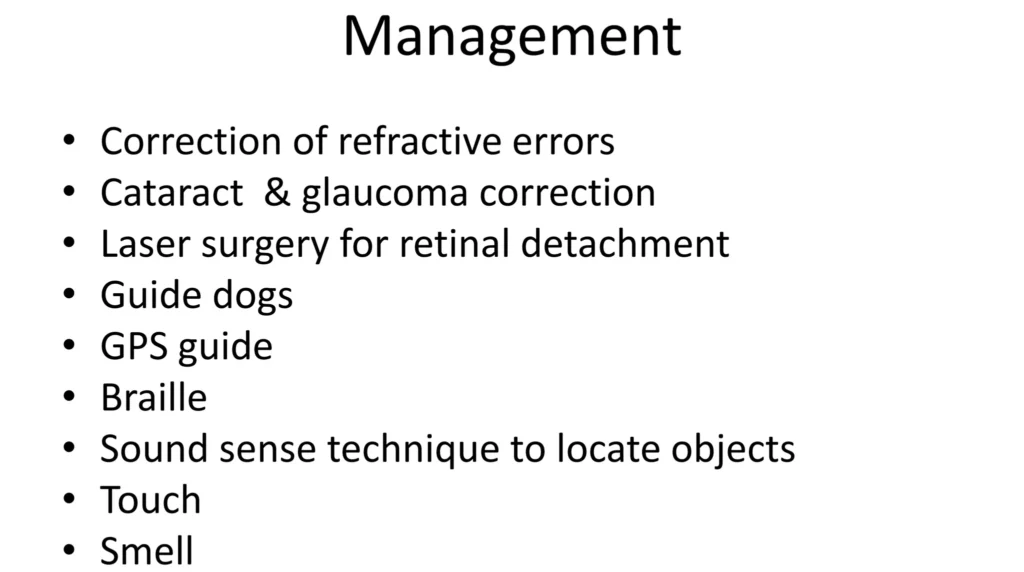
Management of Visual Impairment
Management ranges from Surgery, Pharmacological, Rehabilitation and Prevention.
Patient Reception:
- Greet the patient and their caretaker with empathy and understanding.
- Collect relevant medical history, including information about the visual impairment and any existing assistive devices.
- Provide a comfortable waiting area with appropriate lighting and signage to assist visually impaired individuals.
Medical Assessment and Diagnosis:
- Conduct a thorough examination by an ophthalmologist to determine the cause and severity of the visual impairment.
- Perform necessary tests, such as visual acuity measurements, visual field tests, and imaging studies.
- Discuss the diagnosis with the patient and their caretaker, explaining the implications and available treatment options.
Treatment and Management:
- On return of the results, Prescribe appropriate corrective lenses, such as eyeglasses or contact lenses, if applicable.
- Recommend assistive devices and technology based on the patient’s needs, such as magnification systems, visual aids, and adaptive technology.
- Refer the patient to low vision rehabilitation programs for specialized training and support.
- Provide information about available support services, such as counseling, support groups, and registration as visually impaired if necessary.
Rehabilitation and Training:
- Arrange orientation and mobility training to help the patient navigate their environment safely and independently.
- Offer daily living skills training to enhance independence in activities of daily living.
- Provide access to Braille literacy programs for those interested in learning Braille. Braille is a tactile writing system used by people who are blind or visually impaired. It consists of raised dots arranged in cells, which can be read by touch.
- Facilitate low vision rehabilitation programs to maximize the patient’s remaining vision through training and adaptive strategies.
Emotional and Psychological Support:
- Offer counseling services to address emotional and psychological challenges associated with visual impairment.
- Connect the patient and their caretaker with support groups to share experiences and receive peer support.
- Collaborate with mental health professionals to address any psychological issues related to visual impairment.
Ongoing Monitoring and Follow-up:
- Schedule regular follow-up appointments to monitor the patient’s visual health and adjust the management plan as needed.
- Provide educational resources and information to the patient and their caretaker for continued self-care and support.
Discharge:
- Ensure that the patient and their caretaker understand the management plan and have access to necessary resources and support services.
- Provide written instructions, including medication details, follow-up appointments, and contact information for further assistance.
- Coordinate with other healthcare professionals involved in the patient’s care to ensure a smooth transition post-discharge.
Surgical Management:
Surgical management is crucial according to the cause of the visual impairement.
Cataract Surgery:
- Cataract surgery is a common surgical procedure to treat visual impairment caused by cataracts.
- During the surgery, the clouded natural lens of the eye is removed and replaced with an artificial lens called an intraocular lens (IOL).
- This procedure is usually highly successful in restoring vision and improving visual acuity.
Corneal Transplant:
- In cases where visual impairment is caused by a scarred or damaged cornea, a corneal transplant may be considered.
- During the procedure, the damaged cornea is replaced with a healthy cornea from a donor.
- Corneal transplants can help improve vision and restore clarity to the cornea.
Retinal Surgery:
- Retinal surgery may be performed to address visual impairment caused by retinal conditions such as retinal detachment or macular holes.
- The specific surgical techniques used depend on the underlying condition and may involve repairing or reattaching the retina.
- Laser surgery may also be used to treat certain retinal conditions, such as diabetic retinopathy or retinal tears.
Glaucoma Surgery:
- In cases where visual impairment is caused by glaucoma, surgical interventions may be necessary to manage the condition.
- Different types of glaucoma surgeries are available, including trabeculectomy, tube shunt surgery, and laser trabeculoplasty.
- These procedures aim to reduce intraocular pressure and prevent further damage to the optic nerve, thus preserving vision.
Prevention
- Eat a Nutritious Diet: Consuming a balanced diet rich in fruits, vegetables, and omega-3 fatty acids can help maintain good eye health.
- Get Regular Eye Exams: Regular eye exams are crucial for early detection and treatment of vision problems. The frequency of eye exams may vary depending on age and risk factors.
- Know Your Family’s Eye History: Understanding your family’s history of eye problems can help identify potential risks and take preventive measures.
- Follow a Healthy Lifestyle: Maintaining a healthy lifestyle, including regular exercise and not smoking, can contribute to overall eye health.
- Protect Your Eyes from Trauma: When engaging in activities that pose a risk to your vision, such as sports or working with hazardous materials, wear durable eye protection to prevent injuries.
- Avoid Harmful Substances: Avoid smoking, as it is a major risk factor for vision problems such as macular degeneration and cataracts. Additionally, minimize exposure to harsh chemicals and protect the eyes from harmful substances.
- Protect Your Eyes from UV Radiation: Wear sunglasses that provide 99-100% protection against UVA and UVB rays to shield your eyes from the harmful effects of UV radiation.
- Practice Good Eye Hygiene: Take breaks when using digital devices or performing concentrated activities to prevent eyestrain. Blink regularly to keep your eyes lubricated and use artificial tears if needed.
- Manage Chronic Conditions: Properly manage chronic conditions like diabetes and high blood pressure, as they can contribute to vision problems.
- Genetic testing: Genetic testing can be helpful in prevention of genic eye disorders such as Retinitis pigmentosa.