PREPARATORY QUESTIONS FOR END OF SEMESTER EXAMINATIONS
SURGERY
1a) define the term epistaxis
b) What are the causes of epistaxis?
c) Write down the management of a patient presenting with epistaxis
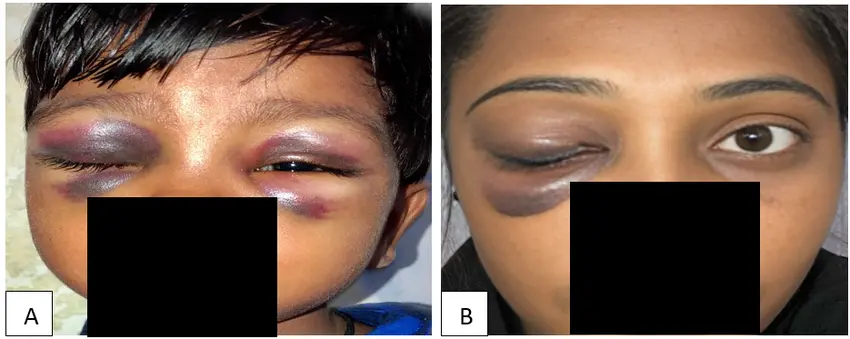
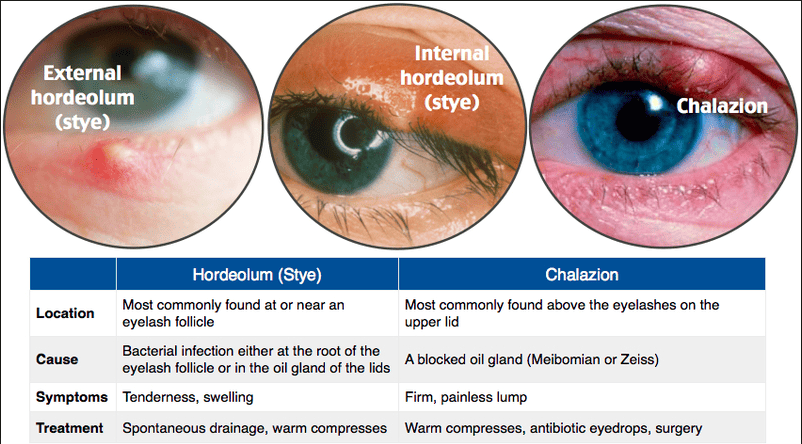
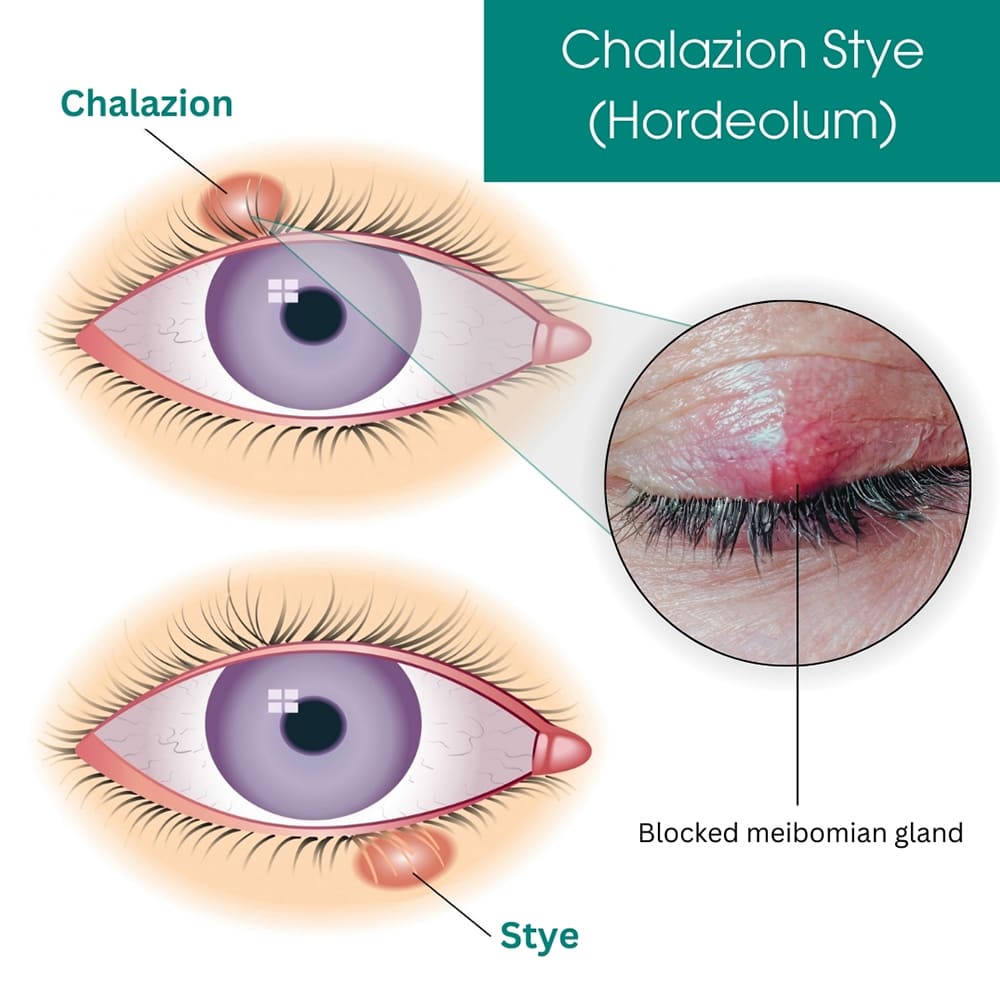
2a) define a sty
b) What are the causes of a sty?
c) Outline the signs and symptoms of a sty
3 An adult has been admitted to a surgical ward with difficulty in breathing, he requires urgent tracheostomy.
a) List the indications of tracheostomy
b) Describe the post-operative management of this patient till discharge
c) Outline the complications that are likely to occur
d) Formulate five actual nursing diagnoses and four potential diagnoses from this patient with tracheostomy
4. Mrs Akello 38years old has presented with nasal polyps and she is to undergo polypectomy
a) List the causes of nasal polyps
b) Outline the signs and symptoms of nasal polyps
c) Give the specific pre and post-operative management of this patient
d) List four complications of nasal polyps
5. a) Define tonsillitis
b) List 6 symptoms and signs of a patient with tonsillitis
c) Give the specific post-operative management for a patient who has undergone tonsillectomy
6. Mrs Nabukeera was admitted on a surgical with a diagnosis of adenitis .She is to undergo adenoidectomy
a) Define adenitis
b) List the signs and symptoms of adenitis
c) Describe the specific post-operative management you would give to her till discharge
7. a) Define burns
b) What are the causes of burns?
c) How can burns be classified
d )Mr. KK has sustained burns on the neck and chest
>calculate the percentage of the area burnt
>what specific management do you give to Mr. KK in the first 72hrs of admission
>give five actual nursing diagnoses Mr KK will have due to the burns
8a) Define the term electrolyte imbalance
b) Give the causes of electrolyte imbalance
c) List the signs and symptoms of electrolyte imbalance
d) Mention the types of electrolyte imbalance in the body
e) How can you manage patient with electrolyte imbalance
9a) Define the term gangrene
b) What are the causes of gangrene?
c) Write down the types of gangrene
d) Mention the signs and symptoms of different types of gangrene
e) Describe the specific management which is given to this patient with gas gangrene
10a) Define the term shock
b) Write down the types/classification of shock
c) State the clinical features of shock
d) Write down all possible complications of shock
e) How can a health worker prevent surgical shock?
11a) Outline the classifications of wounds
b) Give the factors that delay wound healing
c) State five complications of wounds
d) What advice do you give to a patient about wound care at home who is due for discharge?
e) Explain the process of wound healing
12a) Define the term a fracture
b) Mention the different types of fracture
c) Describe the management of a closed fracture of a femur
d) List any 6 complications of a fracture
13a) Define the term inflammation
b) List the signs and symptoms of inflammation
c) Describe the process of inflammation
d) Explain the specific management of a 12yr old patient with inflammation on the lower limb
13A 28year old male was admitted on a surgical ward with a diagnosis of tetanus
a) List five cardinal signs and symptoms this patient would present with
b) Explain the specific nursing management you would give to this from admission to discharge
c) Formulate four actual and two potential nursing diagnoses from this patient’s condition
14a) Define the term immunity
b)Classify immunity
c) Explain the factors that affect an individual’s immune system
15a) Define hemorrhage
b) Explain the different types of hemorrhage
c) Explain the mechanism of hemostasis
d) Outline the specific management of a patient with severe bleeding on the left lower leg
16a)What is blood transfusion?
b) Describe five complications that may occur due to blood transfusion
c) What would cause failure of of a blood drip to run during blood transfusion
d) Explain the nurse’s responsibility before , during, and after blood transfusion
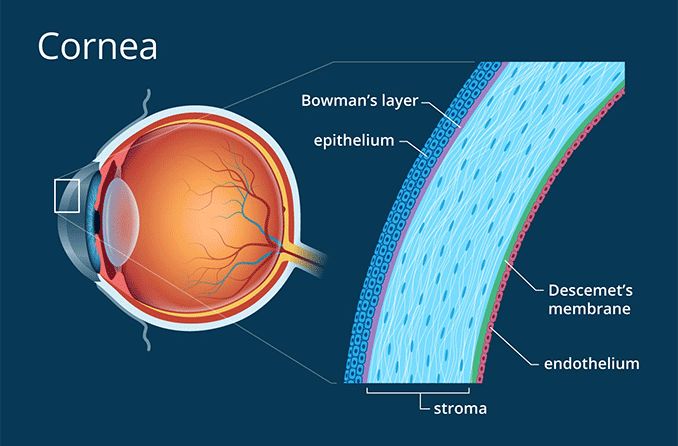
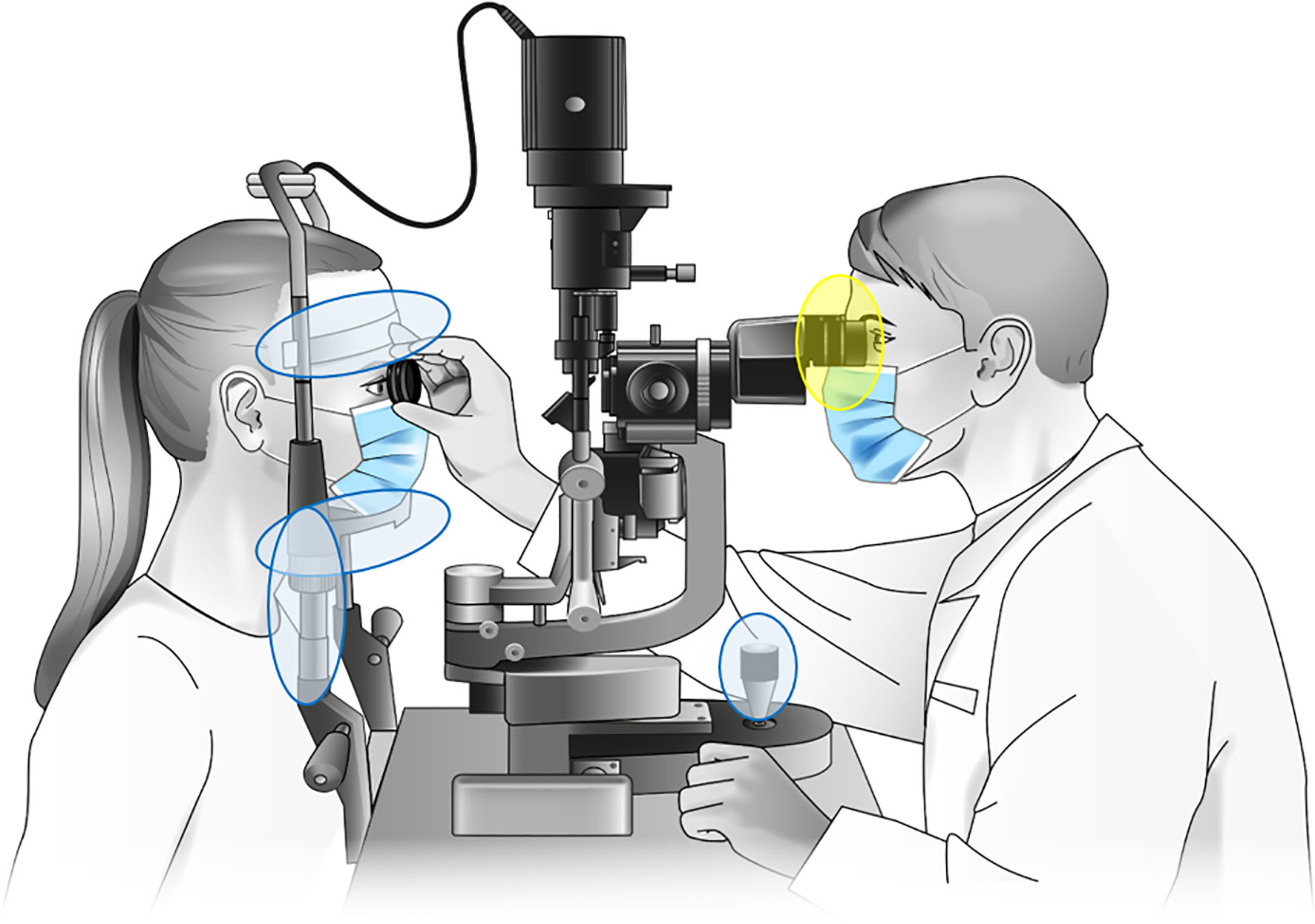
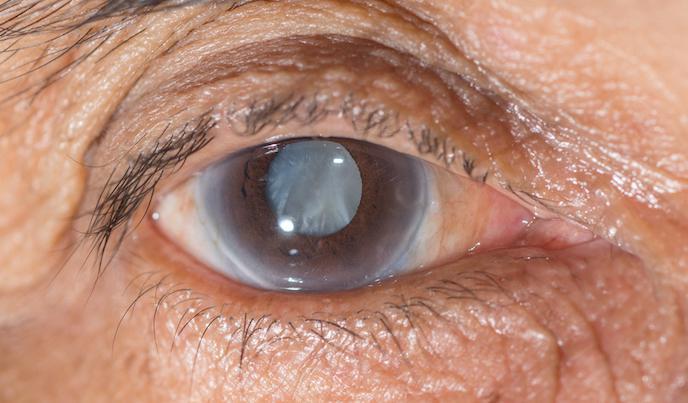
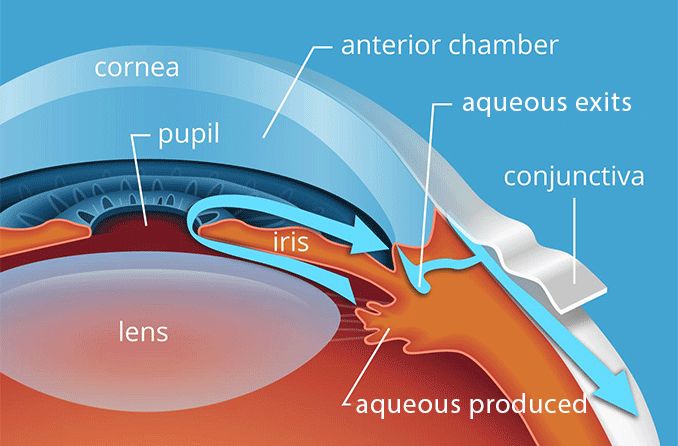
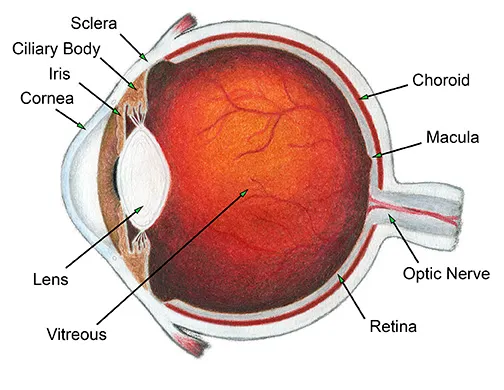
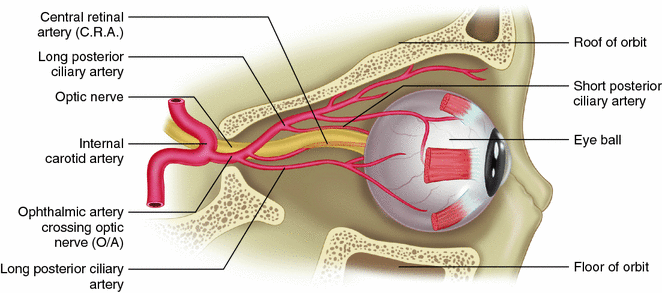
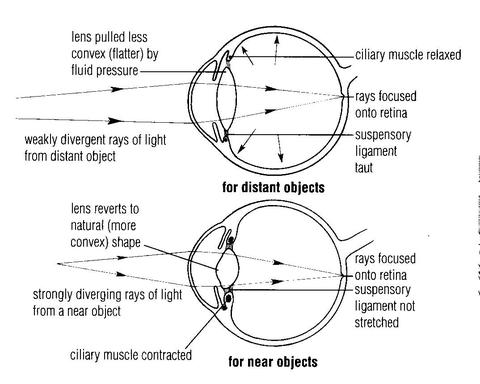
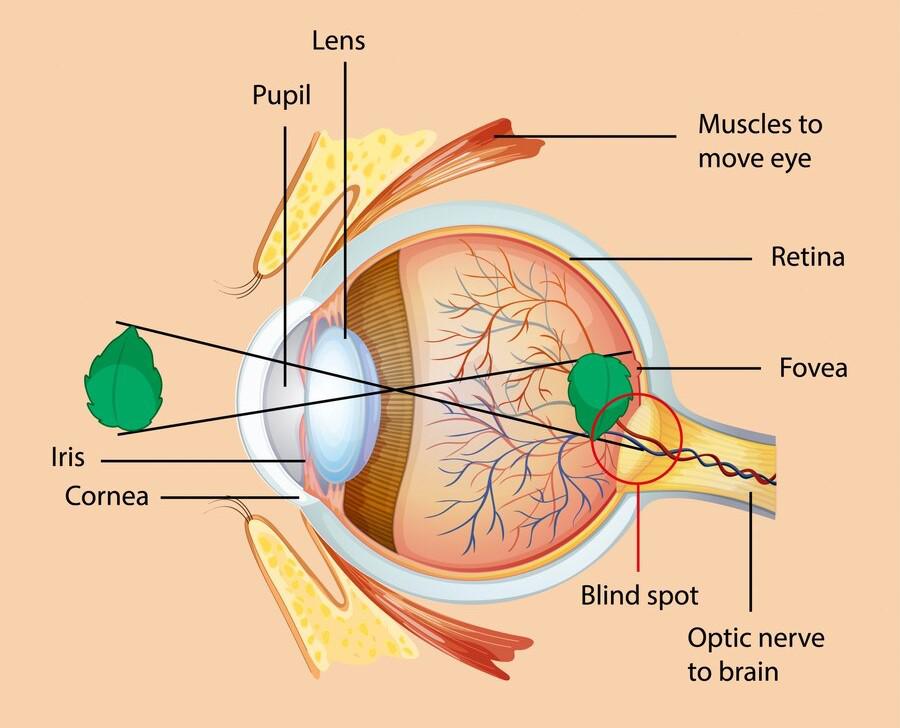
17a) Define a cataract
b) outline the cardinal signs of a cataract
c)Describe the management of Mr Moses a 40yr old presented to your OPD department with a cataract using a nursing process
d)list the likely complications of a cataract
MENTAL HEALTH
18. Define the following terms
a)suicide
b) Suicidal ideation
c) Attempted suicide
d) par suicide
e) paradoxical suicide
19a) outline the common psychiatric conditions associated with suicidal ideation
b) Explain the common factors contributing to suicide in the community
c) Mention the impact of suicide to the family and the community
d) Describe the management of a patient who intends to commit suicide
e) Explain the assessment you would carry out on a patient with suicidal ideation
20a) Define PTSD
b) Outline four signs and symptoms of a patient with PTSD
c) Manage an 11yr old girl who presented with PTSD after rape
21a) Define the term delirium tremens
b) Identify the causes of delirium tremens
C) How can you manage the patient with delirium tremens?
d) Formulate 5 potential nursing diagnoses for a patient with delirium tremens
22. Madam EKEB a 26yr old is very aggressive on the ward that she cares away fellow patients
a) Differentiate between aggression and violence
b) What management do you give to madam EKEB who presents with severe aggression on the ward?
23a) what is a psychiatric emergency?
b) List 10 common psychiatric emergencies
c) Which admission procedure would you follow when admitting a patient presenting with any of the psychiatric emergencies
23a) Explain standards of care in psychiatry
b) Who is a class B criminal lunatic?
c) Mention all the orders used to admit mentally ill patient
d) Write down and explain all the sections used in discharging a mentally ill patient
e) Outline the rights of a mentally ill patient
24. A 30yr old patient has presented in a psychiatric ward with status epilepticus
a) Define status epilepticus
b) Manage the patient who presents with status epilepticus on a ward
c) Formulate four potential and 2actual nursing diagnoses for a patient with status epilepticus
25aDefine mental retardation
b) Classify mental retardation
c) Explain 8 causes of mental retardation
d) What advice do you give to a family with a mentally retarded child?
26. ADHD is one of the common psychiatric conditions in children
a) Outline 6 signs and symptoms of ADHD
b) Manage an 11yr old boy with ADHD
c) What specific advice do you give to a family with a child having ADHD?
27a) Define autism
b) Explain the common features of autism
c) Describe the management of the above condition
28. Depression is one of the common psychiatric conditions
a) Define depression
b) Outline the specific management of a patient with severe depression on a psychiatric ward
c) Make 4 priority nursing diagnoses for a patient with severe depression
COMMUNITY HEALTH
29. a) Define PHC
b) Mention the principles of PHC
c) Outline components /elements of PHC
d) What strategies are used to achieve PHC activities in a given community?
30a) What is community assessment?
b) Explain how you would identify any health problems in a given community
c) Outline 9 important information you would find out in a given home during assessment
31a) Define a home visit
b) Explain how you apply a nursing process during a home visit
c) Outline the merits and demerits of a home visit
32a) Define vital statistics in health
b) Explain the importance of vital statistics in health
c) Outline 6 key vital statistics used to determine the health status of a community or country
33a) Explain the relationship between PHC and CBHC
b) Explain the role of a community nurse/midwife in implementation and achievement of any 4 of the PHC principles
c) Outline the advantages of PHC over other specialized medical services
34a) Define community mobilization
b) Describe how you would mobilize a community towards implementation of a health education program
35a) Define school health
b) Explain the importance of a school health program
c) Explain the role of a nurse in the provision of a school health program
d) Outline the components of school health services
36a) Explain the role of a community in PHC services
b) Give 8 advantages of community participation in PHC services
c) Explain the obstacles to effective community participation in PHC programs
37a) Define community diagnosis
b) Discuss why community diagnosis is important
c) Explain the steps in conducting community diagnosis
38Health promotion are actions related to lifestyles and choices that maintain/enhance population health
a) Outline any 5 health promotion interventions you would implement in a given a community
b) Explain 5major steps in community mobilization
39. Describe the different levels of disease prevention
40. Appropriate technology is one of the elements of PHC
a) How is appropriate technology expressed in implementation of PHC services?
b) Explain the advantages and disadvantages of appropriate technology as an element
41. a) Define the term epidemics
b) Explain the factors that contribute to the causes of epidemics
c) What is the role of a nurse in the management of an epidemic in the community?
42a) Define community health and community based health care
b) State the characteristics of CBHC
c) Describe how you would enter a village in Mityana to implement a community health activity
TROPICAL MEDICINE
43a) Define schistomiasis
b) Explain the different types of schistosomiasis
c )Give the clinical manifestations of schistosoma mansoni
d) Describe the lifecycle of schistosomiasis haematobium using a well labelled diagram
e) Outline the preventive measures of all types of schistosomiasis
44The current disease burden in Uganda is attributed to communicable diseases
a) Describe the modes of transmission of communicable diseases in general
b) Describe the methods/approaches used to prevent and control communicable diseases in the community
c) Explain the types of water diseases and their examples
45a) Define diarrhoea
b) Outline the causes of diarrhoea in Uganda
c) Discuss the drugs used in the management of diarrhoea in children
d) Formulate 5 priority nursing diagnoses of this patient
46a) Define measles
b) Outline the signs and symptoms of measles basing on the stages
c) Describe the management of a12yr old child presenting with measles from admission to discharge
d) List the likely complications of measles
47. Malaria is one of the communicable diseases affecting most communities of Uganda
a) Classify malaria
b) Outline the cardinal signs of complicated malaria
c) Describe the lifecycle of malaria in both man and the mosquito with the aid of diagrams
d) How can different communities prevent the spread of malaria?
e) Make 5 actual and 3 potential diagnoses of malaria
48a) Describe the life cycle of ackylostomiasis with the aid of diagrams
b) Explain the preventive measures of hook worm infestation
c) List the likely complications of neglected worms
49a) Ebola is one of the hemorrhagic fevers devastating some communities and countries due to known and unknown reasons
a) Define hemorrhagic fevers
b) List the different hemorrhagic fevers
c) Outline the different causes and predisposing factors to hemorrhagic fevers
d) Describe the management of Mr. X presented to your hospital suspected to be an Ebola patient
50a) Define rabies
b) Describe the management of rabbis both at home and in the hospital
c) Explain the complications of rabies
51a) Define bacilliary dysentery
b) State the differences between bacilliary dysentery and amoebic dysentery
c) Describe the specific management of a 3yr old child with bacilliary dysentery from admission to discharge
52a) Define typhoid fever
b) Explain the cardinal signs and symptoms of typhoid fever
c) Describe the important information you would give to the community concerning prevention of typhoid fever
53a) Define trachoma
b) Outline the signs and symptoms of trachoma
c) Explain the management of 23yr female presenting with trachoma
d) List the complication
54. Samuel a 30yr old peasant has been presented to the OPD with all the features of tetanus
a) Outline the clinical features of tetanus
b) Describe the management from admission to discharge
c) List the complications of tetanus
MIDWIFERY 1 AND 2 AND OBSTETRIC ANATOMY
55. List the 5 medications used in antenatal and discuss them under
a) Dose
b) Indication
c) Side effects
56a) Outline the obstetrical causes of anemia in pregnancy
b) List the five causes of hemolytic anemia
c) Describe the management of Mrs. mucosal who presents at 36weeks with severe anemia
57a) Define a cervix
b) With the aid of a diagram, describe the structure of the cervix
c) Outline the 6 functions of the cervix
58a) Define the term good antenatal care
b) Give the indications of referring a mother to a doctor during this period
c) How would you manage a mother who comes with lower back pain in antenatal at 32weeks?
59a) Define normal puerperium
b) Describe the management of a mother who has had normal delivery up to discharge
c) List the complication that may occur during this period
60a) Outline the symptoms of pregnancy
61a) Explain the characteristics of normal uterine action during first stage of Labour
b) What is the management of a gravid 3 para 2 mother at term who presents to hospital with history of precipitate Labour on the previous pregnancies?
62a) Describe a vagina
b) What information is got on vaginal examination during labor?
c) Mention four contractions of vaginal examination giving reasons for each
d) List the complications of vaginal examination
63a) Define intrauterine fetal death
b) Outline the causes of IUFD
c) How is the diagnosis of IUFD made?
d) What is the management of IUFD in the hospital?
64a) Describe the pelvic floor
b) Outline injuries that can occur to the pelvic floor during Labour
c) Explain how the knowledge of fetal skull can help you as a midwife prevent perineal tears
65a) Describe the fetal skull
b) How is fetal wellbeing monitored during pregnancy?
C) List the indications of ultrasound scan in late pregnancy
66a) Describe a non-pregnant uterus
b) Describe the changes that take place in this organ during pueperium
c) List the likely complication in the first stage of labor
67a) what is the effect of DM on pregnancy?
68a) how does pregnancy affect DM?
b) How would you care for a diabetic mother who has had a caesarean section in the first 48hours of the operation
69a) Describe the umbilical cord
b) Describe the different abnormalities of the cord
70. Malaria is of the conditions contributing affecting pregnancy and contributing factor to increased maternal mortality and morbidity
a) Explain why pregnant women are more susceptible to malaria
b)Describe the a primigravida who presents to your maternity center at 34 weeks with severe malaria
c) Outline the likely complications of malaria on pregnancy
71. Essential hypertension is one of the hypertensive disorders experienced by pregnant women
a) Define essential hypertension
b) Classify hypertensive disorders in pregnancy
c) Describe the management of Mrs Nangobi a G4P2+1 presenting in antenatal clinic at 32weeks with a diagnosis of essential hypertension
d) How does hypertension affect pregnancy?
72a) outline the signs and symptoms of first stage of Labour
b) Describe the management of a young primigravida in first stage of Labour
c) List the complications likely to occur during this stage of Labour
73a) Define hyperemesis gravidarum
b) Outline the causes of hyperemesis gravidarum
c) Describe the management of G2P1+0 presenting to your maternity center with hyperemesis gravidarum at 28 weeks of gestation
d) Explain the likely complications of this condition
74a) what is preeclampsia
b) Outline the signs and symptoms of preeclampsia
c) What are the predisposing factors of this condition?
d) Outline the nursing of a mother with severe preeclampsia
e) List the complication of severe preeclampsia
75a) Describe the placenta at term
b)Explain the functions of the placenta
c) Outline the abnormalities that may be found on the placenta
76a) With the aid of a diagram, describe the structure of the female breast
b) Explain the physiology of lactation
c) Explain the factors that promote successful lactation
77a) Define labor
b) Explain the physiology of the first stage of Labour
c) Describe the management of a mother in the second stage of Labour admitted in the hospital
78a) Outline the changes in the cervix during the first stage of labor
b) What information is found on the partograph?
c) A G2P1+0 mother came to a health center in normal labor , what may make you refer?
79. Most women find it helpful to get further information and support in their own homes.
a) Give 5 advantages of following up post-partum mothers
b) Explain postpartum maternal assessment you would carry out during domiciliary care
c) List the problems that you would identify during domiciliary care
80a) Describe 6 factors that influence the length of second stage of labor
b) Explain 3 phases used in conducting 2nd stage of labor
c) Give immediate assessment of the baby after 2nd stage of labor
81a) Mention factors that aid in involution of the uterus
b) Explain how you assess and document uterine involution immediately after delivery to 10days postpartum
c) Give five complications of sub involution of the uterus
82a) Explain the antenatal appointment schedules
b) Give 6 barriers to adherence to goal oriented antenatal visits
c) Identify 5 complications a pregnant woman is likely to get if no antenatal is attended
83a) Describe the structure of the ovary
b) List the functions of the ovary
c) Describe the menstrual cycle
MEDICINE I AND 111
84. Mr. KIBULA known hypertensive has been brought to hospital with suggestive features of hypertensive crisis.
a) Mention 8 clinical features of hypertension
b) List 4 causes of HTN and predisposing factors
c) Explain the specific Nursing Care you will give to Mr. KIBULA from the time of admission to discharge.
85. Write short notes on the following (definition, causes, signs and symptoms and complications).
a) Hydrocele
b) Hodgkin’s disease
c) Ankylosing spondylitis
86 a) Define Paget’s disease/Osteitus, deformans?
b) Explain the pathophysiology and etiology of Paget’s disease
c) Describe the specific nursing care you would give to Mr. Muwonge with Paget’s disease
87. Hepatitis B morbidity and mortality is much higher today than before.
a) What are the factors, contributing to the high prevalence of hepatitis B in the communities
b) How does a patient with hep.B present?
c) Give five priority nursing diagnoses for a patient with Hep B infection.
d) Describe the specific nursing management you would give to a patient with hep B.
e) Mention the complications of hep B.
f) Suggest ways how we can prevent hep B infection in the community
88. Define myocardial infarction. List the clinical features of myocardial infarction.
Explain the specific Nursing care given to a patient with myocardial infarction within the first 24Hrs of admission.
89. An adult male patient has presented to OPD with features of pulmonary tuberculosis
a) Outline five cardinal signs and symptoms of pulmonary tuberculosis.
b) List five specific investigations that can be done to confirm pulmonary tuberculosis.
c) Explain the specific nursing care given to this patient from the time of admission until discharge.
90. Mrs. A, a female patient has been admitted on a medical ward with suspected bronchial pneumonia,
a) Outline the clinical features of bronchial pneumonia
b) Describe the specific nursing management you would give to Mrs. X with in the first 72HRS of admission.
c) Explain five likely complications Mrs. X is likely to get following this condition.
91. Mr. Lusoke, a 62 yrs. old male is presented at the OPD with features of congestive cardiac failure
a) Outline the signs and symptoms of congestive cardiac failure.
b) Mention the causes of congestive cardiac failure.
c) Describe the specific nursing care / management you will give to Mr. Lusoke from time of admission to discharge.
92. Outline the signs and symptoms of Parkinson’s disease.
b) Mention the causes and predisposing factors to Parkinson’s disease.
c) Describe the specific Nursing management given to a patient with Parkinson’s disease.
93. Mr. Okello a 28yrs old male presents at OPD with clinical features of urinary tract infection and was admitted.
a) List 5 causes and 6 signs and symptoms of urinary tract infection.
b) Describe the specific nursing care you would give to Mr.Okello within the first 48 hours of admission.
c) Give the measures that can be taken to prevent urinary tract infections.
94 Define Addison’s disease?
b) Outline the causes and risk factions that leads to Addison’s disease.
c) Using the Nursing process, describe the management of a patient with Addison’s disease.
PEDIATRICS 1 AND 11
95. Define the term Apgar score
a) Outline 10 characteristics of a normal new born baby
b) Describe the care given to the normal new born baby within 72 hours after delivery of the head.
96. Differentiate between SAM and MAM
b) Explain the causes of malnutrition in children under 5 years.
c) Explain the importance of breastfeeding in babies’ up to 2years of age.
97. Define the term congenital abnormalities
a) Classify the congenital abnormalities of the heart
b) Explain ways of preventing congenital abnormalities.
98. Mention the factors that predispose to neonatal infections in new born babies.
b) List 8 clinical features of a child with neonatal tetanus.
c) Describe the specific management of a 3 month old child with tetanus.
99. Outline the factors that predispose to birth injuries
Differentiate between a caput succedaneum and a cephalo hematoma.
c) Describe the specific management you would give to a new born baby who presents with a caput succedaneum.
100. Brandon a five weeks old neonate is admitted on ward with a history of fast breathing, chest in drawing and stridor.
b) Explain the specific nursing care you would offer to Brandon in a hospital within the first eight hours of admission.
101. A five year old child has been bought to OPD in a painful sickle cell crisis.
a) Outline 5 possible causes of sick cell crisis.
b. List 4 diagnostic signs and symptoms of sick cell disease in children.
c) Explain the specific management of this child from admission to discharge.
102. A 4 months old baby has been admitted on a pediatric ward and diagnosed with pneumonia.
a) Outline the clinical presentation of this child.
b) Explain the specific management given to the child with in the first 72 hours.
103. Define the following terms.
1) Fracture
ii)Osteopenia of prematurity
osteogenesis imperfecta
Osteomyelitis
b) Mention 5 signs and symptom of osteomyelitis in children.
c) Describe the nursing management of 3 years old child with osteomyelitis.
104. A 8 month old child has been diagnosed with nephrotic syndrome.
a) List 6 signs and symptoms of nephrotic syndrome in children.
b) Describe the specific nursing management you world give to this child within the first 72 hours of admission on a pediatric ward.
c) Outline five complications of nephrotic syndrome.
105. What are the advantages of breast feeding?
Compare human milk and cow’s milk
Outline problems that are faced by mothers during breastfeeding.
106. List five congenital abnormalities of the G’T and 5 musculoskeletal system
Outline the causes of congenital abnormalities.
How do you cause a mother who has delivered a baby with spinal bifida?
107. List the factors that promote good nutrition in the under-five.
List five pieces of advice you would give to a prime para with a two year old baby suffering from protein calorie malnutrition.
List five problems of birth injuries in Uganda.
Outline the roles of a nurse in prevention of birth injuries in Uganda.
PHARMACOLOGY 1 AND 111
108. Define rational drug use
Outline the medical classification of drugs giving examples of each
Mention the legal classes of drugs with examples of each.
109. Define infertility.
State the common cause of infertility in women
c) State the indications, side effects and contraindications of clomiphene and Bromocriptine.
110. Describe the mechanism of action of non-opioid analgesics.
b) Write briefly about the handling of the class of drugs in a hospital
c) Define the following:-
Chemotherapy
Anti tussive
111. Mention 4 Four sources of drugs
b) Write down all routes which can be used for drug administration giving advantages and disadvantages of each.
c) Write down the factors that affects drugs absorption.
d) What factors affect drug dosage and action?
112. State the clinical uses of oxytocin and mention 6 adverse side effects of the drug.
b) Outline 5(five) contraindications of oxytocin
c) Describe 10 (ten) Nursing considerations while administering oxytocin.
113. Define Narcotic drugs and state the types of narcotics.
b) List down 7 nursing considerations before during and after administrating narcotics on ward.
c) What are the legal implications of Narcotics according to the Uganda narcotic drugs and psychotropic substance control ACT?
114. Define immunity and explain the two major types of immunity.
State the specific side effects, indication and the dosage following drugs:-
- Anti D (RHO) Immunoglobulin
- B) Rabies vaccine
- Pneumococcal Vaccine.
115. Describe the physiology of erection in males
b) State the causes of erectile dysfunction
b) Mention the class, indication, Dosage and side effects of the following drugs.
i) Sildenafil.
ii) Tadalafil
iii) Finesteride.
GYNAECOLOGY
- a) Outline signs of breast cancer.
b) Explain post operative care after mastectomy.
c) List possible complications of mastectomy.
- . a) Draw a diagram showing possible sites of vaginal fistula.
b) Outline the 5 major causes of vaginal fistula.
c) Explain specific nursing care of a woman after VVF repair.
118. a) Define the different types of Abortion.
b) Outline causes of missed Abortion.
c) Explain different methods used in the management of missed abortion.
d) Outline the 5 elements of PAC.
- a) Define ectopic pregnancy.
b) Outline signs and symptoms of tubal pregnancy.
c) A mother presents to the medical facility with a tubal pregnancy, describe her management till discharge.
119. a) List the disorders of menstruation.
b) Explain the advice and treatment given to a 17 year old girl with dysmenorrhea.
120 a) Define Hydatidiform mole.
b) Outline signs and symptoms of hydatidiform mole.
c) Describe the methods of managing the above condition and list complications that may follow.
121. Describe pelvic inflammatory disease.
b) What are the predisposing factors of this condition?
c) Describe management of PID in the hospital.
- a) What is infertility?
b) Outline causes of infertility.
c) Explain the different methods that can be used to manage infertility.
- a) Draw a diagram of a uterus indicating sites of fibroids.
b) Differentiate between benign and malignant tumor.
c) Give the management of the mother after myomectomy within the first 48 hours.
d) What specific advice would you give this mother on discharge.
REPRODUCTIVE HEALTH
- a) Define STDs?
b) Explain ten preventive measures against sexually transmitted infections.
c) Describe the syndromic management of STDs.
- a) List 7 components of reproductive health.
b) Outline the advantages and disadvantages of intergrating reproductive health.
c) Outline 10 factors that affect women’s reproductive health.
- a) Define sexual abuse?
b) Explain factors that expose adolescent girls to sexual abuse or vulnerability.
c) Outline 5 clinical features of sexual abuse in an adolescent.
- a) Define i) Post Abortion Care
ii) Comprehensive abortion care.
b) Explain the Rational for PAC.
- a) Who is an adolescent?
b) Describe Tanner’s stage of development in an adolescent.
c) List common health problems faced by adolescents.
- a) What is safe motherhood?
b) Outline the 3 delays that can increase maternal mortality.
c) What is your role as a midwife in reduction of maternal mortality in your community?
- Describe syndromic approach of managing STIs.
- a) Define domestic violence.
b) What are the factors that make you suspect that one is a victim of domestic violence?
c) How would you prevent domestic violence?
- Describe manual vacuum aspiration.
FOUNDATIONS OF NURSING.
- a) Define wounds.
b) Give 5 types of wounds.
c) Outline the factors that delay wound healing.
d) Give the specific management for a patient with specific wound.
e) What specific advice do you give to a patient with a wound prior to discharge.
f) Describe the process of wound healing.
- a) Outline the indications for oxygen administration.
b) Give the rules to follow before, during and after administration of oxygen.
c) Define blood transfusion.
d) Outline the indications of blood transfusion.
e) Outline the appropriate care of the patient before, during and after blood transfusion.
f) Give the complications of blood transfusion.
- a) Define drug administration.
b) Outline the different routes of drug administration.
c) Mention the principles of drug administration including the dos and don’ts in drug administration.
- a) Define infection prevention and control.
b) Define nosocomial infection.
c) Outline the steps taken to prevent infections of the wound.
d) What are the advantages of oral route drug administration over the parental route.
- a) Outline the indications of Tracheostomy.
b) Give the specific pre and post operative nursing care for the patient with tracheostomy.
c) Mention the complications of tracheostomy.
d) Formulate 4 actual nursing diagnoses for a patient with colostomy.
- a) Define lumber puncture.
b) Outline the indications of lumber puncture.
c) Explain the specific nursing care given to the patient prior to after the procedure of lumber puncture.
d) List the complications of lumber puncture.
- a) Define abdominal paracentesis.
b) Outline the indications of paracentesis.
c) Give the specific care given to the patient before and after abdominal paracentesis.
d) Mention the complications of abdominal paracentesis.
- a) Define tractions.
b) Explain the different types of tractions.
c) Outline the specific nursing care given to a patient with tractions.
d) Formulate 5 actual nursing diagnoses for a patient with tractions.
e) Outline the likely complications of the patient on traction.
- a) Outline the indications of underwater seal drainage.
b) Give the specific nursing care for a patient on underwater seal drainage.
c) Formulate four nursing diagnoses for a patient on underwater seal drainage.
d) List the complications of underwater seal drainage.
- a) Outline 6 indications of gastric lavage.
b) Define colostomy.
c) Formulate 4 actual nursing diagnoses and 4 potential nursing diagnoses for a patient with colostomy.
d) Give the specific nursing care to the patient with colostomy.
- a) List the indications of Glasgow coma scale.
b) Describe the Glasgow coma scale.
ANATOMY AND PHYSIOLOGY II
- a) With illustration, describe the formation of flow of CSF.
b) List the functions of CSF.
c) Describe the meninges covering the brain and spinal cord.
- a) Describe the position and gross structure of the parathyroid glands. Outline the functions of parathyroid hormone and calcitonin.
b) Explain the disorders of the thyroid gland.
- a) Describe the structure of a nephron.
b) Explain the processes involved in the formation of urine.
c) Describe how body water and electrolyte balance is maintained.
- a) Describe the structure of the ear.
b) Explain the physiology of hearing.
c) Explain the functions of the accessory organs of the eye.
- a) Explain the role of lymphatic vessels in the spread of infections and malignant disease.
- a) Describe the location of the pharynx and relate it’s structure to it’s function.
b) List the functions of the trachea in respiration.
c) Explain the main mechanisms by which respiration is controlled.
d) Describe the common inflammatory and infectious disorders of the upper respiratory tract.
- a) Define a neuron.
b) Outline the 12 cranial nerves of the nervous system.
c) Describe the transmission of an impulse across a synapse.
PALLIATIVE CARE NURSING
150 a) Define palliative care
b) Explain the principles of palliative care
c) Give the challenges faced in implementing in palliative care services in Uganda
151.a) Define pain according to WHO
b) Explain different types of pain in palliative care
c) Describe the principles of pain management in palliative care
d) Describe the steps of breaking bad news
152.a) Explain 6 roles of palliative care in Uganda
b) Outline 6 symptoms commonly experienced by terminary ill patients
153.a) What is grief?
b) Explain 5 stages of grief experienced by palliative care patients
c) Explain the HOPE approach to spiritual pain management
d) Outline the spiritual problems experienced by palliative care patients