Normal Pregnancy
Normal Pregnancy refers to growth and development of a fertilized ovum and begins from when the ovum is fertilized until the fetus is expelled from the uterus.
Normally the fetus is expelled at term or 9 months or 40 weeks or 280 days.
If the fetus is expelled before 28 weeks, it is called an abortion and if fetus is expelled after 28
weeks but before 37weeks it’s called premature labour and if born after 42 weeks, the post- mature is used.
Pregnancy is said to be normal when;
- The fertilized ovum is growing in the cavity of the uterus.
- One fetus is forming, one placenta and two membranes.
- There is about 1000-1500ml of liquor amnii.
- There is vertex presentation.
- There is no bleeding until show in first stage of labour.
- The mother should remain healthy with no serious disorders of pregnancy.
SIGNS AND SYMPTOMS OF PREGNANCY
When a woman misses a period or two, she may suspect pregnancy and in most cases she is 98% correct if she has been menstruating regularly.
Signs of pregnancy are divided into 3 groups.
- Presumptive
- Probable
- Positive
Presumptive signs
1. Amenorrhea; This is absence of menstruation. Mother may give a history of missing a period or two.
Amenorrhea may also be due to;- use of contraceptives, change of environment, long term illness and emotional upsets.
2. Breast changes; Mother may feel tingling and prickling sensations, breast enlargement and tenderness.
3. Morning sickness(nausea and vomiting); Occurs to 30-50% of the cases, it usually occurs from 4 th -14 th week of pregnancy. Other conditions may give raise to nausea and vomiting but vomiting in conjunction with amenorrhea is suggestive of pregnancy.(may disappear at end of first trimester).
4. Frequency of micturition; Caused by pressure of growing uterus on the bladder usually before 12weeks and decreases when
the uterus rises out of the pelvis at 12 weeks.
5. Skin changes; –
– Striae gravidurum appears on the 16 th week on the abdomen, thighs and breasts.
-Chloasma(mask of pregnancy).
-Linea nigra darkens and can be found below and above the umbilicus.
-Darkening of primary areolar and formation of secondary areolar.
The hormone responsible for the pigmentation of skin is produced by anterior pituitary gland and
it’s called melamine hormone.
6. Quickening; These are the first fetal movements experienced by the mother usually at 18-20 weeks in a PG
and 16-18 in a multi gravida. This helps a midwife to calculate the weeks of gestation if a mother does not know her dates.
7. Fatigue; due to increased blood production, lower blood sugar levels, and lower BP under the influence of progesterone.
Sleep disturbances and nausea may also contribute
8. Mood changes; Due to physical stress, metabolic changes, fatigue or by hormones progesterone and oestrogen.
Probable signs
1. Hagar’s sign;
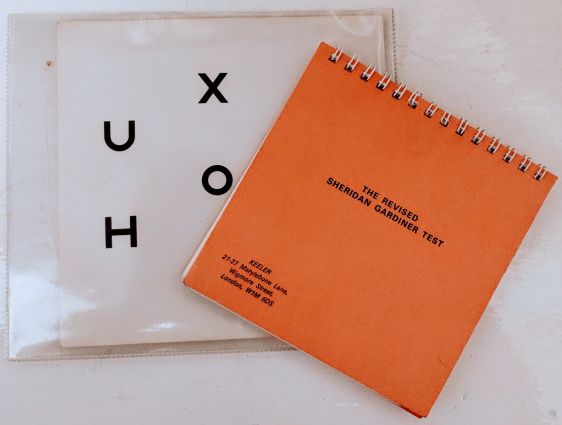
This is detected from 6th -12th week. It is detected by performing a vaginal examination where 2 fingers are inserted into the anterior fornix of the vagina and another hand presses the uterus abdominally, when the fingers of both hands meet, softening if the isthmus is felt.
2. Jacquemier’s sign;
Is the bluish discoloration of the vaginal walls. It takes place from the 8th week onwards and is due to pelvic congestion an indication of pregnancy.
3. Osiander’s sign;
Its increased pulsation felt on the lateral vaginal fornices due to increased vascularity detected from the 8th week onwards.
4. Softening of the cervix (goodel’s sign)
This happens from the 8 th week onwards. The cervix of a pregnant woman is as soft as the lower lip and in a non- pregnant state is as soft as a tip of the nose.
5. Uterine soufflé;
This is a soft blowing sound heard on auscultation. It usually occurs from the 16th week due to increased vascularity of the uterus.
6. Abdominal enlargement;
The uterus enlarges rapidly and progressively from the 16 th week. This excludes gaseous distension, full bladder, fibroids and ascites.
7. Braxton hick’s contractions;
These are painless contractions which usually occur from the 16th week and are felt on abdominal palpation every 15 minutes.
8. Internal ballottement;
The uterus is given a sharp tap just above the cervix which causes the fetus to float upwards in amniotic fluid. The fetus sinks back again and it is felt by the fingers fixed in the vagina. Its detected from 16th-28th week of pregnancy.
9. Presence of HCG(Human chorionic gonadotrophin);
It can be detected in blood for 9 days and in urine 14 days. HCG can be detected in conditions like hydatid form mole.
Positive signs.
Those are signs that are definitely confirmed as pregnancy. They include;-
1. Fetal heart sounds; fetal heart begins beating by the 24th week following conception. It is audible with a Doppler by 10weeks and with a fetoscope by 24weeks. It should not be confused with uterine soufflé from pulsating fetal arteries. The normal fetal heart rate is 120-160 beats per minute.
2. Ultra sound scanning of the fetus; the gestation sac can be seen and photographed. An embryo as early as the 4th week can be identified. The fetal parts begin to appear by the 10th week of gestation.
3. Palpation of the entire fetus; Palpation must include fetal head, back, upper and lower body parts.
4. Palpation of fetal movement; this is done by a trained examiner. It is elicited after 24weeks of gestation.
5. X-ray; It will identify the entire fetal skeleton by the 12 th week. In utero the fetus receives total body radiation that may lead to genetic or gonadal alterations .An x-ray is not a recommended test for identifying pregnancy.
6. Actual delivery of the baby.
DIFFERENTIAL DIAGNOSIS
Enlargement of the abdomen may be caused by other conditions other than pregnancy, these
include;-
- Ovarian cysts.
They may cause abdominal enlargement and when palpated abdominally, the swelling can be separated from the uterus and pregnancy tests will be negative. - Fibroids.
These may be mistaken for pregnancy and normally a hard mass is felt and when pregnancy tests are done, results are negative. - Distended urinary bladder.
In case of urine retention, the catheter will be passed and there will be no other signs of
pregnancy. - Pseudocyesis. In this condition, amenorrhea and other signs suggesting pregnancy will be given by a mother who is anxious to have a baby. When examination is carried out, signs of pregnancy are absent.
PHYSIOLOGY OF PREGNANCY
These are normal natural changes that occur in the body due to pregnancy. These result mainly from alteration of hormones and metabolism.
CHANGES IN THE ENDOCRINE SYSTEM
- Hormonal changes:
The placenta produces several hormones which cause a number of physiological changes.
Successful physiological adaptation of pregnancy is due to alterations in hormone production by
the maternal endocrine system and the trophoblast. - Human chorionic gonadotrophic hormone.
It is produced by the trophoblast. H.C.G levels increase rapidly in early pregnancy, maximum
levels being attained at 8-10 weeksof gestation. The main function of HCG is to maintain the
corpus luteum in order to ensure secretion of progesterone and Oestrogen until placental
production is adequate after 10-12 weeks after which concentration of HCG gradually decreases
until it has completely disappeared 2 weeks after birth. - Progesterone hormone;
This is produced mainly in the corpus luteum. Its function is to thicken the decidua in order to
receive a fertilized ovum. It helps to increase the glandular tissue, ducts of the breasts and muscle
fibres of the uterus. - Oestrogen;
It causes growth of the uterus and duct system of the breasts in pregnancy. It is excreted in urine
and amount present indicates fetal wellbeing. - Relaxin hormone;
During the last weeks of pregnancy, it acts on ligaments and joints producing the “give” of the pelvis. It is also produced by decidua and the trophoblast to promote myometrium relaxation and
may play a role in cervical ripening and rapture of membranes. - HPL ( human placental lactogen): It stimulates the growth of breasts and has lactogenic properties that affect a number of metabolic changes. These changes brought about by HPL ensure that glucose is readily available for body and brain growth in the developing fetus, and protects against nutritional deficiencies.
- Pituitary hormones: The follicle stimulating hormone and L.H are suppressed by the high levels of Oestrogen and progesterone. The adrenal gland increases only slightly in size during pregnancy due to hypertrophy and widening in glucocorticoid area which suggests increased secretion of hormones.
- Thyroid function: In normal pregnancy, the thyroid gland increases due to hyperplasia of glandular tissue and increased vascularity. There is normally an increased uptake of iodine during pregnancy which may be to compensate for renal clearance of iodine leading to reduced level of plasma iodine.
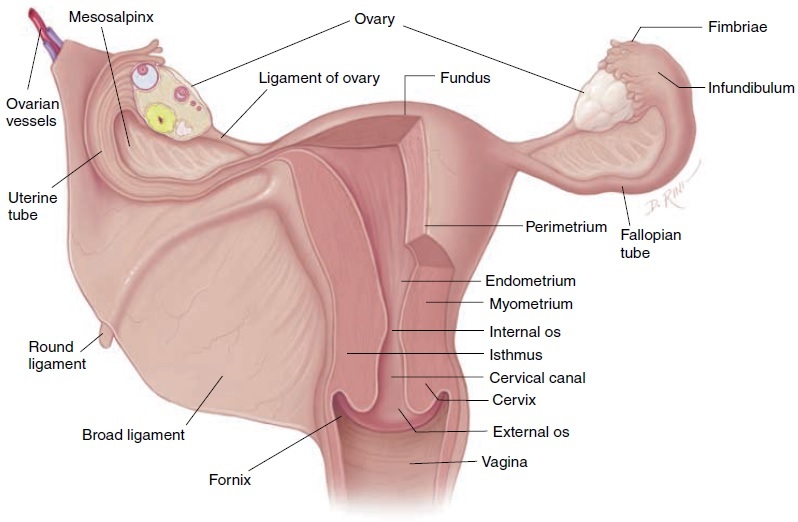
CHANGES IN THE REPRODUCTIVE SYSTEM
CHANGES IN THE UTERUS:
It stretches and expands to accommodate and nurture the growing fetus. This occurs in the
myometrium. The body grows to provide a nutritive and protective environment in which the fetus will develop and grow.
Uterine muscle layers;
1. Endometrium;
– Menstruation stops.
-It becomes the decidua during pregnancy.
-It becomes thick, soft, spongy and readily supplied with blood.
2 . Myometrium.
- The enlargement of the body of the uterus is due to 2 factors.
1. The actual muscle fibres enlarge increasing in length about 10 times and in width about 3 times.
This process is called hypertrophy (increase in size).
2. The new muscle cells make their appearance and grow alongside the original muscle cells. This process is called hyperplasia (increase in number).
The size; as pregnancy advances, the uterus grows from its normal size. The length being 7.5cm,
width 5cm and thickness 2.5cm. So it becomes 30cm in length, 23cm in width and 20 cm in
thickness. The weight increases from 60g to 960g.
The shape; Health growth of the uterus requires adequate space to accommodate the growing fetus, increasing amount of liquor and placental tissue. After conception, the uterus enlarges
because of Oestrogen. At the beginning of pregnancy, it is pear shaped organ, at the end of 12 weeks, it is globular, from 12-38weeks its oval shaped and when lightening takes place after 38weeks, it turns back to globular.
Muscle layers of the myometrium;
- Outer most longitudinal layer,
This layer begins in the anterior wall of the upper uterine segment, passes over the fundus and down the posterior wall. It is by contraction and retraction of this muscle layer that the fetus is expelled from the uterus during labour. - Middle oblique layer,
In this case, muscles are arranged in criss cross manner; the muscle cells surround the blood vessels in the figure of 8 pattern. After separation and expulsion of the placenta, they compress the blood vessels and help to prevent PPH. They are sometimes referred to as living ligatures. - Inner circular layer,
This is the weakest of the 3 layers, the muscle fibres pass transversely around the uterus. They are more developed around the cervix, lower uterine segment and the fallopian tubes. They help in cervical dilatation.
3. The perimetrium;
This is the layer of the peritoneum which does not totally cover the uterus, its deflexed over the bladder anteriorly to form the utero vesicle pouch and posteriorly forming pouch of Douglas. After 12 weeks, the uterus rises out of pelvis and becomes an abdominal organ. It loses its ante-version and ante flexed position and becomes erect and leans on its axis on the right.
CLINICAL OBSERVATIONS OF THE GROWING UTERUS
- At 12 weeks
The uterus is out of the pelvis and becomes upright; it is no longer anteverted and ante flexed. The uterus is palpable just above the symphysis pubis and is about the size of a grape fruit.
- At 16 weeks
Between 12 and 16 weeks, the fundus becomes dome shaped. As it rises, it rotates to the right (dextrorotation) due to the recto sigmoid colon in the left side of the pelvis and exerts tension on the broad and round ligaments.
The conceptus has grown enough to put pressure on the isthmus causing it to open out so that the uterus becomes more globular in shape.
- At 20 weeks
The fundus of the uterus may be palpated at the level of the umbilicus. The uterus becomes more rounded around the fundus.
- At 30 weeks
The fundus may be palpated midway between the umbilicus and ximphoid sternum. Enlarging uterus displaces the intestines laterally and superiorly. Abdominal wall supports the uterus and maintains the relationship btn the long axis of the uterus and axis of the pelvic inlet.
In supine position, the uterus falls back to the vertebral column, aorta and inferior venacava.
- At 36 weeks
By the end of 36 weeks, the enlarged uterus fills the abdominal cavity. The fundus is at the tip of the ximphoid cartilage.
- At 38 weeks
Between 38 and 40 weeks, there is increase in smoothening and softening of the lower uterine segment. Uterus becomes more rounded with a decrease in fundal height. The reduction in fundal height is known as lightening.
Changes in blood supply: The uterine blood vessels increase in diameter and new vessels develop under the influence of Oestrogen. Blood supply to the uterine and ovarian arteries increases to about 750ml/ min at term to keep pace with its growth and meet the needs of the functioning placenta.
Changes in the fallopian tubes: On either side are more stretched out and are more vascular in pregnancy. Uterine end of the tube is usually closed and fimbriated end remains open.
Changes in the isthmus;
It softens and elongates from 7mm to23mm and forms the lower uterine segment during late pregnancy.
Changes in the ovaries:
The follicle- stimulating hormone {FSH} ceases its activity due to the increased levels of estrogen and progesterone secreted by the ovaries and corpus luteum .This prevents ovulation and menstruation. As the uterus enlarges, the ovaries are raised out of the pelvis. Also both ovaries are enlarged due to increased vascularity and become edematous particularly that containing the corpus luteum.
The corpus luteum enlarges during early pregnancy and may even form a cyst on the ovary. The corpus luteum produces progesterone to help maintain the lining of the endometrium in early pregnancy. It functions until about the 10th and 12th week of pregnancy when the placenta is capable of producing adequate amounts of progesterone and estrogen. It slowly decreases in size and function after the 10th to 12th week.
Changes in the cervix:
It remains tightly closed during pregnancy, providing protection to the fetus and resistance to pressure from above when the woman is in standing position. There is slight growth on the cervix during pregnancy, it becomes softer and this is due to increased vascularity and relaxing effects of hormones.
Under the influence of progesterone racemose glands secrete thicker and more viscous mucus which fills the cervical canal and prevents entry of infection in the uterus. The plug of mucous is called opeculum
Towards the end of pregnancy or at the onset of labour the cervix becomes part of the lower
uterine segment, this is called effacement of the cervix. The external os of the cervix also admits a finger. A short softened cervix or os which admits the
tip of a figure at term is referred to as ripe cervix.
Changes in the vagina:
The muscle layer hypertrophies and capacity of vagina increases and it becomes more elastic
allowing it to dilate during 2 nd stage.
The epithelium becomes thicker with increased desquamation of the superficial cells which
increase the amount of normal white virginal discharge known as leucorrhea. The epithelial cells have high glycogen content. The cells interact with Do-derlein’s bacillus and produce a more acidic environment providing extra degree of protection against some organism and increasing susceptibility to others such as candida albicans. The vagina is more vascular and appears violet in colour.
Changes in the vulva:
The vulva appears bluish in colour due to increased vascularity and pelvic congestion.
Breast changes:
-In early pregnancy, breasts may feel full or tingle and increase in size as pregnancy progresses.
-The nipples become more erectile.
– The areolar of the nipples darken and the diameter increases.
– The sebaceous glands become the Montgomery’s tubercles which enlarge and tend to
protrude.They secrete sebum to lubricate the breast throughout pregnancy and breast feeding.
– The surface vessels of the breast become visible due to increased circulation and turns to bluish
tint on the breasts.
-A little clear, sticky fluid(colostrum) may be expressed from the nipples after the 1 st trimester
which later becomes yellowish in colour.
Changes in the cardiovascular system:
The heart
Due to increased work load, the heart hypertrophies particularly in the left ventricle. The uterus pushes the heart upwards and to the left. Heart sounds are changed and murmurs are common.
The cardiac output is increased by 40%. The heart rate increases by an average of 15 beats per minute. The stroke volume increases from 64 to about 71mls.
Effect on blood pressure
During the first trimester, blood pressure remains almost constant. BP drops in 2 nd trimester due to hormone progesterone which causes vasodilation. It reaches its lowest level at 16-20 weeks and towards term, it returns to the level of the first trimester. The decrease may lead to fainting.
Supine position should be avoided in pregnancy as it leads to supine hypotensive syndrome due to compression of the inferior venacava thus reducing venous return. Poor venous return in late pregnancy may lead to oedema in lower limbs, varicose veins and hemorrhoids.
Blood flow
Blood flow increases to uterus, kidneys, breasts and skin but not to liver and brain. Utero
placental blood flow increases by 10-15% about 75mls per minute at term. Renal blood flow increases by 70-80%.
Blood volume
Increase in blood volume varies according to the size of the woman, number of pregnancies she has had, parity and whether the pregnancy is singleton or multiple.
The total blood volume increases steadily from early pregnancy to reach a maximum of 35 to 45% above the non- pregnant level. A higher circulating volume is required for the following;
-To provide extra blood flow for placental circulation.
-To supply the extra metabolic needs of the fetus.
-To provide extra perfusion of kidneys and other organs.
-To compensate for blood loss at delivery.
-To counterbalance the effects of increased venous and arterial capacity.
Plasma volume
Increases by 40% where the red cell mass decreases by 20%leading to haemodilution (physiological anaemia). These changes begin at 6-8weeks of pregnancy. The acceptable Hb level in pregnancy is 11-12g/dl.
Iron metabolism
Iron of about 1000g is needed. 500g is to increase the red cell mass, 300g to fetus and 200g for daily iron compensation.
In normal pregnancy, only 20% of ingested iron is absorbed. The purpose of iron supplementation is to prevent iron deficiency anaemia not to raise Hb level.
Plasma protein
During the 1st 20 weeks of pregnancy, plasma protein concentration reduces due to increased plasma volume. This leads to lowered osmotic pressure leading to oedema of lower limbs seen in late pregnancy. In absence of disease, moderate oedema is termed as physiological oedema.
Clotting factors
Fibrinogen 7,8,9 and 10 increase leading to a change in coagulation time from 12 to 8 minutes.
The capacity of clotting is increased in preparation to prevent PPH after separation of the placenta.
White blood cells.
These are slightly increased during pregnancy, from 700mm to 10500mm during pregnancy and up to 1600mm during labour. The total count cells rises from 8 weeks and reaches a peak at 30 weeks of gestation. This is mainly because of the increase in the number of neutrophils, polymorphs, nucleus, leucocytes, monocytes and granulocytes are active and efficient phagocytes.
Erythrocytes.
They decrease during pregnancy from 4.5million to 3.7million.
HB.
HB concentration falls from 14g/dl; a falling HB is a physiological. The total iron requirements of pregnancy where as a high HB level can be assign of pathology. The total requirements of
pregnancy is averagely 1000g ,about 500gare required to increase the red cells mass and about 300g are transported to the fetus mainly in the last weeks of pregnancy . The remaining 200g are needed to compensate for insensible loss in skin, stool and urine.
RESPIRATORY SYSTEM.
The basal metabolism rate is increased and the volume of air which enters and leaves the lungs during the normal respiration becomes slightly increased. This is because of increased oxygen consumption by the fetus and the work of maternal heart and lungs.
In the late pregnancy the ribs flare out inhibiting the capacity of the thoracic cavity to expand, the enlarging uterus elevates the diaphragm up wards and compresses the lower lobes of the lungs
CHANGES IN THE URINARY SYSTEM
Renal blood flow and glomerular filtration rate increases by 50%.
There is frequency of micturition in early and late pregnancy. Ureters become elongated and kinked due to progesterone hormone and this results into urine stagnation hence increased favor to UTI in pregnancy.
CHANGES IN THE GIT
-The gums become edematous, soft and spongy and may bleed.
-Increased salivation(ptyalism) is common.
-Nausea and vomiting is common in 70% of the cases.
-Changes in taste becoming metallic.
-Craving for abnormal things like soil or plaster known as pica.
-Increased appetite in most women.
-Heart burn due to of stomach content from decreased space by growing uterus.
-There is reduced GIT motility leading to constipation.
Changes in metabolism
– There is increased metabolism to provide nutrients for the mother and fetus.
-Maternal weight, There is continuing weight increase in pregnancy which is an indication of
fetal growth.
Weight gain in pregnancy is as follows;-
4kg in the 1 st 20 weeks(0.2kg/week)
8.5kg in the last 20 weeks(0.4kg/week)
12.5kg approximate total.
Maternal weight gain
Content weight
Uterus 1kg
Breasts 0.4kg
Fat 3.5kg
Blood volume 1.5kg
Extra cellular fluid 1.5kg
Total7.9kg
Fetal weight gain
Fetus 3.4kg
Placenta 0.6kg
Amniotic fluid 0.6kg
Total4.6kg
GRAND TOTAL12.5kg
The following factors influence weight gain.
Maternal oedema.
Maternal metabolic rate.
Dietary intake.
Vomiting or diarrhea.
Amount of amniotic fluid.
Size of the fetus.
CHANGES IN THE MUSCULO-SKELETAL SYSTEM
Progesterone and Relaxin lead to relaxation of pelvic ligaments, joints and muscles. The relaxation allows the pelvis to increase its capacity in readiness to accommodate the presenting part towards term and also during labour. The symphysis pubis and sacroiliac joints soften, the gait of the mother changes as the balance of the body is altered by the weight of the
uterus. Allowing the pelvis to increase its capacity towards term is a process known as a give.
SKIN CHANGES
Increased activity of melanin-stimulating hormone from the pituitary causes varying degrees of pigmentation in pregnant women from the end of 2 nd month until term.The areas that are commonly affected are; areolar of the breasts, abdominal mid line, perineum and axilla. This is because of increased sensitivity of the melanocytes to the hormone or because of greater number of melanocytes in these areas.
-Linea nigra. This is a dark line that runs from the umbilicus to the symphysis pubis and may
extend as high as the sternum. It is hormone induced pigmentation. After delivery, the line begins to fade though it may not ever completely disappear.
-Mask of pregnancy(Cloasma). This is the brownish hyper pigmentation of the skin over the face, fore head, nose, cheeks and neck. It gives a bronze look especially in black complexioned
women.
-Striae gravidurum(stretch marks).
-Sweat glands. Activity of the sweat glands usually increases throughout the body which causes the woman to perspire more profusely during pregnancy.
– A rise in body temperature of 0.5 and increase in blood supply causes vasodilation and makes
woman feel hotter.
MINOR DISORDERS OF PREGNANCY
These are referred to as minor because they are not life threatening.
The causes can be;-
- Hormonal changes
- Accommodation changes
- Metabolic changes and
- Postural changes
DIGESTIVE SYSTEM
Nausea and vomiting (morning sickness)
This is due to hormonal changes progesterone and Oestrogen and high level of HCG, it occurs from 4-16 weeks. This decreases when the placenta fully takes over.
Management
-Light snacks
-Carbohydratesnack like cassava, a hard crackers
-Avoid sweet things
-Coming out of the bed slowly.
Heart burn
Burning sensation in the media sternal region progesterone relaxes the cardiac sphincter and allows reflux of gastric contents into esophagus most troublesome between 30-40 weeks, because of pressure on stomach from growing uterus.
Management
-Avoid bending
-Small frequent meals
-Sleeping with more pillows
-Persistent heart burn antiacids like magnesium triscilicate.
Excessive salivation (ptyalism)
From 8 weeks, hormones are thought to be the cause. It may accompany heart burn. Counseling is helpful.
Constipation
Progesterone cause relaxation of the plain muscles and decreased peristalsis of the gut.
Management
-Increased intake of water, fresh fruit, vegetables and whole meal foods in diet.
-Glass of warm water in the morning, before tea and breakfast may activate the gut.
– Exercise can be helpful especially walking.
Aperients are only considered as a last resort.
Pica
This is when a mother craves for certain foods or unnatural substances.
The cause is unknown but hormones and changes in metabolism are attributed to it.
MUSCULO SKELETAL SYSTEM
This can be due to hormones Relaxin. Discuss with woman and let her be aware, it will
disappear after delivery.
Leg cramps
Cause of leg cramp in pregnancy is unknown may be due to ischemia or a result from changes in PH or electrolyte status.
Management
-Mother to dorsiflex the foot and raise foot of bed.
-Gentle leg movement before sleeping at night.
-Others-use of vit B complements and calcium.
Backache
The weight of the pregnant uterus and altered posture increase susceptibility which is exacerbated by progesterone and Relaxin causing relaxation and softening of ligaments of the pelvis.
Management
-Avoid high heeled shoes.
-Sit on a comfortable chair or support the back on a wall while seated.
-Have extra rest during the day.
CIRCULATORY SYSTEM
Fainting
In early pregnancy, it may occur due to vasodilation under the influence of progesterone before there has been a compensatory increase in the blood volume.
Management
-Avoid long standing periods.
-Quickly sit or lie down if feels slightly faint,
-Mother should avoid lying on her back except during abdominal examination.
Vericose veins
-Progesterone relaxes smooth muscles of veins and results in sluggish circulation. Varicose veins
may occur in legs, anus and vulva.
Management
During pregnancy
-Support tights increase comfort eg stockings.
-Avoid constipation.
-A sanitary pad may give support.
-Use a crepe bandage on affected leg from below upwards before getting out of bed in the
morning and remove it at night.
-The affected leg should be elevated when resting.
-advise mother to see the doctor if varicose veins appear on the vulva.
-In case of severity, book mother for hospital deliverysince they can easily rapture and cause
severe bleeding.
During labour
-Inform doctor.
-Take off blood for Hb, grouping and x-matching.
-Be careful when shaving the vulva and when performing an episiotomy.
-Sedatives are given to prevent premature pushing.
Hemorrhoids
These are veins of the vulva or rectum and they usually occur due to constipation. They can be painful, edematous and ulcerative.
Management
-Advise mother on diet to avoid constipation.
-Use cold compress gently on the area.
-Doctor may order analgesic like anusol.
Heart palpitations
This occurs due to increased functioning of the heart to meet the demands of the growing fetus
and mother.
NERVOUS SYSTEM
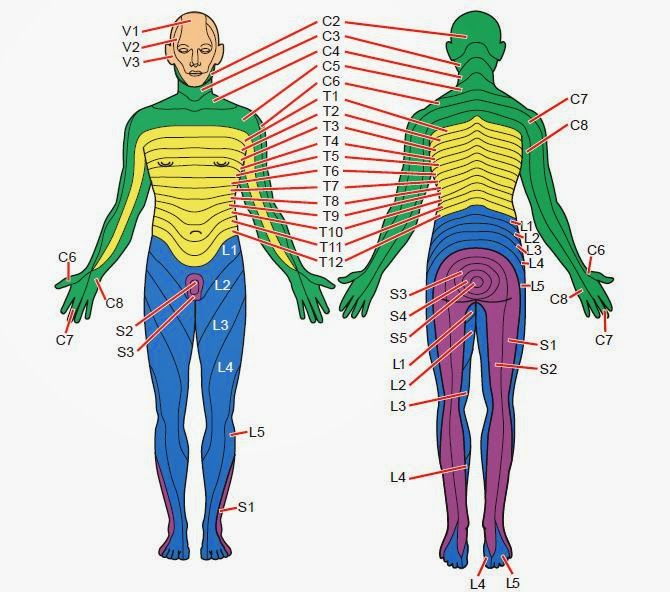
Carpal tunnel syndrome
The mother complains of numbness, pins and needles in her fingers and hands.
It’s caused by fluid retention which causes oedema and pressure on the median nerve by compressing it.
Management
-Wearing a splint at night and rising hands on a pillow at night.
-If it persists, refer to doctor who will give diuretics.
Insomnia
This is failure to get sleep and may be caused by worries, anxietyand it shouldn’t be taken
lightly.
Emotional instability
Hating, irritation,loving i.e. willing to stay closer to partner.
GENITAL URINARY SYSTEM
Leucorrhoea
This is increased, non- irritant, vaginal discharge.
Management
-Ensure hygiene if distressing.
-Wear cotton under pants for easy absorption.
Frequency of micturition
This occurs in early pregnancy when the growing fetus is still in the pelvic cavity and late pregnancy when the PP descends and competes for space needed by bladder.
INTEGUMENTARY SYSTEM
Itching of the skin
This can be due to Striae gravidurum, poor hygiene, heat rash and minor skin rashes.
Management
-Wear cotton clothes which are non-irritating.
-Advise on personal hygiene.
-Apply calamine lotion in case of skin rash.
Disorders which require immediate action
- Vaginal bleeding.
- Reduced fetal movements.
- Frontal or recurrent headache.
- Sudden swelling or oedema.
- Early rapture of membranes.
- Premature onset of contractions
- Maternal exhaustion at whatever extent.
- Fits.
- Excessive nausea and vomiting.
- Epigastric pain.